Hodgkin's disease
and Martina Feichter, medical editor and biologist Updated onDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Hodgkin's disease (Hodgkin's lymphoma) is a malignant tumor of the lymphatic system. It assumes degenerate white blood cells in the bone marrow. Typical symptoms of Hodgkin's disease are painless, swollen lymph nodes. The disease is one of the rare types of cancer and affects men a little more often than women. Read everything you need to know about Hodgkin's disease here: causes, symptoms, diagnosis, therapy and prognosis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C81
Brief overview
- Description: rare form of lymphatic cancer that mainly affects young adults - men more often than women.
- Symptoms: typically painless swollen lymph nodes, sometimes also B symptoms (fever, weight loss, night sweats) and / or unspecific complaints such as fatigue, weakness, itching, lymph node pain after alcohol consumption (alcohol pain)
- Causes: The exact causes are unknown. Several factors are probably involved in the development of cancer, such as infection with the Epstein-Barr virus, immune deficiency, genetic predisposition.
- Diagnosis: including physical examination, blood tests, analysis of tissue samples, x-rays, ultrasound, computed tomography
- Treatment: Mostly chemotherapy followed by radiation therapy. If necessary, further therapies such as stem cell transplantation or targeted therapies.
- Prognosis: Very good, most patients can be cured. However, it is important to diagnose and treat as early as possible.
Hodgkin's disease: description
Hodgkin's disease (Hodgkin's lymphoma) is a form of cancer of the lymph glands (malignant lymphoma), i.e. a malignant disease of the lymphatic system. It starts from degenerate lymphocytes, namely from B lymphocytes. This type of defense cells has the task of producing antibodies against invading pathogens (e.g. bacteria, viruses).
Other forms of lymph gland cancer are grouped under the term non-Hodgkin lymphoma. For the most part, they come from B lymphocytes, but sometimes also from T lymphocytes. The latter are another type of immune cell that is important for controlling immune responses and fighting viral infections.
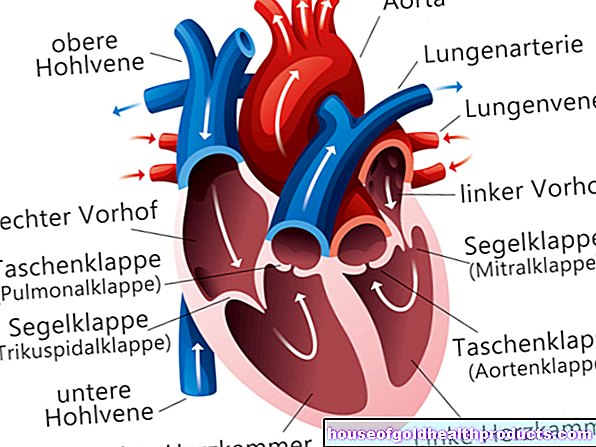
The lymphatic system
The lymphatic system (lymphatic system) includes the lymph vessels (lymph vessels) and the lymphatic organs such as the thymus, bone marrow and spleen. The lymph vessels collect and transport the tissue fluid (lymph) from the tissue back into the venous blood vessel system. Intermediate in the lymphatic vascular system are the lymph nodes - small, bean-shaped structures that filter the lymph. In lymph gland cancer, degenerate lymph cells establish themselves in the lymph nodes at an early stage of the disease.
Frequency of Hodgkin's disease
Hodgkin's lymphoma is a rare type of cancer. In 2020, 8,856 women and 11,002 men were newly diagnosed with it in Europe. The disease most commonly occurs in young adulthood. A second, smaller frequency peak is observed in older age (approx. 60 years).
Histological forms of Hodgkin's disease
From a histological (histological) point of view, Hodgkin lymphomas can be divided into two main groups: classical Hodgkin lymphoma and nodular lymphocyte-predominant Hodgkin lymphoma.
Classical Hodgkin lymphoma (cHL)
With a share of around 95 percent, classic Hodgkin lymphoma is by far the most common. It is further divided histologically into four subtypes:
- Nodular sclerosing type (NS): approx. 65 percent of all cases of Hodgkin lymphoma
- Mixed type (MC): approx. 25 percent
- Lymphocyte-rich type (LR): approx. 4 percent
- low-lymphocyte type (LD): approx. 1 percent
In all four subtypes, two types of degenerate cells appear that are characteristic of classic Hodgkin lymphoma - the mononuclear Hodgkin cells (arise from degenerate B lymphocytes) and the multinucleated Sternberg-Reed giant cells. The latter are said to result from the amalgamation of several Hodgkin cells.
