Endocarditis
All content is checked by medical journalists.In the case of endocarditis, the inner lining of the heart (endocardium) becomes inflamed and, above all, the heart valves. Endocarditis is usually triggered by a bacterial infection, which must be treated with antibiotics as quickly as possible. Heart inflammation is more rarely caused by another disease (e.g. fungal infection, autoimmune disease). Read more about the causes and treatment of endocarditis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I33I09I01I38I39
Endocarditis: description
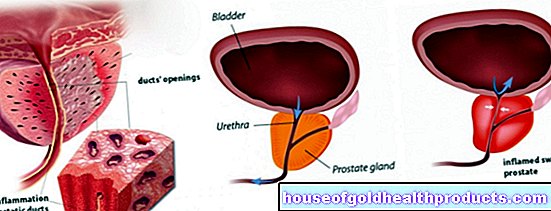
Endocarditis is inflammation of the inner lining of the heart, the so-called endocardium. The heart wall is made up of three different layers - the endocardium is the inner one. It lines the atria and chambers of the heart and also forms the four heart valves. These act as valves for the blood that is pumped through the heart with each beat. In most cases of endocarditis, one or more heart valves are inflamed, usually the mitral valve and / or the aortic valve, and rarely the valves of the right heart.
Usually an infection with bacteria causes the endocarditis, less often fungal infections. There are also non-infectious forms of endocarditis. Here the endocardium becomes inflamed without being colonized by pathogens, for example in the context of rheumatic fever. The non-infectious form of endocarditis is becoming increasingly rare in Western countries, while the infectious form is becoming more common. This is mainly due to the fact that certain heart operations are performed more often today - and these can also be the cause of an infection. Most elderly people develop endocarditis.
There are two types of infectious endocarditis:
- In the acute course, the patient's condition suddenly deteriorates rapidly (endocarditis acute).
- In the subacute form (endocarditis lenta), the signs appear insidious and are therefore often not directly recognized as endocarditis symptoms.
In both cases, it is important that heart inflammation is diagnosed and treated as early as possible in order to avoid severe disease.
Endocarditis: symptoms
The symptoms of endocarditis differ depending on the cause. Acute endocarditis is often caused by staphylococci. It manifests itself with sudden and rapidly progressing symptoms. Above all, these include:
- fever
- chills
- Slump in performance, weakness
- paleness
- Fast heartbeat (tachycardia)
- Muscle and joint pain
- Clouding of consciousness
- Heart and kidney failure up to organ failure
The inflammation creates deposits on the heart valves (thrombotic material + pathogens).Small, also infectious pieces can be detached from this, which can get to other parts of the body via the bloodstream. There they close small vessels (embolism). The tissue in question therefore receives too little oxygen (ischemia) and perishes. Depending on the region of the body, these septic embolisms cause various endocarditis symptoms, such as:
- A so-called septic-embolic herd encephalitis in the central nervous system. Stroke-like symptoms, headaches, neck stiffness or severe drowsiness (somnolence) may occur.
- On the skin, the emboli cause bleeding into the skin. Doctors speak of Janeway lesions (painless bleeding on the soles of the hands and feet) or Osler nodules (painful, nodular bleeding in the fingers and toes). Smallest, punctiform hemorrhages are usually seen on the nails (petechia).
- Infarcts and enlargement of the spleen
- Kidney attacks
- Vascular occlusion in the eye and hemorrhage in the retina
The subacute form (endocarditis lenta) begins insidiously. The typical causative agent of subacute endocarditis is Streptococcus viridans. Those affected often have a low fever for a long period of time. Chills occur occasionally or not at all. Sick people often complain of poor appetite and weight loss. Persistent inflammatory reactions also affect other organs in this endocarditis - mostly through the deposition of proteins in the immune system (immune complexes).
Endocarditis symptoms may be slightly different for non-infectious causes. In rheumatic endocarditis, for example, other signs of rheumatic fever are usually in the foreground - such as joint pain that wanders from one joint to another. People with lupus erythematosus often do not notice for a long time when deposits form on their heart valves (Libman-Sacks endocarditis). Other layers of the heart wall can become inflamed (pericarditis, myocarditis) and cause various symptoms, such as chest pain and a faster heartbeat.
Endocarditis: causes and risk factors
Endocarditis can have a number of causes. Both infectious (bacterial) endocarditis and a non-infectious (abacterial) form are possible.
Infectious endocarditis
In most cases, the triggers for infectious endocarditis are bacteria, especially staphylococci and streptococci, and occasionally enterococci. The most common pathogen is Staphylococcus aureus. Other bacteria and fungi are also possible, but rarely. Fungal infections make up about one percent of endocarditis and mainly affect patients with a severely weakened immune system.
Bacterial endocarditis threatens above all patients with previous damage to the inner lining of the heart, on which the pathogens can settle more easily, for example through:
- a congenital or acquired heart defect (e.g. open ductus arteriosus); unnatural blood turbulence can attack the endocardium and promote infections.
- Operations on the heart, especially when foreign bodies are used; this applies in particular to artificial heart valves, but also to venous catheters and cables from pacemakers.
Endocarditis can also occur when a lot of bacteria are washed into the bloodstream. This can be done through certain operations in the area of the teeth and airways, as well as through an abscess or with drug addicts who use injections.
However, endocarditis does not always have to be a bacterial infection of the inner lining of the heart. Some conditions can also cause non-infectious endocarditis:
Rheumatic endocarditis
Rheumatic endocarditis only develops after a bacterial infection has expired. About one to three weeks after a strep infection (usually in the form of tonsillitis or sore throat), what is known as rheumatic fever can occur. The sick person develops a high fever and various joints become inflamed (wandering polyarthritis). Sometimes nodules and rashes form on the skin (erythema annulare rheumaticum, erythema nodosum).
