Kidney cancer
and Martina Feichter, medical editor and biologist Updated onSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Kidney cancer (malignant kidney tumor) is a malignant growth of the kidney. It can start from different cell types. Renal cell carcinoma (renal cell cancer) is by far the most common in adults. Most of the patients are older and male. Read everything you need to know about the topic: causes, symptoms, diagnosis, treatment and chances of a cure for kidney cancer.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C64C65
Brief overview
- What is kidney cancer (kidney cancer)? A malignant tumor of the kidney, with renal cell cancer (renal cell carcinoma) being the most common variant. Most of the patients are older men.
- Symptoms: Usually none at first, later mostly blood in the urine and kidney / flank pain. The tumor may be palpable. Other possible symptoms: tiredness, fever, lack of appetite, weight loss, anemia, high blood pressure and possibly signs of metastases such as bone pain, shortness of breath, headache, etc.
- Causes: Not exactly known. Risk factors are smoking, obesity, high blood pressure, end-stage kidney weakness, genetic predisposition and old age.
- Diagnostics: doctor-patient consultation, physical examination, laboratory tests, imaging (ultrasound, computed tomography, magnetic resonance tomography), biopsy if necessary. Furthermore studies on tumor spread.
- Therapy: Surgical removal if possible. In the case of a small tumor, only active monitoring or ablative therapy (e.g. destruction with cold) may be required. In advanced stages, drug therapy, radiation therapy, as an alternative or in addition to surgery.
- Prognosis: Relatively good if the kidney cancer is recognized and treated in good time. However, if there are already metastases of kidney cancer, the life expectancy (chance of survival) of those affected is significantly lower.
What is kidney cancer?
Kidney cancer (renal carcinoma) is a malignant tumor of the kidney. It arises when individual cells of the kidney undergo malignant changes (degenerate) and begin to proliferate unchecked. Such a kidney cancer tumor can develop from different cell types.
By far the most common variant in adults is renal cell cancer (renal cell carcinoma, adenocarcinoma of the kidneys). It develops from epithelial cells of the nephrons (nephron = basic functional unit of the kidneys). There are different types of renal cell carcinoma: By far the most common is the so-called clear cell carcinoma; Papillary carcinoma and Bellini duct carcinoma are less common.
This article is primarily about renal cell cancer!
In addition to renal cell carcinoma, other malignant kidney tumors fall under the term kidney cancer. This includes, for example, the rarer renal pelvic carcinoma. It develops from the tissues of the urinary tract, which originate in the kidneys.
In children, it is not the kidney cell carcinoma but the so-called nephroblastoma (Wilms tumor) that is the most common type of malignant kidney tumor. It arises from cells that resemble kidney cells in the embryo, which is why it is called an embryonic tumor. Overall, however, children rarely develop a malignant tumor on the kidney.
Kidney metastases and kidney cancer metastases
In some cases, a malignant growth in the kidney does not turn out to be kidney cancer, but rather as a daughter tumor (metastasis) of another type of cancer somewhere in the body. Such kidney metastases can be caused by lung cancer or breast cancer, for example.
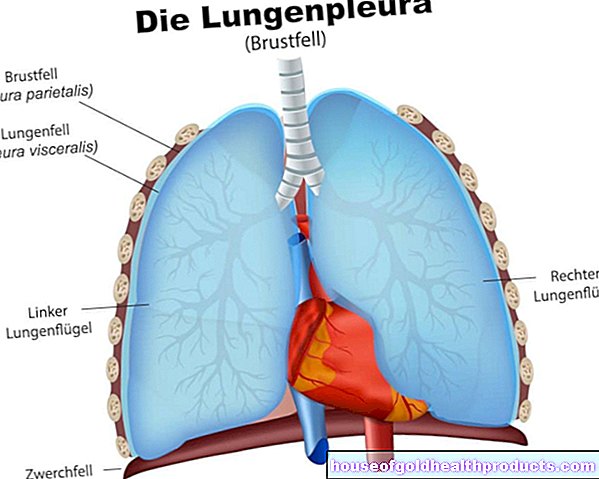
Kidney cancer metastases, on the other hand, are daughter settlements of kidney cancer in other parts of the body. They arise when individual cancer cells detach themselves from the tumor, reach other locations via lymph and blood vessels, attach themselves there and form a secondary tumor. Kidney cancer can affect lymph nodes and cause metastases in the lungs, bones, liver or brain, for example.