The subtype of classic Hodgkin lymphoma has no influence on therapy planning.
Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL)
This form of Hodgkin lymphoma is also known as "nodular paragranuloma". It only accounts for about five percent of all Hodgkin's disease. The tumor cells occurring here are a variant of the Sternberg-Reed giant cells and are called L&H (lymphocytic & histiocytic) according to their morphology.
Hodgkin's disease: symptoms
The typical first sign in most Hodgkin's disease patients is prolonged (> four weeks), painless lymph node swellings. The affected lymph nodes under the skin are usually difficult to move, coarse and of a rubbery consistency.
The lymph nodes in the neck area are most often affected (in approx. 70 percent of cases), less often those in the armpits or in the groin region. These lymph nodes can be felt - in contrast to the lymph nodes behind the breastbone (mediastinal), which can also be swollen in Hodgkin's lymphoma (approx.six out of ten cases). The swelling of these mediastinal lymph nodes can be seen on X-rays and can also be noticeable in the form of impaired breathing, a feeling of pressure behind the breastbone and constant irritable cough.
Lymph node swellings in the abdomen are also possible. Indications of this can be pain and a feeling of pressure in the abdomen as well as unclear diarrhea.
Affected lymph node regions can be painful shortly after consuming even the smallest amounts of alcohol. This so-called alcohol pain is quite characteristic of Hodgkin's disease, but only occurs in very few patients. The exact mechanism behind the phenomenon is not yet known.
Swollen lymph nodes can also have harmless causes. For example, lymph nodes are typically enlarged in the event of an infection. Then, however, they usually react painfully to pressure (e.g. when palpating), can be easily moved under the skin and usually swell noticeably a short time after the infection.
General and B symptoms in Hodgkin's disease
Some Hodgkin's disease patients develop unspecific general symptoms such as fatigue, decreased performance and severe itching all over the body.
In addition, the so-called B symptoms can exist. This is the combined occurrence of the following three symptoms:
- Weight loss: Inexplicable loss of more than ten percent of body weight within six months.
- Night sweats: Inexplicable heavy sweating at night - those affected often grow up soaking wet and have to change their nightwear or bed linen.
- Fever: Inexplicable fever above 38 ° C, possibly as Pel-Epstein fever (= wave-like fever in Hodgkin lymphoma patients).
The B symptoms can occur not only with Hodgkin's disease, but also with some other serious illnesses (e.g. other cancers, tuberculosis, HIV / AIDS).
Symptoms in the further course
At an advanced stage, Hodgkin's lymphoma can affect various other organs - with corresponding symptoms.
For example, cancer colonization in the skeleton can lead to bone pain. An infestation of the bone marrow can result in changes in the blood count, for example with anemia, increased bleeding tendency and susceptibility to infection as the consequences. If the liver is affected by cancer, it can enlarge (hepatomegaly), which can cause a feeling of pressure in the upper abdomen and changes in the liver and bile values in the blood. The spleen can also enlarge due to cancer (splenomegaly) and cause abdominal discomfort. Neurological symptoms threaten when Hodgkin's lymphoma spreads to the nervous system.
Hodgkin's disease: causes and risk factors
The exact causes of Hodgkin's disease are not yet known. Presumably, however, several factors must come together for the disease to develop.
In some patients, an infection with the Epstein-Barr virus (EBV) - the causative agent of Pfeiffer's glandular fever - could be involved in the development of Hodgkin's disease.
Researchers are also investigating a possible genetic predisposition to Hodgkin's lymphoma: the children and siblings of patients have a slightly higher risk of developing this type of lymphatic cancer.
A congenital or acquired (e.g. due to HIV) immune deficiency is also considered a risk factor for Hodgkin's disease: It can promote the development of degenerate B lymphocytes.
There may also be a link between Hodgkin's disease and long-term smoking. Various substances in tobacco smoke can damage the genome of body cells so that they degenerate more easily.
To what extent other lifestyle factors and environmental factors play a role in the development of Hodgkin's disease is currently unclear.
Hodgkin's disease: examinations and diagnosis
The right person to contact if you suspect Hodgkin's disease is your general practitioner or a specialist in internal medicine and oncology.
Medical history and physical examination
The doctor will first ask you about your medical history (anamnesis). This information will help him to narrow down the possible causes of your symptoms. Possible questions from the doctor include, for example:
- What complaints do you have?
- How long have the complaints existed?
