Clogged tear duct
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.If the tear duct is blocked (also known as tear duct stenosis, lacrimal duct stenosis or dacryostenosis), the tear duct through which the tear fluid flows is blocked. As a result, the eye begins to water more. This often occurs in babies (e.g. due to a congenital malformation). But adults are also affected (e.g. through infections, injuries). Find out here how a blocked tear duct can develop and what you can do about it!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Q10

Brief overview
- Treatment: The doctor initially treats conservatively (without surgery), e.g. with a tear sac massage, antibiotic eye drops, eye rinsing. If there is no improvement, an operation is usually necessary.
- Causes: A blocked tear duct is either acquired (e.g. due to infection or injury) or congenital (e.g. due to malformation).
- Description: Clogged or narrowed tear duct through which the tear fluid can no longer flow freely.
- Symptoms: Watery and red eyes, recurring eye inflammation, pain and swelling in the inner corner of the eye, blurred vision
- Diagnosis: Conversation with the doctor, examination of the eye, if necessary ultrasound, X-ray Course: Usually easy to treat. In severe cases, abscesses under the eyes and inflammation of the surrounding tissue occur.
- Course: Generally easy to treat. In severe cases, abscesses under the eyes and inflammation of the surrounding tissue occur.
What can you do about a blocked tear duct?
Treatment will depend on what is causing the blockage in the tear duct. Ophthalmologists recommend treating the blocked tear duct initially without major interventions and as gently as possible. If this does not bring the desired result, an operation is usually necessary.
Non-surgical treatment
At the beginning, the doctor tries to treat a blocked tear duct without surgery (conservative). He is as careful as possible to avoid further injuries to the eye. In the case of babies in particular, it is important that the treatment is as gentle as possible. Because even the smallest injuries can lead to scarring in the area of the tear and nasal duct.
When it comes to babies, wait and see
In babies it can happen that the so-called "Hasner membrane" does not recede by itself after birth, as it normally does. The "Hasner membrane" is a membrane that closes the transition from the tear ducts to the child's nose during pregnancy.
If the membrane does not recede, the tear-nasal duct remains closed or severely narrowed. As a result, the tears cannot flow down the nose, they back up and finally run over the edge of the eyelid.
Since it is possible that the thin skin membrane in babies' tear ducts will loosen spontaneously in the course of the first few months of life, doctors recommend waiting for the time being. In the meantime, it often helps to clean the child's eyes with lukewarm water (not too warm!) If pus settles in the eyelids.
Lacrimal sac massage
In some cases, bagging the eyes can also help open the tear ducts. To do this, massage the area of the eye sac with stroking movements from the inner corner of the eyelid to the nose with the fingertips. By applying gentle pressure to the tear sac, one tries to use the jammed fluid to try to “burst” the membranous seal.
Ideally, ten of these massage movements should be performed four times a day. As soon as the tears and nasal passages are open, the doctor usually prescribes nose and eye drops. They have a decongestant effect and slow down the release of mucous membrane secretions in the tear duct.
Let an ophthalmologist or pediatrician show you the massage technique beforehand!
Home remedies
Home remedies such as warm compresses should also help to alleviate the symptoms of a blocked tear duct. The best way to do this is to take a hygienically clean cloth (or sterile gauze) and briefly put it in warm (not too hot!) Water. To make the water sterile, it is best to boil it briefly beforehand. Then place the cloth over the eyes (or just over one affected side) for about twenty minutes.
Home remedies alone are not recommended to treat a blocked tear duct. Let a doctor clarify the complaints beforehand!
The warmth of the compress promotes blood circulation and, if necessary, helps to widen the tear duct a little. Warm or cold infusions made from marigold flowers, black tea or oak bark are also suitable for eye compresses. Ask your doctor or pharmacist.
Use medicinal herbs from the pharmacy and not from your own garden for the compresses.
An eye rinse (eye shower) from the pharmacy can also help with irritated eyes (e.g. due to foreign objects such as small stones). It usually contains sterile saline that corresponds to the natural salt content of the eyes.
To do this, tilt your head slightly back and hold the upper and lower eyelids apart with your fingers. With the other hand, place the eyewash bottle close to the eye so that the rinse runs directly into the eye. Rinse the eye until the eye wash bottle is empty and then discard it.
Do not use tap water to wash your eyes. This also increases the risk of infection.
