Biliopancreatic Diversion
Dr. med. Fabian Sinowatz is a freelancer in the medical editorial team.
More about the experts All content is checked by medical journalists.The biliopancreatic diversion (also BPD or biliopancreatic division) is the most complex and at the same time most effective operation in obesity surgery. The intervention deliberately causes a disturbance in the absorption of food in the small intestine (malabsorption). However, the biliopancreatic diversion cannot be completely reversed later and food supplements must be taken for life. Here you can find out everything about the requirements, implementation and effects of biliopancreatic diversion.
What is biliopancreatic diversion?
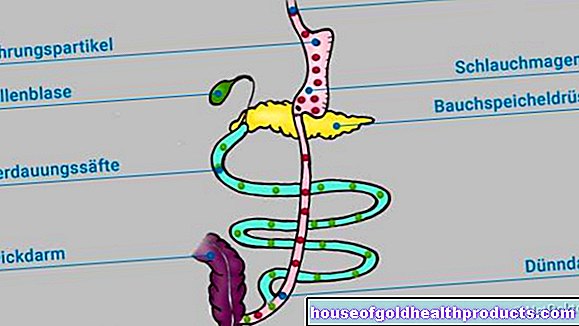
The term "biliopancreatic diversion" means that the digestive secretions of the bile (bilis) and pancreas (pancreas) are only conveyed to the food pulp in the lower part of the small intestine. This hinders the breakdown of nutrients and they are only absorbed in significantly smaller quantities from the small intestine into the blood.
Biliopancreatic diversion usually results in a particularly significant weight reduction in obese patients. Internationally, the biliopancreatic division is considered the standard procedure, but in Germany it has hardly gained acceptance.
What happens through biliopancreatic diversion?
The principle of action is primarily based on malabsorption deliberately caused by the operation - this is the technical term for poor absorption of nutrients from the intestine. Normally, the chyme coming from the stomach mixes with the digestive enzymes from the pancreas and gallbladder already in the duodenum. The nutrients are broken down as a result and can now be absorbed by the intestinal mucosa and passed on into the bloodstream.
Due to the biliopancreatic diversion, however, they are only introduced much further down into the small intestine. It is only from here that the food pulp and digestive juices mix. This means that only a short section of the intestine and significantly less time is available for the breakdown and absorption of food - a large part of the nutrients therefore migrate undigested into the large intestine and are excreted with the stool.
However, the weight reduction does not result solely from malabsorption. The second principle of action is the so-called restriction: With the biliopancreatic division, the stomach is significantly reduced, among other things. Due to the reduced stomach volume (restriction) you are full faster and therefore eat less.
Surgical Procedure for Biliopancreatic Diversion
Basically, a distinction is made between two variants of the operation: the sole biliopancreatic diversion (BPD) and the biliopancreatic diversion with duodenal switch (BPD-DS). In BPD, the stomach is reduced to a volume of around 250 to 500 milliliters. With BPD-DS, on the other hand, the stomach is reduced to a so-called “sleeve stomach” with a volume of only around 100 to 120 milliliters. This means that the restriction in the BPD-DS is even more pronounced than in the case of BPD alone. Another advantage is that the BPD-DS also has the pylorus. The chyme does not get unhindered from the remaining stomach into the intestine, but is released more slowly and continuously through the pylorus into the intestine. This significantly reduces the risk of what is known as dumping syndrome (see below).
Preparation for biliopancreatic diversion
Before the procedure, a gastroscopy is important to rule out serious diseases of the stomach and duodenum. An ultrasound of the abdomen should also be carried out in order to detect any existing biliary flow disorders - for example due to gallstones - beforehand. If gallstones are discovered, the gallbladder is usually removed as a precautionary measure during the biliopancreatic diversion, as further stones can quickly form later during the desired weight loss, which then very often lead to inflammation of the gallbladder and bile duct. Before the operation, an electrocardiogram (EKG) and a pulmonary function test are usually also necessary.
Course of the operation
Today, biliopancreatic diversion is mainly performed as a minimally invasive operation. This procedure, also known as the "keyhole technique", does not require a large abdominal incision. Instead, the surgical instruments and a small special camera are inserted into the abdomen through several small incisions in the skin. Minimally invasive operations generally have a lower surgical risk than open operations and are therefore particularly suitable for obese patients who are already at a significantly higher surgical risk.