- Have you noticed any swelling in your neck or other parts of your body?
- Have you recently woken up sweaty at night?
- Have you lost body weight in the past six months without eating less or exercising more?
- Have you had a fever lately?
- Does the consumption of alcohol cause you pain?
- Are you aware of any underlying illnesses?
- Does your family have cancer of the hematopoietic system (leukemia, lymphoma)?
The anamnesis is usually followed by a physical examination. The doctor measures your blood pressure and pulse and listens to your lungs. Above all, however, he checks whether he can feel enlarged lymph nodes somewhere. He also scans the spleen and liver - they can also be enlarged in Hodgkin's lymphoma.
Blood test
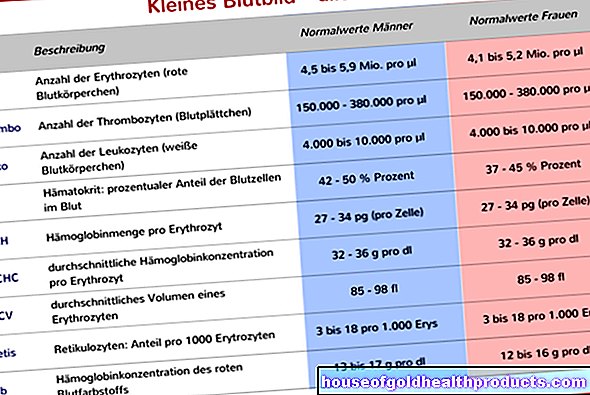
Blood analyzes are also part of the diagnosis of suspected Hodgkin's disease. The blood count of sick people often shows unspecific signs of inflammation such as an increase in blood sedimentation (blood cell sedimentation rate, ESR). Among other things, the liver values (such as Gamma-GT, GPT), the kidney values creatinine and uric acid as well as bilirubin and alkaline phosphatase are also determined.
The proportion of the various white blood cells (leukocytes), as determined in the course of the complete blood count, is also important. For example, a shortage of lymphocytes - called lymphocytopenia - can set in early in the course of the disease. Sometimes there is also a shortage of red blood cells (erythrocytes), i.e. anemia (anemia). In about 20 percent of the cases in Hodgkin's disease, the blood count shows an increased number of eosinophils - a subtype of white blood cells. Medical professionals refer to this as eosinophilia.
As part of the laboratory tests, the patient's blood is also tested for antibodies to HIV, hepatitis B and hepatitis C. In addition, the blood level of lactic dehydrogenase (LDH) and - in women - that of human chorionic gonadotropin (HCG) are measured.
Tissue sample bone marrow & lymph nodes
If Hodgkin's disease is suspected because the lymph node swelling is unexplained and has persisted for more than four weeks, a complete lymph node is removed to confirm the diagnosis (lymph node extirpation) and examined under the microscope for characteristic cell changes (a second pathologist should confirm the diagnosis).
Tissue samples from the bone marrow (biopsy) provide another diagnostic option. The doctor pulls the sample out of the medulla of the iliac crest with a puncture needle. Such a bone marrow tissue sample can also contain degenerate cells and thus provide evidence of Hodgkin's disease. According to the S3 guideline from June 2018, however, a bone marrow biopsy should be dispensed with if bone marrow involvement has been ruled out in the imaging using PET / CT.
Imaging procedures
Imaging examinations help to determine the stage of the disease and to detect any secondary tumors (metastases) in other organs. X-rays, ultrasound, computed tomography (CT) and PET / CT are used. Other examinations, such as magnetic resonance imaging (magnetic resonance imaging, MRI), can be useful as required.
Hodgkin's disease - staging (according to Ann-Arbor)
Hodgkin's disease is divided into four stages, depending on how much it has spread in the body. The more lymph node regions are affected, the more advanced the disease and the worse the prognosis. Basically, Hodgkin's disease is a cancer that can be cured at any stage.
|
stage |
Infestation |
|
I. |
Involvement of only one lymph node region or a single localized attack outside the lymphatic system |
|
II |
Involvement of two or more lymph node regions on the same side of the diaphragm or localized incursion outside the lymphatic system and lymph node regions on the same side of the diaphragm |
|
III |
Involvement of two or more lymph node regions or organs outside the lymphatic system on both sides of the diaphragm |
|
IV |
Non-localized, diffuse or disseminated involvement of one or more extralymphatic organs (such as the brain) with or without involvement of lymphoid tissue |
The stage is further described with the addition of A or B: addition A stands for the absence of B symptoms (night sweats, fever, weight loss), addition B for the presence of B symptoms.