As soon as the first metastases have formed, the prognosis and chances of a cure for patients with kidney cancer worsen.
Function of the kidneys
The paired kidney fulfills vital tasks in the body: First and foremost, it continuously filters the blood, taking out harmful substances, among other things, which are then excreted with the urine it produces.
The kidneys also help regulate the water and electrolyte balance as well as the acid-base balance. Last but not least, they produce two hormones: renin (important for regulating blood pressure) and erythropoietin (involved in regulating erythrocyte production).
You can find out more about these tasks of the kidneys in the article Kidney function.
Kidney cancer: frequency
Kidney cancer - by far the most common variant, kidney cell cancer - mainly affects older men. Overall, it is a rather rare form of cancer:
In Germany, the Center for Cancer Registry Data (Robert Koch Institute) registered a total of 14,029 new cases in 2017, in 8,864 men and 5,165 women. Kidney cancer accounted for almost 2.9 percent of all new cancer cases * (489,178) this year.
According to Statistics Austria, a total of 1,370 people were diagnosed with kidney cancer in 2018 with 897 men and 473 women. That was around 3.2 percent of all new cancer cases * (42,219) this year.
According to the Swiss Cancer League, there were an average of 1,000 new cases of kidney cancer (renal cell cancer) per year in the period from 2013 to 2017 - 690 in men and 310 in women. This corresponded to a share of around 2.4 percent of the average annual new cancer cases * (42,500).
* "New cancer cases" means all new cases of malignant neoplasms (including leukemia and lymphomas) - with the exception of the new cases of "white" skin cancer (non-melanotic skin cancer). It is an international practice not to include this under "total cancer".
How do you recognize kidney cancer?
Kidney cancer (renal cell carcinoma) often causes no symptoms for a long time. The first symptoms usually only appear in more advanced stages - when the tumor has reached a certain size and / or has metastasized in more distant regions: Kidney cancer often causes blood in the urine (hematuria) and pain in the kidney area or flank pain. In some patients, the tumor can be felt.
General symptoms of kidney cancer include fatigue, fever, loss of appetite, and unwanted weight loss. However, these symptoms are very unspecific - they can also appear in other forms of cancer and many other diseases.
Other possible kidney cancer symptoms are high blood pressure (hypertension), anemia, and high levels of calcium in the blood (hypercalcemia). Liver dysfunction with an increase in alkaline phosphatase (AP) in the blood - called Stauffer's syndrome - is typical of renal cell carcinoma.
In male patients, there may be another sign of kidney cancer: if the tumor breaks into one of the kidney veins, a varicose vein rupture in the testicle (varicocele) can develop.
Metastatic kidney cancer: symptoms
If the kidney cancer has spread in the body, there are generally other symptoms. A few examples: Pain and spontaneous fractures are possible signs of bone metastases, i.e. skeletal involvement by the malignant kidney tumor. Symptoms of lung metastases can include shortness of breath and chest pain. Brain metastases can manifest themselves, for example, with headaches, nausea, vomiting, paralysis or seizures.
Kidney cancer: causes and risk factors
The causes of kidney cancer or kidney cell cancer are largely unknown to this day. There are, however, certain established risk factors that favor the outbreak of the disease. These include:
- smoking
- Obesity
- high blood pressure
- End-stage renal failure: This is chronic kidney failure in stage 5 (end stage). Possible causes include kidney damage from diabetes or high blood pressure and polycystic kidney disease (a genetic disease in which numerous fluid-filled cavities form in the kidneys).