The heart can also be involved, for example in the form of rheumatic endocarditis. It is still referred to as non-infectious endocarditis, since this inflammation is not caused by the streptococci, but by defense mechanisms of the own immune system, which mistakenly attack the body's own tissue. Doctors call this heart valve inflammation endocarditis verrucosa, in which small, reddish valve deposits form.
Endocarditis in lupus
Endocarditis can also occur in the context of systemic lupus erythematosus, an autoimmune disease from the rheumatic group. This is called Libman Sacks endocarditis. Similar to rheumatic endocarditis, the body's own defenses cause inflammation and deposits on the heart valves (fibrin thrombi).
Other forms of endocarditis
Endocarditis associated with Löffler's syndrome (hypereosinophilic syndrome), an inflammatory disease that usually affects lung tissue, is also rare. In Löffler's endocarditis (also called parietal fibroplastic endocarditis), the inner lining of the heart thickens. Certain immune cells (eosinophilic granulocytes) collect on it. In this form, however, the heart walls are primarily involved.
Carcinoid syndrome, a disease in which a tumor increasingly releases certain messenger substances (especially serotonin), can attack the heart valves and lead to endocardial fibrosis. Thrombotic endocarditis is when other serious illnesses cause blood cells to attach to the heart valve. These diseases include cancer, severe malnutrition or severe kidney weakness with persistently elevated urea.
Endocarditis: examinations and diagnosis
To diagnose endocarditis, the doctor first asks about the medical history (anamnesis). For example, he asks whether the patient is aware of a heart defect and whether an intervention on the heart may have taken place. But other operations (for example at the dentist) can provide important information. This also applies to previous infections, autoimmune diseases and drug use. For example, during a physical exam, doctors measure body temperature and listen to the heart with a stethoscope.
If endocarditis is suspected, an echocardiography (also called ultrasound cardiography - UKG) follows. The heart is examined through the chest with an ultrasound machine. Further examinations will follow if there are abnormalities or the person concerned has an increased risk of endocarditis (for example, patients with artificial heart valves). For example, a heart ultrasound, which is carried out through the esophagus (transesophageal echocardiogram, TEE), provides an even more precise picture of the heart. Therefore, if the TEE does not show any deposits on the valve, endocarditis is very unlikely.
The patient's blood test is also particularly important because it can provide information about the cause. For this purpose, the blood is examined in the laboratory for pathogens that may trigger infectious endocarditis (blood cultures). If the germ is found, it can be specifically treated with the right antibiotic. If the cause of the endocarditis remains unclear, further examinations follow, for example magnetic resonance imaging (MRI) or the removal of a tissue sample from the inner lining of the heart (endocardial biopsy).
If the diagnosis of endocarditis is difficult, doctors sometimes do additional tests, such as computed tomography (CT) or positron emission tomography (PET). So that they can better assess whether there is actually an inflammation of the heart valves, so-called Duke criteria are laid down in the endocarditis guideline. If a certain combination of these criteria is present, endocarditis is considered confirmed.
Endocarditis: treatment
Different specialists - usually cardiologists, microbiologists, infectiologists and cardiac surgeons - decide which endocarditis therapy is right in each individual case. With bacterial endocarditis, the most important measure is rapid and effective antibiotic therapy. The antibiotics are usually given intravenously (i.e. directly into the vein). The doctors adjust the choice of antibiotic as precisely as possible to the causative agent - if a germ is found. With regular blood tests they check how well the therapy is responding.
In about every tenth case, the pathogen cannot be detected (so-called culture-negative endocarditis). Nevertheless, the use of antibiotics is justified even if endocarditis is suspected. Because the patient's life depends on the rapid treatment. In these cases, doctors try a combination of antibiotics that covers almost all pathogens.
Antibiotic therapy is insufficient for about every second patient with infectious endocarditis. An operation is necessary, for example, if the heart valves are severely damaged by the inflammation and there is a risk of heart failure. In such a case, the doctors usually remove the diseased tissue and insert one or more artificial heart valves into the patient.
In the case of non-infectious causes, the most important part of endocarditis therapy is that the underlying disease is treated. Patients with systemic lupus erythematosus, for example, can help with cortisone preparations, which slow down the autoimmune reaction. In rheumatic fever, on the one hand, the streptococci are fought with antibiotics, on the other hand, the defense reaction is dampened with anti-inflammatory drugs. In order to prevent a rheumatic fever, doctors give antibiotics to the previous sore throat or tonsillitis if a rapid streptococcal test is positive.
Endocarditis: prophylaxis
You can find out which measures you can take to prevent endocarditis here.
Endocarditis: disease course and prognosis
The prognosis of endocarditis depends on several factors:
- Time of diagnosis
- Cause of the inflammation of the lining of the heart
- (Pre) damage to the heart
- Age of the patient
- Immune system of the patient
- Chronic previous illnesses (e.g. diabetes mellitus)
- With bacterial endocarditis: sensitivity of the pathogen to antibiotics
Complications that arise when growths or deposits on the endocardium loosen are relatively common in endocarditis. If these "pieces" are washed into the bloodstream, they can block a blood vessel and thus trigger a stroke or embolism.
Today, infectious endocarditis can be successfully treated in around three out of four cases. However, if it is recognized too late or if the person is older and has multiple illnesses, the likelihood of it being fatal increases. Without treatment, endocarditis (almost) always leads to death.
Tags: laboratory values anatomy nourishment