Defined risk factors
In addition to the staging, the determination of further, precisely defined risk factors is important for therapy planning. These include:
- Large mediastinal tumor, i.e. a tumor behind the breastbone, the size of which is at least one third of the diameter of the chest
- Extranodal involvement, i.e. spread of the tumor beyond lymphatic tissue (lymph nodes, spleen, thymus, etc.)
- high blood sedimentation
- Involvement of three or more lymph node areas ("lymph node areas" are not synonymous with "lymph node regions" in the Ann-Arbor classification, but sometimes include several such lymph node regions)
Stage + risk factors = risk group
Depending on the stage of Hodgkin's lymphoma and the defined risk factors that are present, they are divided into risk groups:
>> early stages
This includes Hodgkin lymphomas in stage I A or B (i.e. stage I without or with B symptoms) according to Ann-Arbor, if none of the defined risk factors mentioned above are present.
>> medium stages
These include Hodgkin's lymphomas of the following characterization:
- Stage I A or B with one or more risk factors
- Stage II A with one or more risk factors
- Stage II B, if the risk factors are high blood sedimentation and / or involvement of three or more lymph node areas
>> advanced stages
One speaks of an advanced stage Hodgkin lymphoma in the following cases:
- Stage II B, if the risk factors are extranodal involvement and / or large mediastinal tumor
- Stage III A or B
- Stage IV A or B
The treating physicians orientate themselves to the risk group (early, middle, advanced stage) when planning the therapy.
Hodgkin's disease: treatment
Therapy for Hodgkin's disease is individually tailored to each patient. Before starting therapy, the attending physician should provide the patient with comprehensive, understandable and complete information about the planned treatment, its effects and possible side effects. He should also offer participation in clinical studies - as far as possible. In addition, the doctor clarifies whether the cancer patient needs psychological support (psycho-oncological support).
Chemotherapy and radiation therapy
Most Hodgkin lymphoma patients receive chemotherapy and radiation therapy. There are differences depending on the stage of the disease.
>> Therapy in the early stages
Affected patients are preferably treated with a combination of chemotherapy and radiation therapy (exception: in the rare nodular lymphocyte-predominant Hodgkin lymphoma, NLPHL, radiation therapy is sufficient treatment in stage I A without risk factors).
Chemotherapy is usually carried out according to the so-called ABVD scheme in two cycles. The letters ABVD stand for the four chemotherapeutic agents that are administered to the patient in combination here: Adriamycin (= doxorubicin), bleomycin, vinblastine and dacarbazine. After completing the chemotherapy, the patient is then irradiated.
After the two cycles of chemotherapy using the ABVD scheme, an imaging examination using PET / CT is recommended to check how well the tumor has responded to treatment. If necessary, an intensification of the therapy can be considered individually. Then two additional chemotherapy cycles are carried out according to the BEACOPPescalated scheme (bleomycin, etoposide, adriamycin, cyclophosphamide, oncovin = vincristine, procarbazine, prednisone).
>> Therapy in the middle stages
For middle-stage Hodgkin lymphoma, treatment consists of four cycles of chemotherapy, supplemented by radiation if necessary. There are differences depending on the age of the patient:
Patients aged 60 and under should receive two cycles of BEACOPPescalated followed by two cycles of ABVD. Alternatively (e.g. if the patient refuses the intensive BEACOPP chemotherapy) four cycles of ABVD are available.
In some cases, this is followed by radiation therapy. The decision about this depends on the result of the PET / CT examination, which is used to check its effect after chemotherapy. Exception: If the patient has received four ABVD cycles as chemotherapy, radiation is always added.
In principle, intensified BEACOPP chemotherapy is not carried out in patients over 60 because it is associated with excessive toxicity and mortality in this age group. Instead, if their general condition allows, patients should receive two cycles of ABVD and two cycles of AVD. If this does not work, choose a different chemotherapy regimen. In any case, the remaining tumor tissue is still irradiated after chemotherapy.
>> Therapy in advanced stages
Advanced Hodgkin's lymphoma is also treated with chemotherapy and, if necessary, radiation therapy:
Patients up to the age of 60 generally receive intensified chemotherapy BEACOPPescalated. The number of treatment cycles depends on the PET / CT findings. After completion of the chemotherapy, PET / CT should be used to check how well the tumor has responded to the chemotherapeutic agents. Depending on the result, radiation therapy may also be carried out.
