combustion
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.In the event of a burn, the skin is damaged by the effects of heat. Most burns are superficial. In severe cases (burns), intensive medical treatment is necessary. Severe burns can cause reactions throughout the body. Treatment depends on the severity. Find out everything you need to know about incineration here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. T23W87T20T27X19T24T21T22T30T28T31

Combustion: description
A burn is skin damage caused by direct exposure to heat. Contact with hot liquids is called scalding. Hot or heated objects cause so-called contact burns. Chemical accidents can result in chemical burns or chemical burns. Electrical damage is known as electrical burns. UVA, UVB and X-rays cause so-called radiation burns.
Burn frequency
Every year in Europe, millions of people with burns are treated by general practitioners and thousands are treated as inpatients in clinics. Many of them require intensive medical treatment and come to the hospital with burns and chemical burns. 180,000 people worldwide succumb to burn injuries every year.
Typically burns in adults are caused by flames or hot gases (for example, from deflagration after an explosion). On the other hand, scalds occur most frequently in children and the elderly. Burns mostly occur in the home or at work.
Structure of the skin
The outermost layer is the upper skin (epidermis). The superficial horny layer with its protective film of sebum and sweat prevents the penetration of bacteria, fungi and foreign substances. In addition, the epidermis protects the body from drying out. It is easily worn away, but is constantly being reproduced by deeper-lying cells. A slight burn is usually limited to the epidermis. The outermost defense cells of the immune system are located at the border to the dermis underneath.
The dermis (corium, dermis) is located directly under the epidermis. Finely ramified blood vessels, muscle cords and nerves run here. The upper cells of the dermis are more active than the lower ones. Therefore, a superficial sclera burn heals more easily than a deeper one. Underneath is the subcutis, which consists of fatty tissue and is traversed by larger blood vessels and nerves.
Depending on the depth of the burn, burns are divided into four degrees of burn:
1st degree burn
In the case of a first-degree burn, the burn wound is limited to the epidermis, usually only to the superficial horny layer (stratum corneum). She heals without consequences.
Burns: 2nd degree
A 2nd degree burn damages the skin down to the top layer of corium. Read everything you need to know about 2nd degree burns here
3rd degree burns
3rd degree burns damage the entire epidermis and extend into the subcutaneous tissue.
4th degree burn
A burn 4.Grades charred all layers of the skin and often also affects the underlying muscle tissue with bones, tendons and joints.
Burn: symptoms
The symptoms of a burn or scald primarily depend on its depth: the deeper the burn injury, the more the pain sensation is lost. In the case of particularly deep burns, some patients no longer experience pain at all (analgesia) because the nerve endings are burned just like the rest of the skin tissue. The severity of a burn or scald depends not only on the temperature, but also on the duration of exposure.
Blisters form when the epidermis separates from the underlying dermis. The epidermal cells swell and die (vacuolating degeneration). An open burn wounds from leaking fluid from the bloodstream. Dead tissue appears white in the early phase and later turns into black-brown scabs.
In general, severe burns usually affect the entire organism. The dead tissue can lead to kidney failure via certain mechanisms. Due to the loss of body fluids and proteins through the burn injury, the tissue is no longer adequately supplied with blood and oxygen. Patients complain of dizziness or even lose consciousness.
Ultimately, a major burn injury can result in life-threatening shock (burn shock). Typical symptoms include noticeably low blood pressure, a very fast beating heart (rapid heartbeat, tachycardia), cold, pale arms and legs, and metabolic disorders. The decreased blood flow to the organs can eventually lead to their failure.
Depending on the degree of burn, the following symptoms can occur:
|
Degree of combustion |
Symptoms |
|
I. |
Pain, swelling (edema), redness (erythema) |
|
II a |
severe pain, redness, blistering |
|
II b |
little pain, redness, blistering |
|
III |
no pain, skin appears black, white or gray and leathery, irreversible tissue death (necrosis) occurs. |
|
IV |
Body areas completely charred black, no pain |
scalding
Thick (viscous) liquids store heat better and, if scalded, often damage the skin more than water, for example. Usually different degrees of combustion occur at the same time. So-called "runoff marks" are often recognizable.
Inhalation trauma
Breathing in hot gases or air mixtures can also damage the airways. This so-called inhalation trauma usually has an unfavorable effect on the general healing process of the patient. Burns on the head and neck, burnt nose and eyebrow hair and traces of soot in the ear, nose and throat area indicate such damage. Affected people are usually hoarse, find it difficult to breathe and cough up soot.