- Genetic predisposition: In rare cases, hereditary gene mutations contribute to the development of renal cell cancer (hereditary renal cell carcinoma). The most common is the von Hippel-Lindau syndrome, caused by mutations in the VHL gene. They significantly increase the risk of clear cell carcinoma (the most common type of kidney cell cancer).
Old age is also linked to an increased risk of kidney cancer. Life expectancy and prognosis are then mostly influenced by concomitant diseases that often occur in old age (e.g. cardiovascular diseases).
Some experts also classify occupational exposure to halogenated hydrocarbons or long-term X-rays as kidney cancer risk factors (renal cell cancer risk factors).
Influence of diet unclear
The relationship between dietary factors and the risk of renal cell cancer is contradicting itself. There is also no evidence that fruit and vegetable consumption can prevent tumors from developing. Overall, the data currently available do not allow any conclusions to be drawn about the possible influence of certain foods or nutrients on the development of renal cell cancer.
How is kidney cancer diagnosed?
Kidney cancer (renal cell cancer) is discovered more and more by chance: In the course of examinations that are carried out for other reasons (e.g. ultrasound examination or computed tomography of the abdominal cavity), malignant kidney tumors are found in many patients. Often it is then still quite small, i.e. not very far advanced.
In other cases, the diagnosis of kidney cancer is only made when symptoms of the more advanced tumor prompt the person to see a doctor.
Medical history and physical examination
In the case of unexplained complaints, the medical history is routinely taken first (anamnesis): The doctor inquires exactly which complaints the patient has, how severe they are and how long they have existed. He also asks, among other things, about any previous or underlying illnesses.
The next step is the physical examination. This includes, for example, palpating the kidneys from the outside - the doctor may be able to identify a hardening or lump.
However, further examinations are required for a diagnosis of kidney cancer. In addition, there are examinations that can be used to determine the extent of the cancer (e.g. presence of metastases). This is important for therapy planning.
Laboratory tests
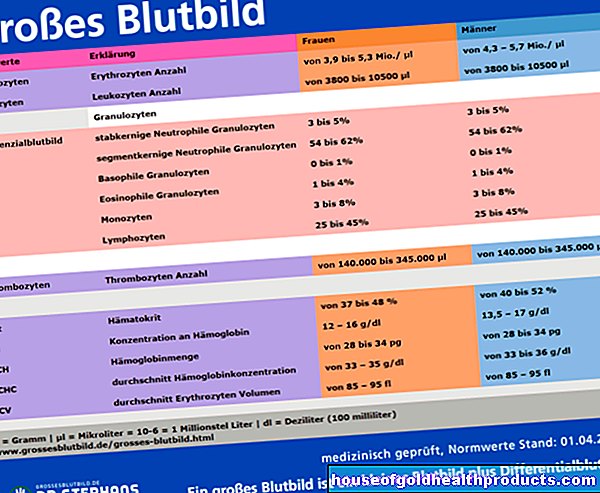
Laboratory tests can detect abnormal changes in the patient's blood and urine samples. If kidney cancer is suspected, blood values such as blood count, blood clotting and electrolytes in the blood (such as sodium, potassium, calcium) are determined. In addition, one measures the blood level of alkaline phosphatase (AP), the kidney values in the blood and urine and the liver values.
In addition, the urine is checked for blood (hematuria). Sometimes this proportion of blood is so large that the urine is visibly reddish in color (macrohematuria). In other cases, invisible amounts of blood are found in the urine (microhematuria).
Imaging procedures
If the kidney tumor is of a certain size, it can usually be detected in an ultrasound examination (sonography). Computed tomography (CT) offers a much higher image resolution. It is the standard method for detecting small kidney tumors. It is also used to determine the extent of the cancer (staging) and to plan the surgical removal of the tumor.