Patients over 60 years of age also receive chemotherapy, but not BEACOPP, but, for example, two cycles of ABVD and four to six cycles of AVD. This is usually followed by radiation.
Other therapies
In certain cases of Hodgkin's disease, other therapy options are available. Here are some examples:
If the usual chemotherapy and radiation therapy treatments are unsuccessful or if there is a relapse, an autologous stem cell transplant is sometimes performed: healthy blood stem cells (from which the lymphocytes, among other things, are derived) are taken from the patient. Then high-dose chemotherapy destroys the patient's entire bone marrow, including any cancer cells. The sick person then receives the blood stem cells previously removed back, which then ensure that new blood is formed with healthy cells.
Blood stem cells from a suitable donor are rarely used for stem cell transfer (allogeneic stem cell transplantation).
You can read more about the exact process and possible risks of stem cell transfer in the article Stem Cell Transplantation.
For some years now, selected Hodgkin's disease patients have had the option of targeted therapy with the active ingredient brentuximab vedotin. It is an artificially produced antibody that is loaded with a chemotherapeutic agent. The antibody can dock on a certain surface protein of the cancer cells, whereupon it is absorbed into the cell interior. There the chemotherapeutic agent is released so that it can develop its effect - the cancer cell can no longer divide and dies. However, this treatment is only possible in patients whose tumor cells contain the surface protein mentioned.
In some patients, attempts are made to treat Hodgkin's lymphoma with immunotherapy with checkpoint inhibitors (anti-PD1 antibodies) such as nivolumab: Hodgkin's lymphoma can activate certain control points of the immune system that slow down immune reactions (immune checkpoints). This protects the tumor from an attack by the body's defenses. Checkpoint inhibitors can release these "brakes" and thus increase the immune system's fight against cancer.
Hodgkin lymphoma: therapy in pregnant women
Young adults are most likely to develop Hodgkin lymphoma. Thus, it is not uncommon for pregnant women to be affected. These should then be closely monitored during obstetrics. This includes - in addition to the standard examinations - an ultrasound examination with measurement of the unborn child (fetometry), amniotic fluid and ultrasound control of the unborn child every three weeks.
Chemotherapy treatment for Hodgkin lymphoma during pregnancy depends on the stage of pregnancy:
If a woman falls ill with Hodgkin's lymphoma in the first trimester of pregnancy, the necessary chemotherapy should, if possible, be waited until the beginning of the second trimester. The reason: chemotherapy drugs carry a high risk of child malformations, which can be particularly fatal at the beginning of pregnancy. Until chemotherapy becomes possible, the pregnant woman should be closely monitored by a doctor.
If Hodgkin's lymphoma is diagnosed in the 2nd or 3rd trimester, chemotherapy can in principle be carried out straight away (up to about two weeks before delivery).However, it is checked individually whether the cancer treatment cannot be postponed until after the birth.
As described above, radiation therapy is very often indicated as a supplement to chemotherapy. However, this should not be carried out during pregnancy, but only after the birth. There should be a maximum of 12 weeks between the completion of chemotherapy and the start of radiation.
Other measures
When treating Hodgkin's disease, it is also important to treat the side effects of the therapy, for example with anti-nausea medication (a common side effect of chemotherapy).
During Hodgkin's disease therapy, patients should use double contraception (e.g. contraceptive pill and condom). The drugs used for treatment can damage the development of an unborn child.
Patients also benefit from exercise during and after cancer treatment. For example, it can help against the persistent tiredness and exhaustion that are often associated with cancer (fatigue syndrome).
Doctors should talk to patients of fertile age about measures to protect fertility before starting therapy - cancer therapy can affect fertility. For example, there is the possibility of removing unfertilized egg cells or sperm before starting therapy and freezing them for artificial insemination at a later date.
Hodgkin's disease: disease course and prognosis
The chances of a cure for Hodgkin's disease are very good. Hodgkin's lymphoma is sensitive to chemotherapy and radiation therapy and can therefore be cured in most cases. The earlier the disease is discovered and treated, the better the chances of recovery. But even with advanced Hodgkin lymphoma, a cure is still possible. Even with a relapse of Hodgkin's disease - i.e. a relapse of the cancer - good long-term therapy results and even cures can often be achieved. However, years or decades after Hodgkin's disease treatment, another cancer (non-Hodgkin's lymphoma, leukemia, etc.) can develop due to chemotherapy and radiation therapy.
Tags: dental care Diseases prevention
























.jpg)