Lyme disease
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Lyme disease is the umbrella term for a group of bacterial infectious diseases. Borrelia are the trigger. Relapsing fever and Lyme borreliosis mainly belong to this group. However, the term borreliosis is often equated with Lyme borreliosis: It is the only disease caused by Borrelia in Europe. Here you can find out everything you need to know about the routes of infection, symptoms and treatment of Lyme disease.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M01G01A68
Brief overview
- What is Lyme disease? Bacterial infection transmitted by tick bites, mostly in the warm season. Incubation period: Days, weeks and months pass from the bite to the onset of the first symptoms
- Distribution: Everywhere in wooded and plant-populated Europe and North America
- Symptoms: extensive, often rounded skin reddening ("wandering reddening"), flu-like symptoms with headache, body aches, fever; Paralysis, paralysis, nerve pain in neuroborreliosis; Inflammation of the joints (Lyme arthritis); Inflammation of the heart muscle (Lyme carditis)
- Diagnostics: evidence of blood and / or nerve water tests (CSF test); rarer samples from joints and skin
- Treatment: with antibiotics for several weeks
- Prevention: skin inspection after all outdoor activities, early and professional removal of the tick
Lyme disease: description
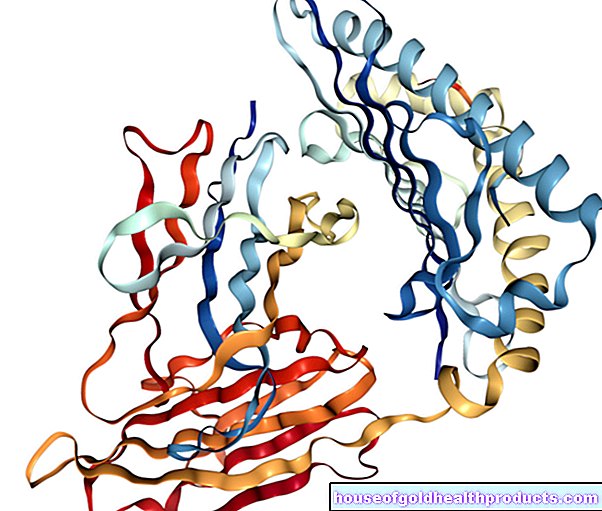
Borreliosis diseases are caused by agile, helical bacteria: Borrelia. They attack humans and other mammals. Blood-sucking insects serve as carriers. The bacteria can only get into the skin of other living beings through the stings of these parasites.
With us, in the vast majority of cases, borreliosis is transmitted through a tick bite (not a tick bite), namely through the bite of the common wood buck (Ixodes ricinus). Occasionally, living beings are also infected by other bloodsuckers such as horseflies, mosquitoes or fleas. There is no direct infection from person to person.
The most common Borrelia disease in humans is Lyme disease. It occurs almost worldwide in the temperate climatic zones and thus also in our latitudes. In the tropics and subtropics, other forms of Borrelia disease are also common, such as lice or tick relapsing fever. It is rarely brought to Germany by travelers or refugees.
Lyme disease
Lyme disease (also called Lyme disease) is the most common tick-borne disease in Europe. It is triggered by certain closely related Borrelia, all of which are part of the species complex Borrelia burgdorferi sensu lato (Bbsl) counting.
How many ticks in an area are infected with Borreliosis pathogens varies widely over a small area - the infection rate fluctuates between five and 35 percent. And when an infected tick bites a person, it does not always transmit Borrelia. Even after transmission, only a small proportion of those infected actually develop Lyme disease (a good one percent).
The prognosis for patients depends to a large extent on rapid treatment: Lyme borreliosis detected and treated at an early stage usually heals completely. Under certain circumstances, however, the disease can lead to serious complications, secondary diseases and long-term damage.
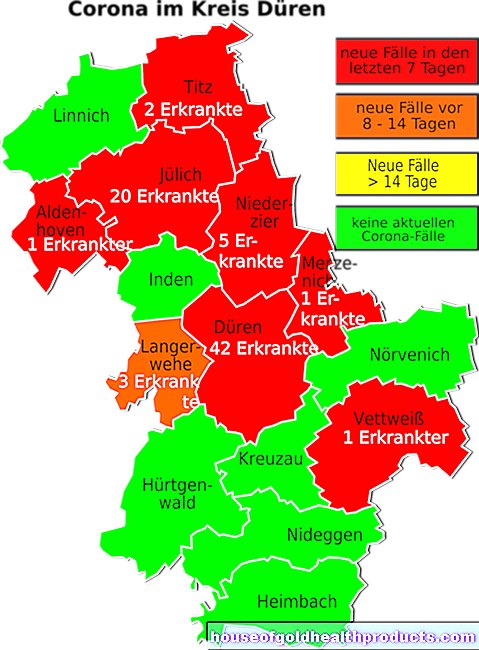
Lyme disease: occurrence
There are no typical Lyme disease areas, as we know it from the TBE (early summer meningo encephalitis). Borreliosis occurs in all wooded and plant-covered areas in Europe and North America.