In some cases, rinsing the nose with a saline solution can also help. The tear duct ends in the nose, so it is possible that this is also where the cause of the blockage lies. If necessary, this can be removed using a nasal douche.
Only use home remedies after consulting your ophthalmologist and wash your hands thoroughly before each use!
Antibiotic eye drops
In acute infections and signs of bacterial inflammation (e.g. pus in the corner of the eye), the doctor often prescribes antibiotic eye drops. They inhibit the formation of bacteria and thus inflammation. The person concerned (or in the case of babies the parents) put the eye drops into the eyes several times a day for several days. You can find out from your ophthalmologist which dosage is necessary in your individual case.
Always wash your hands thoroughly before using eye drops!
Irrigation of the tear ducts
If the tear duct does not open by itself or by massaging the tear sac, the doctor flushes the draining tear ducts with saline solution. To do this, he uses a special cannula (thin hollow needle), which he carefully inserts into the blocked tear duct.
The rinsing creates an overpressure in the tear and nasal duct, which opens the skin seal. This form of treatment only takes a few minutes. The doctor will numb the affected area locally; general anesthesia is only necessary in rare cases. Such an overpressure flush is successful in up to 90 percent of the cases.
surgery
In severe cases (e.g. injuries) or if the non-drug treatment does not bring the desired result, the doctor will perform an operation on the eye.
Probing the tear ducts
If the irrigation is still unsuccessful, the doctor tries to open the lacrimal duct with a small probe (thin cannula) under general anesthesia. At the same time, it expands (dilation) and flushes the tear duct to loosen any blockages. The procedure usually takes no longer than 30 minutes.
Occasionally it is necessary for him to insert a small inflatable balloon into the tear duct to widen the duct even more (balloon dilatation). In some cases, the doctor will insert a thin plastic tube or thread for three or four months to allow the tear fluid to drain out.
Dacryocystorhinostomy (DCR)
If all previous treatments fail, the doctor performs a so-called dacryocystorhinostomy (also dacryorhinostomy; Toti operation). To do this, he creates a diversion (bypass) or a passage with the help of a thin silicone tube from the tear sac to the nose, through which the tear fluid can drain.
The doctor will leave it there for about three to six months to prevent the tear duct from growing closed again. The procedure is also performed under general anesthesia.
Endonasal lacrimal duct surgery
In some cases, endonasal lacrimal duct surgery is necessary.The doctor removes a piece of the bone lamella between the tear sac and nasal cavity through the nose in order to create a drain-free opening for the tear fluid. As with the dacryocystorhinostomy, the operation is performed under general anesthesia and takes about 30 minutes.
In adults, an operation is often the only way to successfully and permanently remove long-standing blockages in the tear duct. It is only necessary in exceptional cases for babies.
How does a blocked tear duct develop?
A blocked tear duct has several possible causes. This includes:
Incompletely developed nasal tears
The thin membrane that closes the transition from the tear ducts to the child's nose during pregnancy (“Hasner's membrane”) usually recedes by itself shortly before or shortly after the birth.
In five to seven percent of all newborns, the membrane of the tear duct does not open by itself after birth, the tear-nasal duct remains closed or severely narrowed. As a result, the tears cannot drain through the nose, they back up and eventually run over the edge of the eyelid (congenital or connatal tear duct stenosis).
Malformed facial or skull bones can also lead to blocked tear ducts.
Inflammation of the tear ducts
Bacterial infections or inflammations of the nose (e.g. runny nose), the eyes or the tear ducts themselves sometimes cause the tear duct to swell up and block the drainage of the tear fluid (tear duct blockage).
Injuries to the tear ducts
If the tear ducts or surrounding bone areas are injured (e.g. by a blow in the face or an accident), the tear duct can also be obstructed.
Narrowed tear ducts in old age
In the course of the aging process, the tear ducts of some people narrow. This increases the risk of the tear ducts becoming blocked.
Tumors, cysts, stones
Tumors, other pathological growths (e.g. cysts) or small stones that get into the eye can also clog or block the tear ducts.
What is a blocked tear duct?
The lacrimal gland regularly secretes tear fluid in order to moisten the eye evenly with the blink of an eye. In the inner corner of the eye, the excess tear fluid flows through the tear ducts - consisting of tear points, tear ducts and the tear-nasal duct - into the nose.