Electrical incineration
Electrical burns occur when the body is exposed to electrical current, such as lightning strikes. Since the body offers a natural resistance to the current, heat develops - the greater the resistance, the greater the heat development. Because the bones offer great resistance, nearby muscle tissue is usually destroyed. The severity of an electrical burn also depends on the type of current, the current flow and the duration of contact. Usually there is only a small, inconspicuous skin wound where electrical current has entered the body.
Burn: causes and risk factors
Burns and scalds occur when the body is exposed to intense heat. Tissue is destroyed at temperatures above 44 degrees Celsius. With long-term exposure to heat, values above 40 degrees Celsius are sufficient. In addition to the temperature, the duration of the exposure to heat plays a key role in the development of a burn.
Possible causes of a burn or scald are:
- Open fire, flames, explosion: classic combustion
- hot water, steam, oil and other liquids: scalds
- hot metal, plastic, coal, glass: contact burning
- Solvents and cleaning agents, concrete, cement: chemical combustion
- Electric current in the household, high-voltage lines, lightning: electrical incineration
- Sunbathing, solarium, radiation treatments using UV and X-rays: radiation burns
Tissue death
Due to the heat acting on it, the protein in the body's cells coagulates. The cells perish and the surrounding tissue can die (coagulation necrosis). Finally, inflammatory messenger substances (prostaglandins, histamine, bradykinin) and stress hormones are released, which make the blood vessel walls more permeable (increase in permeability). Fluid flows from the bloodstream into the tissue and causes it to swell, known as edema. The leakage of fluid from the blood vessels is highest in the first six to eight hours and can last for up to 24 hours.
Effects on the body
In the course of the formation of edema, the amount of circulating blood (lack of volume, hypovolemia) in the bloodstream decreases. As a result, organs are no longer adequately supplied with blood. Ultimately, kidney failure and intestinal deficiency can lead to cardiovascular failure and death.
Afterburn
Due to the water retention, the tissue around the burn can no longer be adequately supplied with oxygen and further cell damage occurs. Doctors refer to this as "afterburn". Due to the continuous flow of fluid into the tissue, the extent of a burn can usually only be fully assessed after one day.
Burn: diagnosis and examination
A visual diagnosis is usually sufficient for the first assessment of a burn. However, the circumstances in which the burn injury occurred are also important. In addition to questions about your symptoms, your doctor will also ask you questions about how the accident happened:
- How did the burn come about?
- What caused the burn, such as an open fire or a hot object?
- Did the burn occur at home or at work?
- Have you burned yourself in hot water or hot fat, that is, were you scalded?
- Was there hot smoke, toxic gases, or soot in the air around you?
- Do you have pain?
- Are you dizzy or have you lost consciousness for a short time?
Your family doctor or dermatologist (dermatologist) is the right contact for minor burns. Serious burns must be treated by an emergency doctor and then a surgeon.
Physical examination
After the consultation with the patient, the doctor examines the body in detail. In the case of severe burns, for example after a clothing fire, the burn victim is completely undressed. In addition, the doctor will measure blood pressure, pulse and the frequency of breaths and monitor the work of the heart, which can be impaired in particular by electrical accidents. Finally, the doctor will listen to the lungs (auscultation), draw blood and have an X-ray of the lungs made.
Needle sample
To distinguish a 2nd degree burn from a 3rd degree is usually difficult at the beginning and can only be achieved after about 24 hours. The stitch with a needle will help. With a third degree burn, the patient does not feel any pain.
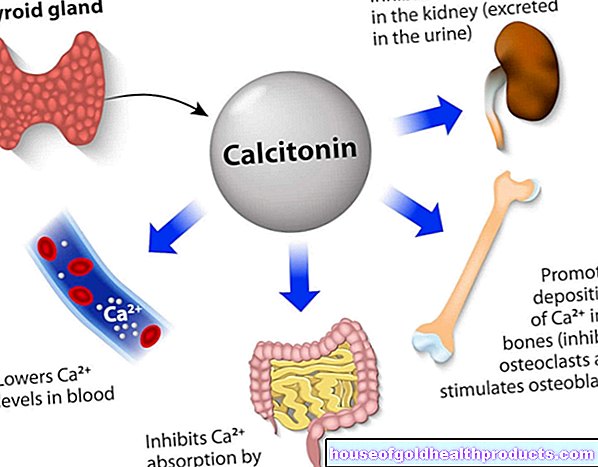
Blood test
Certain blood values provide information about inflammation, blood loss and lack of fluids as well as respiratory function. In the case of an inhalation trauma, there is usually a high proportion of carbon monoxide in the blood, which in particular inhibits the transport of oxygen. In addition, inflammatory messengers (e.g. interleukins IL-1, -2, -8 and tumor necrosis factor alpha) can be detected in the blood in severe burns. Since a burn victim also loses protein through the burn wound, the protein content in the blood is reduced in severe burns. While the sodium content is usually reduced, the potassium content increases due to cell damage.
