TESE and MESA
Nicole Wendler holds a PhD in biology in the field of oncology and immunology. As a medical editor, author and proofreader, she works for various publishers, for whom she presents complex and extensive medical issues in a simple, concise and logical manner.
More about the experts All content is checked by medical journalists.TESE and MESA are abbreviations for two surgical procedures for obtaining sperm cells - either from the testes (TESE) or from the epididymis (MESA). These sperm are then available for artificial insemination using ICSI (intracytoplasmic sperm injection). Find out here which operation helps when and how the success of TESE and MESA is going.

What are TESE and MESA?
Since the beginning of the 1990s, men with poor spermiograms have been able to be helped: thanks to Intracytoplasmic Sperm Injection (ICSI), successful artificial insemination has basically only required a single fertilizable sperm cell - this is injected directly into the egg cell in a test tube with a fine needle. But what to do if the man's sperm does not contain any or too few sperm cells that can be obtained for ICSI?
In such cases, a TESE or MESA may help: These are small surgical interventions through which sperm cells are taken directly from the testicles or the epididymis:
- TESE stands for testicular sperm extraction, i.e. the extraction of sperm from the testes (in principle an extended testicular biopsy).
- MESA stands for microsurgical epididymal sperm aspiration, i.e. the extraction of semen from the epididymis.
A tissue-sparing, minimally invasive variant is the Mirko-TESE (also M-TESE, microsurgical extraction of testicular tubular segments), which is preferably used for small testes.
Artificial insemination using ICSI can then take place after a TESE or MESA.
How do TESE and MESA work?
MESA: epididymis in focus
With the MESA, the doctor punctures the epididymis with a fine needle (cannula) and removes epididymis. It will then be examined for active mature sperm (epididymal spermatozoa). The procedure is performed under general anesthesia and with the help of a surgical microscope. It is therefore somewhat more complex than testicular sperm extraction. The semen sample obtained is frozen (cryopreservation) and only processed shortly before the ICSI.
TESE: focus on testicles
During TESE, testicular tissue is removed from one or both sides in an outpatient procedure and examined for suitable sperm cells. The man receives a local or general anesthetic for this. The small operation works in detail as follows:
The surgeon exposes the testicles through a small, one to two centimeter long incision in the scrotum. He then takes at least three small tissue samples and sends them to the laboratory for analysis. with self-dissolving sutures and applies a pressure bandage to the scrotum.
In the laboratory, the testicular tissue samples are examined for active and fertile sperm. If you find what you are looking for, the tissue is frozen (cryopreservation). Only shortly before the ICSI is the frozen testicular tissue thawed and the sperm removed.
After the TESE, the patient has to take it easy for a few days and refrain from sex for one to two weeks.
Fresh TESE
In rare cases, fresh TESE is also possible, i.e. without the intermediate step of freezing. In that case, however, artificial insemination must begin immediately after the procedure. In this way, the costs of cryopreservation are eliminated and the risk of losing sperm due to freezing is reduced.
However, it should be remembered that the woman must undergo hormone treatment for artificial insemination in order to then obtain fertile egg cells from the ovaries that are stimulated in this way. This procedure, which is challenging for women, is in vain if no sperm cells capable of fertilization can be found in the testicle samples obtained using TESE.
Who are TESE or MESA for?
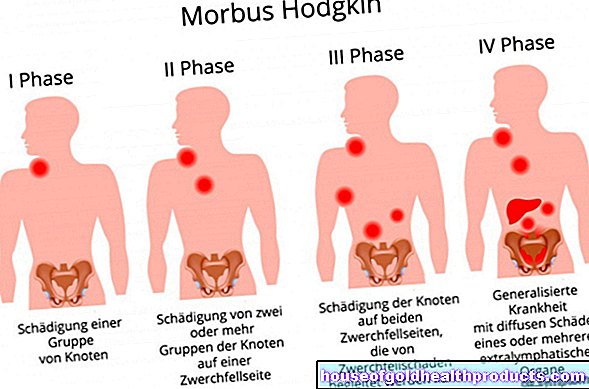
There are many reasons for a male fertility disorder: Pathological changes in the testicles or epididymis such as varicose veins (varicocele) or undescended testicles, testicular cancer, Klinefelter syndrome and testicular damage as a result of mumps can impair male fertility.
As a result of these disorders, there are often no sperm at all in the seminal fluid. Doctors then speak of azoospermia: either the man does not produce any sperm or such a small amount that no sperm cells can be detected in the ejaculate (non-obstructive azoospermia) or the path for the seminal fluid is blocked (obstructive azoospermia).
In both cases, TESE and MESA can help, provided that healthy sperm can be found in the testicular tissue or in the epididymal fluid. It must also be ensured beforehand that artificial insemination using ICSI is possible for the partner.
In addition, the reason for the poor semen analysis must be thoroughly checked before TESE and MESA. If the vas deferens are closed, an attempt should first be made to surgically restore the patency (re-fertilization operation). Incidentally, this also applies to men who still want children after sterilization. It is possible that the severed vas deferens can be reconnected and natural fertilization is possible again.
The MESA is primarily used for closed, non-reconstructable or missing spermatic ducts as well as immobile sperm. It is also suitable for men with non-treatable ejaculation disorders due to an operation or paraplegia.
TESE and MESA: chances of success
The chances of getting pregnant have increased significantly since the introduction of TESE and MESA and ultimately through ICSI.
Whether the TESE will be successful can be estimated from the testicle size and the basal level of the follicle-stimulating hormone (FSH). Small testicles and elevated FSH levels are unfavorable. In 60 percent of the cases, however, spermatozoa can be successfully obtained. The pregnancy rate is around 25 percent. With the Mirko-TESE, the tissue-friendly variant, testosterone production can be increased with medication and the method can thus be optimized.
The success of the MESA is independent of the number of spermatozoa obtained and the type of vas deferens occlusion. The pregnancy rate is around 20 percent.
Advantages and disadvantages of TESE and MESA
TESE and MESA are small surgical interventions. Therefore, there are the common risks associated with anesthesia and surgery: infection, bruising, swelling or bleeding can occasionally occur.
With TESE in particular, the tissue removal can reduce the testicle size. Sometimes this reduces the amount of hormone-producing cells in the testes so much that testosterone production is also restricted. Most of the time, however, this condition is only temporary and regenerates within a year. The risk for this is around ten percent. In very rare cases, the testicular tissue can shrink completely or even die.
The advantage of TESE and MESA is obvious - the chance to obtain fertilizable sperm cells despite an inadequate spermiogram and to conceive a child with the help of ICSI. Theoretically, only a single potent sperm cell is sufficient for this. Overall, TESE and MESA are relatively safe, effective and largely tissue-sparing microsurgical interventions.
Tags: drugs travel medicine Menstruation
















.jpg)