Since ticks cause Lyme disease in humans, there is a seasonal increase in the disease - ticks depend on warm weather (the common wood tick becomes active from around 6 ° C). So in this country you can get infected with Lyme borreliosis, especially between April and October (earlier or later in the year if the weather is warm). Most infections occur in the summer months.
Lyme disease: incubation period
It usually takes days to weeks between the tick bite and the appearance of the first symptoms of Lyme disease. "Incubation period" is what doctors call this period between infection and the outbreak of disease.
About half of the sick develop a typical reddening of the skin called "wandering redness", medically called erythema migrans. Their incubation period averages seven to ten days. In infected people who do not develop "wandering redness", the disease often only becomes noticeable weeks after infection with general symptoms such as fatigue, swollen lymph nodes and a slight fever.
In addition, there are patients who show signs of organ involvement only weeks to months, sometimes years after the infection. These include changes in the skin (acrodermatitis chronica atrophicans) or painful inflammation of the joints (Lyme arthritis).
Borreliosis signs of the nervous system (neuroborreliosis) or the heart (Lyme carditis) usually only appear a few weeks after the infectious tick bite.
Because the incubation time with Lyme disease can be relatively long, some patients can no longer remember the tick bite. Often this was not even noticed.
Lyme disease: symptoms
A Lyme disease can express itself in many ways. Many people with Lyme disease initially show no symptoms at all. Others develop reddening of the skin at the puncture site, which slowly gets bigger. Doctors speak of erythema migrans, the "wandering red". In addition, flu-like symptoms can occur, such as headache and body aches as well as fever.
Wandering redness
After a tick bite, the Borrelia spreads in the tissue. Under certain circumstances, they then spread through the blood in the body and thus affect various organs. In this way, skin reddening occurs elsewhere as well.
In some cases, the infection spreads to the nervous system. Then neuroborreliosis develops (see below). Borrelia rarely affects other body organs such as the heart.
Long-term effects include chronically inflamed, painful and swollen joints (Lyme arthritis) or progressive skin changes (acrodermatitis chronica atrophicans).
You can read more about the typical signs of Lyme disease and possible long-term effects in the article Lyme Disease Symptoms.
-
Don't be afraid of Lyme disease
Three questions for
Prof. Dr. med. Heidelore Hofmann,
Specialist in dermatology and allergology -
1
Prof. Hofmann, what to do if a tick has bitten itself?
Prof. Dr. med. Heidelore Hofmann
First of all: don't panic! Studies show that Borrelia only migrate from the midgut of the tick to the host after about ten hours. Nevertheless, remove the tick as soon as possible and preferably with a tick card or tongs, without squeezing the body. The second step is then to observe the puncture site.
-
2
What can indicate an infection with Borrelia?
Prof. Dr. med. Heidelore Hofmann
Reddening of the puncture site that appears shortly after removing the tick and then disappears is harmless. Skin reactions that only show up a few days later, on the other hand, are typical of a Borrelia infection. Very often this is a ring-shaped reddening that spreads more and more - the so-called wandering reddening.
-
3
When should you go to the doctor?
Prof. Dr. med. Heidelore Hofmann
If you notice a skin change of any kind within six weeks of a tick bite - it doesn't always have to be your typical ring! Or if you feel sick like the flu without having cold symptoms such as runny nose or cough. Then a doctor should clarify a possible infection with Borrelia.
-
Prof. Dr. med. Heidelore Hofmann,
Specialist in dermatology and allergologyProf. Dr. med. Heidelore Hofmann is the coordinator of the AWMF guideline "Cutaneous Lyme Borreliose", former senior physician at the Department of Dermatology and Allergology at the Technical University of Munich and the Lyme disease consultation hour.
Neuroborreliosis
Neuroborreliosis develops when the Borrelia attack the nervous system. Often the nerve roots of the spinal cord become inflamed (radiculitis), causing excruciating, burning nerve pain. They are especially noticeable at night.