In some cases, another high-resolution imaging method is chosen as an alternative to CT - magnetic resonance imaging (MRT), also known as magnetic resonance imaging. It is recommended, for example, if there is a suspicion that renal cell carcinoma has already grown into the venous vessels or the vena cava. Then the spread of the tumor can be assessed better with MRI than with CT.
biopsy
Imaging is usually sufficient to reliably diagnose kidney cancer (renal cell cancer). However, if the diagnosis is still unclear afterwards, it is possible to take a tissue sample and examine the tissue under the microscope (biopsy). However, this should only be done if the choice of therapy depends on the results of the examination. If, on the other hand, it is clear from the outset that an unclear kidney tumor will be surgically removed, for example, no tissue sample should be taken beforehand.
The reason for this is that taking samples is associated with certain risks (including bleeding). A kidney biopsy is therefore only recommended in certain cases - such as for the treatment decision in the case of an unclear kidney tumor. In addition, a biopsy should or can be performed in the following cases to confirm the diagnosis:
- before an ablative therapy - i.e. before the targeted destruction of the tumor tissue by means of cold (cryoablation) or heat (radio frequency ablation)
- in patients with metastases before a planned kidney removal (cytoreductive nephrectomy)
In the case of cystic kidney tumors (= kidney tumors with fluid-filled cavities), however, a biopsy is not recommended. One reason for this is the potential risk of cyst fluid leaking into healthy tissue during sample collection and thus spreading tumor cells.
Performing the biopsy
The biopsy should be performed as a punch needle biopsy. Under ultrasound or CT control, a fine hollow needle is "shot" with a punch through the abdominal wall into the tumor tissue in order to obtain a cylindrical tissue sample. At least two such tissue cylinders should be removed. The patient is given a local anesthetic before the biopsy.
Further investigations
Once the diagnosis of kidney cancer (renal cell cancer) has been made, it is important to find out how far the cancer has already spread in the body (spread diagnosis). Which examinations are necessary and useful for this depends on the individual case.
For example, all symptom-free patients with kidney tumors larger than three centimeters should have a computed tomography of the chest (chest CT). The greater the tumor size, the greater the likelihood of metastases, for example in the lungs.
If brain metastases are suspected (e.g. due to seizures, paralysis, headaches), magnetic resonance imaging of the skull (cranial MRI) is recommended. For better imaging, the patient should be injected with a contrast medium prior to the examination.
If there are possible signs of bone metastases (e.g. pain), the patient's entire body is examined using CT or MRI (whole-body CT or MRI).
Occasionally, a vascular x-ray (angiography) is performed - but not to determine the spread of kidney cancer in the body, but to determine the vascular supply to the tumor. This can be helpful for the subsequent surgical removal of the tumor.
Kidney cancer: therapy
The stage of the tumor has the greatest impact on the type of treatment for kidney cancer. The age and general state of health of the patient are also taken into account when planning therapy.
Basically, a locally limited (not metastatic) renal cell cancer is operated on if possible: If the malignant tumor can be completely cut out, the kidney cancer is curable. In the case of a small kidney tumor, active monitoring or ablative therapy can be chosen as an alternative to surgery in certain cases.
In the case of renal cell carcinoma with metastases, cure is usually no longer possible - i.e. no curative therapy that aims at a cure. Instead, people with end-stage kidney cancer receive palliative therapy. This aims to avoid or alleviate symptoms, improve the quality of life of the patient and extend his life. Various therapy options are available for this.
For example, the tumor on the kidney and the individual metastases can be treated locally by means of surgery and / or radiation therapy. In addition, drugs are available against kidney cancer that act on the whole body (systemic therapy).
In the following you will find more detailed information on the various therapeutic approaches for renal cell cancer.
Active surveillance
In the case of a small renal cell carcinoma that has not yet metastasized, the therapy may be limited to active surveillance. This consists of regular check-ups, during which the tumor growth is checked with imaging procedures.
Such active monitoring can be useful in patients for whom surgical removal of the tumor or other form of cancer therapy would be too stressful - for example, in patients with other diseases and / or a limited life expectancy. Active monitoring is also a possible strategy for patients who refuse surgical or ablative therapy (see below) for their small kidney tumor.