The biliopancreatic diversion takes place in several surgical steps. Under general anesthesia, the surgeon inserts the instruments and a camera with a light source into the abdominal cavity through several skin incisions. During the operation, gaseous carbon dioxide is also introduced into the abdominal cavity so that the abdominal wall stands out from the organs and the surgeon has a better view and more space in the abdominal cavity.
Now the stomach is cut off just below the esophagus. At the end of the esophagus there is only a small residual stomach (stomach pouch) left. The remaining parts of the stomach are removed. In the case of biliopancreatic diversion with duodenal switch, instead of the gastric pouch, a so-called sleeve stomach with a considerably smaller volume is formed.
Next, the surgeon cuts the small intestine about 2.5 meters from the start of the large intestine. The lower part is now pulled up and sewn directly to the stomach pouch or sleeve stomach. The upper part of the small intestine no longer has any connection to the stomach and in future will only serve to transport the digestive secretions from the bile and pancreas. It is now passed about 50 centimeters above the large intestine into the small intestine and sutured.
The common piece of small intestine, in which the food particles and digestive juices mix, is therefore only about half a meter long instead of several meters. Since this is no longer sufficient for a complete breakdown and absorption of the food components, these are mainly passed on undigested into the large intestine, which in turn hardly absorbs any nutrients. Because it mainly serves to thicken the digested meal.
Duration of surgery, hospital stay and incapacity for work
The biliopancreatic diversion takes about two to three hours and is always performed under general anesthesia. The operation usually requires a hospital stay of around eight days - one for preparation and seven for close medical observation after the procedure. On average, about three weeks after the operation, if the course of the operation is uncomplicated, it is possible to resume professional activity.
For whom is biliopancreatic diversion suitable?
Biliopancreatic diversion is a procedure for people with obesity and a body mass index (BMI) of ≥ 40 kg / m² (obesity grade III). If metabolic diseases such as diabetes, high blood pressure or sleep apnea syndrome already exist due to being overweight, biliopancreatic diversion can be useful from a BMI of 35 kg / m².
The prerequisite for biliopancreatic diversion and all other interventions in obesity surgery is that all non-surgical measures have not shown sufficient success for a period of six to twelve months. These measures include professional nutritional advice, exercise training and behavioral therapy (a so-called multimodal concept for obesity). For biliopancreatic diversion, one should be at least 18 and at most 65 years old, although the operation is also possible for younger or older people in individual cases.
For people with extreme obesity (BMI> 50 kg / m²), the operation is sometimes divided into two operations: First, only the sleeve stomach is applied. This is intended to reduce the weight and thus the risk of surgery for the second procedure (the actual biliopancreatic diversion).
A malabsorptive procedure such as biliopancreatic diversion is particularly recommended for people who cannot change their unfavorable eating habits. While these people lose weight poorly through other procedures (such as sleeve stomach or gastric banding), weight loss can be expected in the case of biliopancreatic diversion due to malabsorption even with persistently unfavorable eating habits.
For whom is biliopancreatic diversion not suitable?
There are various physical and mental illnesses for which obesity surgery such as biliopancreatic diversion is not indicated (contraindicated). In particular, previous operations and malformations of the stomach or intestines can represent important contraindications for biliopancreatic diversion. Psychological comorbidities such as addictions or untreated eating disorders (e.g. "binge eating" or bulimia) are also exclusion criteria for the procedure. Whether you are suitable for biliopancreatic diversion or not, you can find out in advance in a conversation with the surgeon.
Effectiveness of biliopancreatic diversion
The biliopancreatic diversion is the surgical procedure with which the greatest weight loss is usually achieved. Studies have shown that excess weight loss (EWL) after one year is 52 percent for BPD alone and 72 percent for BPD-DS. In addition to the purely cosmetic and psychological relief effect, the weight loss after the procedure also has positive effects on the patient's metabolism. In many cases, the procedure greatly improves or even cures an existing diabetes mellitus. The blood sugar levels often return to normal shortly after the operation, although the patient has not lost any significant weight at this point. The reasons for this are not yet completely clear. Some researchers suspect that the altered gastrointestinal passage sets various hormonal changes in motion that have a beneficial effect on the energy metabolism.
Advantages of biliopancreatic diversion over other procedures
Since the effect of biliopancreatic diversion is based on two different principles (restriction and malabsorption, see above), the procedure is particularly effective and is particularly effective in people whose obesity is caused by excessive consumption of high-calorie foods or beverages. For these people, sometimes referred to as “sweet-eater”, a stomach-shrinking procedure such as the gastric balloon, gastric band or sleeve stomach would not be sufficiently effective.