Bronchoscopy for airway burns
If the airways are burned, the doctor will perform a lungoscopy. Using a flexible, thin tube with a camera at the end, the doctor can make deeper regions visible. In the case of an inhalation trauma, there are traces of soot and whitish-gray areas that indicate the death of cells. Examination of the lung mucus (tracheal secretion) can also indicate a burn if, for example, soot particles are found.
Estimation of the extent of the burn
Especially in the first few days after a major burn, the doctor will closely monitor the progress and carry out some examinations again. In order to assess the extent of a burn, the doctor uses the so-called rule of nine according to Wallace. According to this, the arms each take up nine percent of the body surface, legs, torso and back 18 percent each (two nine percent), head and neck nine percent and the genital area one percent.
According to the palm rule, a patient's palm is roughly one percent of the total body surface.
Both rules are only rough estimates that need to be adjusted especially for small children and infants. For example, the head of an infant makes up 20 percent of the body area, while the torso and back only make up 15 percent each.
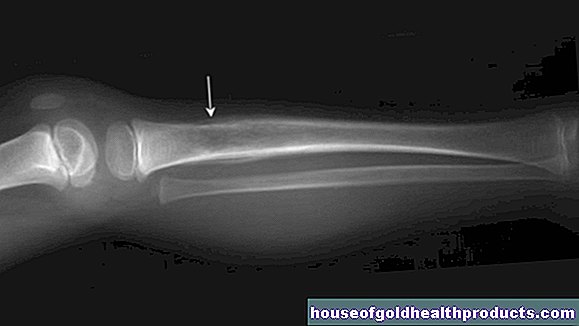
Accompanying injuries
During the physical examination, the doctor pays attention to further injuries such as broken bones or internal bleeding and will arrange further examinations, for example a computed tomography or an ultrasound, if necessary. If the burn wound is suspected of being infected with bacteria, a swab is taken and the exact pathogen is determined. In principle, adequate tetanus vaccination protection is important. After the basic vaccination, a booster vaccination should take place at least every ten years.
Burn: treatment
What to do in case of burns. Read everything you need to know about burn treatment and how you can treat scalds here.
Burn: disease course and prognosis
The healing process in the case of a burn depends primarily on the depth and extent of the burned body surfaces. Pre-existing illnesses, the old age of the person affected and accompanying injuries such as organ damage reduce the chances of recovery. Infants and children are more prone to complications than adults.
A burn becomes life-threatening especially when around 15 percent of the body surface of an adult (at least grade 2b) is damaged - eight to ten percent of children are threatened. If left untreated, severe burns ultimately lead to cardiovascular failure and thus death.
Estimation of the prognosis
There are two systems that can be used to estimate the healing process of a burn victim. With the Banx Index, which is considered out of date, the percentage of the body surface area burned is added to the patient's age. According to this index, if the value is over a hundred, the probability of survival is less than ten percent.
The so-called ABSI score, which takes several factors into account, is more precise. In addition to age and extent, the presence of a respiratory burn, third-degree burns and the gender of the patient also play a role. But even with the ABSI score, certain risk factors are disregarded. Because according to more recent medical studies, in addition to accompanying or previous illnesses such as diabetes, wound healing disorders and increased susceptibility to infections, obesity and nicotine and alcohol consumption reduce the probability of survival.
Prospects for healing
Depending on the depth of the burn, healing can take several weeks or months. A 2nd degree burn will heal in about a month, leaving pronounced scars to form. If tissue has to be transplanted (transplantation), not only significant scars but also different skin tones can occur. Those with severe burns must be treated in specialized centers. In 2013, almost 13 percent of the severely burned patients admitted in 2050 died.
Prevent burns
Many burn accidents result from careless behavior. Prevention plays an important role, especially in the case of burns caused by electricity. In this way, safety measures at endangered workplaces are constantly being improved. Clarifications about safety precautions and regular maintenance work are also intended to protect against electrical burns.
You can also prevent burns at home with just a few simple measures. Always switch off the power before doing electrical work and use flammable substances such as alcohol properly. Don't smoke in bed. With small children in the household, you should close hot, open oven doors and put boiling pots or burning candles out of reach. This will reduce the risk of scalding or burns.
Tags: organ systems palliative medicine prevention