When an actively monitored tumor grows, experts recommend its surgical removal.
Ablative therapy
A possible alternative to active monitoring in patients with small renal cell carcinoma as well as additional diseases and / or limited life expectancy is ablative therapy. This means the direct destruction of the tumor tissue without major surgical intervention. Usually this is done using cold (cryoablation) or heat (radio frequency ablation):
- Cryoablation: The doctor inserts a cold probe into the renal cell carcinoma through a small incision in the abdominal wall or as part of a laparoscopy. The probe cools the tumor tissue to -60 to -70 degrees Celsius, whereupon it dies.
- Radiofrequency ablation (RFA): Here too, a probe is inserted into the kidney tumor through the abdominal wall or during a laparoscopy. With the help of alternating current, she heats the cancerous tissue to 60 to 100 degrees Celsius, which destroys it.
In both cases, the insertion and "work" of the probe are monitored on a screen using imaging techniques (such as ultrasound or CT).
Operation: Different techniques
There are various options and techniques for the surgical treatment of renal cell cancer.
Non-metastatic kidney cancer: surgery
Surgical removal is the treatment of choice for non-metastatic renal cell cancer. If possible, surgery is performed to preserve the organs (partial nephrectomy): the surgeon only cuts out the cancerous part of the kidney. He makes sure to preserve as much healthy kidney tissue as possible.
The procedure is usually carried out as an open operation, i.e. over a longer skin incision (depending on the location of the tumor, for example on the abdomen or on the flank).
A surgeon with sufficient experience can also partially remove the kidney as part of a laparoscopy. Because this only requires several small incisions in the abdominal wall, through which the surgical instruments are inserted into the abdominal cavity, one also speaks of keyhole surgery or minimally invasive surgery.
A non-metastatic renal cell carcinoma cannot always be removed in such a way that the rest of the kidney is preserved. Then the entire organ has to be removed, which doctors call a radical nephrectomy. Usually this is not a problem - the second, healthy kidney can take over all kidney functions on its own.
If patients with non-metastatic renal cell cancer have enlarged lymph nodes, they can be surgically removed to check for cancer cells. If, on the basis of the imaging examinations before the operation or during the operation, it is suspected that an adrenal gland is also affected by the cancer, it will also be removed.
Metastatic kidney cancer: surgery
If a renal cell cancer has already spread to other organs, you can no longer achieve a cure with its surgical removal. However, in some cases it can be useful to excise the malignant kidney tumor. This can relieve discomfort such as local pain and bleeding, for example. Surgery may even extend a patient's survival.
Systemic therapy
In the case of advanced and / or metastatic renal cell cancer, cancer drugs are usually given that work throughout the body (i.e. systemically). The following substance groups are available:
- Tyrosine kinase inhibitors (e.g. axitinib, sorafenib): They inhibit signaling pathways in cancer cells that control their growth. They also block the formation of new blood vessels that the tumor needs to grow. All in all, kidney cell cancer can be prevented from growing for at least a while.
- mTOR inhibitors (temsirolimus, everolimus): The enzyme mTOR is generally important for cell growth and supply. Cancer cells contain a particularly large amount of this enzyme and can thus grow and multiply in an uncontrolled manner. mTOR inhibitors limit this proliferation of cancer cells.
- Checkpoint inhibitors: Immune checkpoints are control points of the immune system that limit immune reactions (e.g. against the body's own cells) if necessary. Some cancer tumors (such as kidney cancer) can activate these "brakes" and thus protect themselves from attack by the body's defenses. Checkpoint inhibitors (such as pembrolizumab, nivolumab) remove these "brakes".
- VEGF antibodies: The artificially produced antibody bevacizumab inhibits certain binding sites for growth factors (VEGF receptors) and thus the formation of new blood vessels that the growing kidney tumor needs to supply.
Doctors decide on a case-by-case basis which drugs are best for a kidney cancer patient. Active ingredients are often combined with one another, for example pembrolizumab plus axitinib. The VEGF antibody bevacizumab is also not given alone in renal cell cancer. Instead, it is always combined with interferon - an active ingredient that counteracts the growth of cancer cells.