In addition, neuroborreliosis can be associated with flaccid paralysis (for example in the face) and neurological deficits (sensory disorders in the skin). Children in particular often get meningitis.
Neuroborreliosis is usually curable. In severe cases, however, damage can remain. Neuroborreliosis is very rarely chronic, with the central nervous system (brain, spinal cord) typically inflamed. Those affected increasingly suffer from gait and bladder disorders.
You can read everything you need to know about symptoms, diagnosis and treatment of neuroborreliosis in the article Neuroborreliosis.
Lyme disease: causes and risk factors
The pathogens of Lyme borreliosis are bacteria from the species group Borrelia burgdorferi sensu lato. Ticks transmit these Borrelia to humans. There is no direct infection from person to person. That is why nobody is contagious with Lyme disease! Or to put it another way: Sick people are not contagious!
Ticks transmit borreliosis pathogens
The older a tick is, the higher the risk that it will carry borreliosis pathogens. Because the tick first has to infect itself with the bacteria: It infects small rodents and other forest dwellers that carry the Borrelia. The bacteria themselves do not make the tick sick, but survive in its gastrointestinal tract.
Ticks live particularly on grass, leaves and bushes. From there, she can hold on to people (or an animal) passing by in a flash. It then migrates to warm, moist and dark areas of the body to suckle blood. The armpits and the pubic region, for example, are particularly popular. However, ticks can also attach themselves to any other part of the body.
Does the Lyme disease infection take place immediately?
While a tick is now sucking blood on a person, it can transmit the Borrelia. But that doesn't happen right away, but only after several hours of vacuuming. The Borrelia are located in the tick's intestine. As soon as this begins to suck, the bacteria migrate into the tick's salivary glands and then enter the body of the stung with the saliva.
A lower time limit for the act of sucking, from which a Lyme disease infection can be expected, cannot be reliably specified - also because the probability of Borrelia transmission varies depending on the Borrelia species. It is generally assumed that the risk of Lyme disease is low if an infected tick has sucked on a person for less than 24 hours. If the blood meal lasts longer, the risk of borreliosis transmission increases.
Lyme disease: examinations and diagnosis
Tick bite - yes or no? The answer to this question is an important clue for the doctor. Since the first symptoms of Lyme disease often only appear weeks or months after the infection, many patients no longer remember the tick bite or have not even noticed it. You can then at least tell the doctor whether it was possible: Anyone who often walks in forests or meadows or pulls weeds in the garden can easily catch a tick.
In addition to the possibility of a tick bite, the doctor is also interested in the patient's precise complaints: The "wandering redness" is particularly meaningful in the early stages of the disease. You should also inform your doctor about general symptoms such as headaches and body aches. In later stages of the disease, patients often report persistent joint or nerve pain.
The suspicion of "borreliosis" can finally be confirmed by laboratory tests. The doctor can look for antibodies against Borrelia in a blood or nerve water sample (in neuroborreliosis). However, the interpretation of such laboratory results is not always easy.
You can read more about the diagnosis of Lyme disease in the article Lyme Disease Test.
Lyme disease: treatment
Borrelia can be fought like other bacteria with antibiotics. The type, dose and duration of use of the medication depend primarily on the stage of Lyme disease and the age of the patient. For example, adults in the early stages of the disease are usually given tablets with the active ingredient doxycycline. In contrast, this antibiotic must not be used in children under nine years of age (i.e. before the enamel formation is complete) and pregnant women. Instead, the doctor prescribes amoxicillin, for example.
In later stages of the disease (chronic neuroborreliosis, etc.), doctors often also use antibiotics such as ceftriaxone or cefotaxime. The medication is usually given as a tablet, but sometimes also as an infusion via the vein (e.g. ceftriaxone).
The success of antibiotic therapy depends particularly on the start of treatment: In the early phase of Lyme disease, the treatment is usually more effective than in the later stages.
You can read more about the treatment of Lyme disease in the article Borreliosis Therapy.
Borreliosis: disease course and prognosis
It is very important to start therapy quickly with Lyme disease. The course and prognosis of the disease are significantly influenced by whether the bacteria have had time to spread and multiply in the body. With the right treatment, the symptoms usually resolve completely.
Under certain circumstances, however, signs of Lyme disease persist. Sometimes patients have mild facial nerve palsy for life. Other sufferers have dragging joint pain. A reaction of the immune system that lasts beyond the infection causes inflammation here.