In the case of a blocked tear duct - also known as lacrimal duct stenosis, lacrimal duct stenosis or dacryostenosis - the duct that connects the eyes to the nose (tear-nasal duct) is narrowed or blocked on one or both sides.
As a result, tear fluid can no longer flow properly, causing the tear fluid to run over the edge of the eyelid (Epiphora) - the eye water.
While lacrimal duct stenosis in adults usually results from inflammation or damage to the lacrimal duct, in children it is predominantly the result of an incompletely developed lacrimal duct. Five to seven percent of all newborns are affected by such a congenital (congenital) tear duct obstruction.
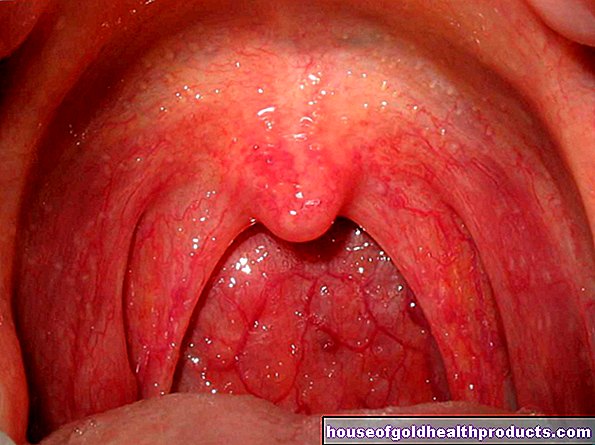
How is a blocked tear duct noticeable?
A blocked tear duct causes a variety of symptoms in both babies and adults. Those affected show the following symptoms, among others:
- The eye is constantly watering (e.g. even when the child is not crying).
- The tears run down the edge of the eyelids or down the cheek.
- The affected person sees blurred.
- The eyes are itchy and reddened (symptoms are similar to those seen with dry eyes).
- Yellowish crusts form on the eyelid skin and in the corner of the eyelid (stuck eyes) due to dried-on tear fluid.
- The skin of the face is irritated and reddened from the tears.
- If the tear duct remains blocked for a long time, the tear sac often becomes inflamed (dacryocystitis). When pressure is applied to the tear sac area, mucus flows out of the tear points (mucus plug).
- The tears appear thicker (tear fluid in the tear sack thickens).
- Recurring, purulent inflammation in the tear sac or conjunctivitis caused by bacterial infections (infections are both a consequence and a cause of a tear duct blockage).
- The affected person has swelling and pain in the inner corner of the eye.
In babies, the first symptoms usually become noticeable in the first few weeks after birth.
What does the doctor?
If the symptoms persist (e.g. watery eyes, pain in the eyes), it is necessary to consult a doctor. The first point of contact is the family doctor. If necessary, he will refer you to an ophthalmologist or ENT doctor for further examinations.
Even if watery eyes initially suggest simple inflammation, it's important to rule out other eye diseases, such as congenital conjunctivitis, a tumor, or glaucoma.
anamnese
The doctor first conducts a detailed discussion with the person concerned (anamnesis). Among other things, he asks questions about the existing symptoms, for example:
- When did the complaints arise?
- Did they arise suddenly or did they develop over a longer period of time?
- Are possible triggers for the complaints (e.g. an injury) known?
Examination of the eye
After the interview, the doctor examines the eyes for visual abnormalities (e.g. increased tears, discoloration). To do this, he takes a closer look at the eyes using a slit lamp and measures the intraocular pressure. If necessary, the doctor will carry out an eye test.
To test whether the tear duct is blocked, he then drips a colored liquid into the eye. If the doctor observes that the colored tear fluid does not run off as usual in the inner corner of the eye or the person affected even tastes the fluid and feels it run down the back of the throat, this provides the first indication of a blocked tear duct.
If there is an inflammation, pus often flows out of the bags when pressure is applied to the corner of the eye.
Further investigations
Ultrasound and X-ray examinations are suitable for further clarification. With the X-ray, the doctor makes the drainage conditions in the tear-nasal duct visible, among other things. To do this, he flushes the tear duct with contrast medium beforehand.
Is a blocked tear duct treatable?
A blocked tear duct is usually treatable. With timely treatment, the symptoms usually disappear within a few days. If, on the other hand, a blocked tear duct is not treated or treated too late, in the worst case scenario a lacrimal sac abscess or a purulent inflammation of the entire surrounding tissue (phlegmon) will develop.
Tags: home remedies eyes skin