Disadvantages and side effects of the procedure
A biliopancreatic division is a surgically demanding procedure. Compared to gastric sleeve surgery, significantly more cuts and sutures are necessary. The intervention in the digestive system is very pronounced and not completely reversible after successful weight loss. Therefore, one should familiarize oneself with the possible side effects before the procedure. How strong these are in each individual case varies:
Deficiency symptoms: One of the most common side effects of biliopancreatic diversion is a lack of vitamin D and vitamin B12: Vitamin B12 is absorbed in the last section of the small intestine (terminal ileum). A certain auxiliary protein, the so-called intrinsic factor, must also be available for absorption. The intrinsic factor is produced in the stomach. Since a large part of the stomach is removed in biliopancreatic diversion, the formation of the intrinsic factor is reduced and thus the vitamin B12 uptake is greatly reduced.
For this reason, vitamin B12 must be regularly administered into the muscle or via the vein into the blood throughout life.Vitamin B-12 preparations are also available that are absorbed directly through the oral mucosa (sublingual application), but their effectiveness is questionable. It is not yet clear why a vitamin D deficiency can occur after biliopancreatic diversion clarified.
Patients with biliopancreatic diversion must be careful to consistently supply vitamins B12 and D - otherwise there is a risk of severe complications such as anemia (anemia due to vitamin B-12 deficiency) and osteoporosis (due to vitamin D deficiency).
Dumping syndrome: The dumping syndrome (English to dump = to fall) describes the combination of several symptoms, which can arise from the sudden emptying of only slightly pre-digested food from the remaining stomach into the small intestine. Since there is no stomach door, the concentrated food goes straight to the small intestine. There, following the laws of physics (osmosis), it draws water from the surrounding tissue and blood vessels into the intestine.
This reduces the volume of fluid in the bloodstream, which can lead to a marked drop in blood pressure and even collapse. Some people report associated symptoms such as dizziness, nausea, sweating, or severe palpitations (early dumping). In addition, the high water content of the chyme can cause severe diarrhea.
Dumping syndrome occurs especially after the consumption of osmotically very active (hyperosmolar) food, for example with sugary drinks or after fatty foods. The dumping syndrome is prevented by the PBD-DS (see above). In this variant of biliopancreatic diversion, the gastric porter is retained.
Loss of muscle mass: Due to the greatly reduced supply of nutrients, there is a relative deficiency in carbohydrates, which the body tries to compensate by forming new sugars from amino acids. Amino acids are the building blocks of proteins, which in turn are an important building block of the muscles. Above all, the body breaks down underused muscles in order to secure the energy balance. Patients after biliopancreatic diversion should therefore counteract muscle breakdown by increasing physical activity. Joint-friendly sports such as cycling, moderate strength training, swimming or aqua jogging are particularly suitable.
Biliopancreatic Diversion: Risks and Complications
Biliopancreatic diversion harbors various general and specific surgical risks. This includes:
- general anesthetic risks
- Thrombosis of the deep veins in the leg with the risk of pulmonary embolism
- Infections in the area of the external and sutures
- Leakage of the organ sutures on the stomach pouch / sleeve stomach or small intestine (suture insufficiency) with the risk of peritonitis
In studies, mortality after biliopancreatic diversion ranged from 0.5 to 7.6 percent. However, these are purely statistical values. The individual surgical risk depends largely on the physical condition at the time of the operation.
Post-op nutrition
After the biliopancreatic diversion, a fundamental change in diet is necessary in order to avoid digestive problems. Apart from that, the weight loss is more pronounced the lower in fat and calories one eats after the operation. After biliopancreatic diversion, the following nutritional rules must be adhered to for life:
- Meals should only consist of small portions (reduced stomach size)
- every single bite has to be chewed very well, as there is no pre-digestion by the stomach
- sugary foods or drinks and very long-fiber meat should be avoided
- Food supplements (especially vitamin D, vitamin B12) must be taken for life
Medicines are also sometimes absorbed differently or in a smaller amount of active ingredient. The biliopancreatic diversion may therefore require an adjustment of the time and dose of medication.
Tags: sex partnership prevention menopause















.jpg)