The medication is used, for example, in the form of infusions or tablets, depending on the active ingredient. During systemic kidney cancer treatment, the course of the disease should be monitored every six to twelve weeks with the help of a detailed imaging examination (preferably computed tomography).
The "classic" drug treatment for most forms of cancer is chemotherapy. In kidney cancer - i.e. metastatic renal cell cancer - it is not a treatment option because it usually has no effect here.
Local treatment of kidney cancer metastases
Kidney cancer metastases (lungs, bones, etc.) are often treated specifically. The aim is either to increase the chances of recovery or - if the disease is too advanced - to alleviate or prevent symptoms (such as pain).
Depending on the location, size and number of the metastases, surgical removal and / or irradiation (radiation therapy) are recommended. The latter can under certain circumstances (e.g. with some brain metastases) also be carried out as stereotactic radiotherapy. The malignant tumor is irradiated very precisely from different angles with high intensity.
Supportive therapy
Kidney cancer symptoms and other consequences of the cancer or cancer therapy are specifically treated as required. Examples:
Painkillers (analgesics) help against tumor-related pain. Paracetamol or ibuprofen may be sufficient for mild pain. If the pain is moderately severe, the doctor will prescribe a weak opioid pain reliever such as tramadol. In the case of severe tumor pain, strong opioid pain relievers such as morphine must be used.
This pain therapy can sometimes be usefully supplemented with other drugs (co-drugs such as muscle relaxants).
If you have anemia as a result of cancer or cancer therapy, you may need blood transfusions.
Cancer patients in general often suffer from pronounced exhaustion (fatigue). On the other hand, experts recommend individually adapted endurance training as part of exercise therapy.
Kidney cancer patients with bone metastases should receive drugs to prevent bone fractures - bisphophonate or the monoclonal antibody denusomab in combination with calcium and vitamin D.
Kidney cancer: disease course and prognosis
Most of those affected are primarily interested in one question: Can kidney cancer be cured? In fact, the prognosis for the most common form - renal cell cancer - is relatively favorable compared to many other forms of cancer.
In individual cases, however, the chances of recovery depend on the one hand on how large the tumor on the kidney is and how far it has spread at the time of diagnosis. The following applies: the earlier diagnosis and treatment, the better the prognosis for kidney cancer.
The chances of recovery and life expectancy also depend on the type of kidney cancer. As mentioned, the vast majority of patients have renal cell cancer of the clear cell type. As long as it is still limited to the kidneys, this tends to have a somewhat poorer prognosis than other types of renal cell carcinoma in the localized stage.
The patient's age and any concomitant diseases also have an influence on the chances of recovery from kidney cancer (renal cell cancer).
Kidney cancer: aftercare and rehab
Even after kidney cancer treatment is complete, patients are not left alone. Aftercare and rehab are the next steps.
Aftercare
Attending the recommended follow-up examinations after kidney cancer is very important.The check-up appointments serve, among other things, to detect a possible relapse (relapse) of kidney cancer as well as (new) metastases at an early stage. It is also important to keep an eye on the patient's kidney function.
The follow-up examinations routinely include a doctor-patient conversation (anamnesis), physical and laboratory examinations as well as an imaging examination of the abdomen and, if necessary, chest (ultrasound and / or computed tomography or magnetic resonance imaging).
How often and for how long a kidney cancer patient is invited to follow-up examinations depends largely on their risk of relapse (low, medium, high). In principle, several follow-up appointments over a period of several years are recommended. Initially, they are set at shorter intervals (e.g. at three months), later at longer intervals (annually).
Rehabilitation after kidney cancer
After a kidney cancer illness, an individually adapted rehabilitation (rehab) is recommended. It is intended to help patients cope with the consequences of the disease and its treatment and to regain physical and mental fitness for a return to everyday life and possibly professional life.