Early signs are often missing or go unnoticed, which is why Lyme disease is recognized and treated later. The treatment of Lyme disease in such advanced stages of the disease is always difficult. Sometimes a further dose of antibiotics is required.
The experts in the medical guidelines do not recommend months of antibiotic therapy, repeated repetitions or combinations of several active ingredients!
In some cases, people become infected without developing any clear signs of the disease. Antibodies against Borrelia can be detected in around one in five Germans over the age of 70 - in most cases without a previous illness. The infection heals independently and with the help of the immune system.
Borreliosis, once overcome and healed spontaneously or under therapy, does not offer any immunity. This means that you can later become infected with Lyme disease and get sick from it.
Post Lyme Disease Syndrome
Post-borreliosis syndrome is particularly popular in health magazines and the media. However, there is no clear definition that describes this clinical picture. The media report on patients who complain, for example, of muscle pain, fatigue, lack of drive or difficulty concentrating.
However, previous studies indicate that these unspecific complaints do not occur more frequently than is generally the case in people with a previous Borrelia infection. Therefore, many experts doubt that the supposed "post-borreliosis syndrome" is actually related to Lyme disease.
Well-known long-term effects of a Borrelia infection are persistent skin changes (acrodermatitis chronica atrophicans), joint inflammation (Lyme arthritis) or neurological complaints (chronic or late neuroborreliosis).
If you suffer from post-Lyme disease symptoms, it is advisable to investigate other possible causes of these symptoms. For example, the reason for chronic fatigue or poor concentration can be a virus infection or even a hidden depression. Then the doctor can initiate appropriate treatment.
Lyme disease & pregnancy
Earlier case reports and small studies initially suggested that Borrelia infection during pregnancy interfered with child development. However, recent studies have not yet confirmed this assumption.
However, there is no evidence to unequivocally rule out the harmful effects of infection in pregnancy. That is why the doctor also consistently treats Lyme disease during pregnancy with antibiotics. To do this, he chooses active ingredients that do not harm the mother or the unborn child.
According to the current state of knowledge, women who have already had Lyme disease and were treated accordingly before becoming pregnant do not have to worry.
In addition, there is no evidence that mothers can transmit Lyme disease through breastfeeding.
Lyme disease: prevention
Ticks offer the only starting point for protection against Lyme disease: Prevent tick bites or remove a tick that is already sucking as quickly as possible. The following tips apply to this:
If you are out and about in forests and meadows or doing gardening, you should wear light-colored (white) clothing whenever possible. Ticks are easier to spot on it than on dark textiles. The arms and legs should also be covered by clothing so that the small bloodsuckers do not easily come into contact with the skin.
You can also apply tick or insect repellants. Please note, however, that these do not offer 100% protection against a tick bite and are only effective for a few hours.
Avoid short cuts through tall grass and bushes. Instead, stay on paved paths.
In any case, after being outdoors, you should thoroughly check your entire body for ticks. Also, check your pets for possible ticks: the parasites could spread to you from your cat or dog.
If you find a sucking tick on your skin, you should remove it immediately and professionally: Grasp the tick directly above the skin with fine tweezers or tick pliers and pull it out slowly and without twisting. Press as little as possible so as not to force body fluids from the animal into the wound. Also, check that you have not accidentally torn the body off while the parasite's head is still in the wound.
If you try to poison or suffocate a tick that is sucking on the skin with oil or other substances, you increase the risk of infection! Because in the struggle for survival, the tick may transmit even more Borrelia.
You should then disinfect the stab wound. Although this does not protect against Lyme disease, it does prevent wound infection.
Taking antibiotics as a precaution after a tick bite (without diagnosing a Lyme disease infection) is not recommended.
There is no Lyme disease vaccination!
Doctors can vaccinate against early summer meningoencephalitis (TBE), which is also transmitted by ticks. It is particularly advisable for those who live in or travel to risk areas. However, there is no preventive vaccine against Lyme disease.
Additional information:
Guidelines:
- S2k guideline "Cutaneous Lyme Borreliosis" of the German Dermatological Society (as of 2016)
- S1 guideline "Neuroborreliosis" of the German Society for Neurology (status: 2018)
Self-help groups:
Borreliose- und FSME-Bund Deutschland e.V. - Federal Association of Borreliose Self-Help
https://www.borreliose-bund.de
Federal Association of Tick Diseases e.V.
Werrastrasse 60, 64625 Bensheim, Germany
https://www.bzk-online.de/
Tags: alcohol drugs baby toddler gpp