How a rehab program looks in detail depends on the needs of the patient. However, building blocks from a wide variety of disciplines are incorporated, for example from medicine, psychology, physiotherapy, occupational therapy and sports therapy.
Doctors in rehab take care of existing side effects of cancer therapy, such as nerve damage caused by surgery (e.g. with electrotherapy). Psychological individual and group discussions as well as learning relaxation techniques can be helpful in getting emotional consequences such as fears, depression or dejection under control. Physical fitness can be increased with adapted exercise therapy. Heat packs, nutritional advice and social counseling (such as returning to work) can also be part of the diverse range of rehabilitation after kidney cancer.
Kidney cancer: how to deal with the disease
Kidney cancer is a serious disease. Dealing with it and the treatment demand a lot of mental and physical strength from you as a patient. You can help on various levels to cope with this difficult time as well as possible.
Kidney Cancer & Diet
A special diet for kidney cancer is generally not necessary. However, a healthy, balanced diet with sufficient amounts of water is generally advisable in order to promote general health and support the immune system. This can also help to cope better with the often stressful cancer therapy.
Your doctors will keep track of your nutritional status while you are being treated for kidney cancer. In this way, you can counteract an existing or threatened nutrient deficiency. Nutritional advice or nutritional therapy can then be helpful - possibly even after the treatment has been completed as part of the rehabilitation.
Kidney cancer patients who suffer from kidney failure (kidney failure) must pay particular attention to their own diet - either independently of the cancer or as a result of cancer therapy. In the long term, you have to be careful not to consume too much protein - its breakdown could put too much strain on the weakened kidney (s). A nutritionist can provide advice on making the necessary dietary changes.
In principle, kidney cancer patients should also avoid excessive alcohol consumption.
Kidney Cancer & Exercise
Sport and exercise are not only good for the body, but also for the soul. Therefore, if possible, care should be taken to ensure that kidney cancer patients begin physiotherapy and exercise training while they are receiving cancer therapy. In rehab, targeted and individually tailored physical activity should be continued on a regular basis.
For example, exercise therapy based on endurance, strength and / or coordination can be useful. Activities such as swimming, Nordic walking and treading water can also increase physical fitness and rebuild muscles that have been lost as a result of kidney cancer disease and therapy.
During rehab, patients also receive tips for future training at home.
Kidney Cancer & Psychological Support
Many patients and their families have problems coping with serious illnesses such as kidney cancer. Diagnosis alone can be a heavy burden. Added to this are stresses and worries during the time of cancer therapy and aftercare.
Professional support from psycho-oncologically trained specialists can help in such cases. Such professionals focus on the psychological and physical effects of cancer and help those affected to cope better with it.
According to experts, cancer patients and their relatives should have the opportunity to take advantage of psychosocial counseling and treatment during the entire illness and therapy phase. If necessary, speak to your doctor about it! He can discuss worries and fears with you and / or provide you with suitable professional contacts.
Kidney Cancer & Complementary Therapy
Some kidney cancer patients hope for additional help from complementary healing methods. They can improve well-being and quality of life and generally strengthen body and soul. As a rule, however, they cannot do anything against the cancer itself. Some examples of such procedures that are sometimes used for kidney cancer (cancer in general):
- acupuncture
- homeopathy
- Mistletoe therapy
- Hyperthermia
If you would like to use such methods as a supplement - that is, as a complement - to conventional ("conventional") kidney cancer therapy, you should speak to your doctor first. He can point out possible risks and interactions.
However, they are not suitable as alternative healing methods - cancer experts urgently advise against using acupuncture & Co. as a substitute for conventional kidney cancer treatment.
There are no generally established definitions for "complementary medicine" and "alternative medicine". The two terms are sometimes used synonymously. In general, however, complementary therapies differ from alternative therapies in that they do not question the value and approach of conventional medicine ("orthodox medicine"), but consider themselves to be complementary to it.
Tags: unfulfilled wish to have children diet alcohol













.jpg)

.jpg)