Dysphagia
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.The term dysphagia stands for any type of swallowing disorder. A number of diseases can lead to painful or painless dysphagia, for example infections, malformations and chronic or malignant diseases. Damage to the nervous system, such as a stroke, can also trigger dysphagia. Read everything you need to know about the symptom of dysphagia: definition, causes, therapy.

Dysphagia: description
With dysphagia, the act of swallowing is disturbed. A healthy act of swallowing occurs in three phases:
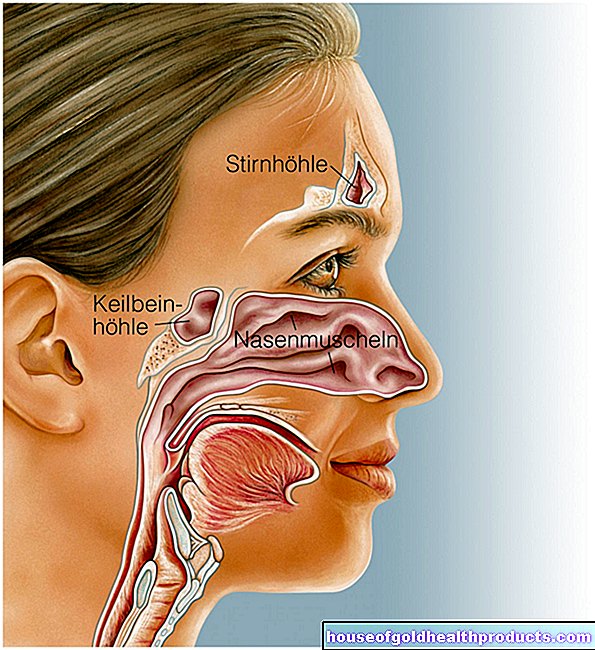
In the oral cavity (oral phase) the food is chopped up, mixed and mixed with saliva (moisture and digestive proteins). The tongue finally transports the pulp towards the throat, and the actual swallowing movements are triggered (swallowing reflex).
In the pharynx (pharyngeal phase), the muscles in the pharynx wall transport food in a targeted manner to the esophagus. The entrance to the trachea in front of it is closed by the epiglottis and vocal folds so that one does not "choke" and food residues get into the lungs. Conversely, the entrance to the esophagus is blocked by the upper esophageal sphincter when breathing and speaking.
In the esophagus, the porridge is transported down to the stomach by uniform muscle waves in the wall muscles (esophageal peristalsis) (esophageal phase). As a result, food or liquids reach the stomach even when lying down, i.e. without the help of gravity. To do this, the lower sphincter opens at the end of the esophagus. When it is closed again, the act of swallowing is ended.
The swallowing process is controlled by special centers in the cerebrum and brain stem.
Dysphagia, odynophagia, and aphagia
In most cases, the term dysphagia is used to refer to any type of swallowing disorder. More precisely, dysphagia describes painless problems during the swallowing process, which mean that food or liquid can no longer be transported properly to the stomach. If those affected feel pain, doctors speak of odynophagia. If swallowing is no longer possible at all, patients suffer from so-called aphagia.
In addition, dysphagia is divided into two main types: oropharyngeal dysphagia and oesophageal dysphagia.
Oropharyngeal dysphagia
In this type of dysphagia, swallowing disorders usually occur in the throat area and the mixture of food and liquid cannot be swallowed into the esophagus. It either flows back into the mouth, nose and throat (regurgitation) or gets into the trachea and lungs (aspiration). A strong urge to cough then usually pushes the porridge back up. However, if it remains in the lungs, inflammation can occur there (aspiration pneumonia).
Esophageal dysphagia
The responsible disorder lies in the area of the esophagus. Patients typically report that they feel the food “slip through” or “get stuck” in the chest area (feeling of pressure).
A possible cause of oesophageal dysphagia is a tissue overgrowth that steadily narrows the esophagus. If the esophageal opening is less than 13 millimeters wide, patients complain of dysphagia when eating solid foods. If it is less than five millimeters wide, liquids can hardly get through.
Stuck components can completely close the esophagus (bolus obstruction). Patients complain of severe pain or burning behind the breastbone and unpleasant salivation (not even the saliva can be swallowed).
Further dysphagia
The risk of swallowing disorders naturally increases with age. The reason: the connective tissue and also the muscles become weaker over the years. The swallowing reflex is often only triggered with a delay. Numerous medications and previous illnesses can also have negative effects. As a result, some patients can no longer adopt the correct posture for eating and drinking.
If the swallowing disorders are solely due to the aging process, doctors speak of presby dysphagia. In the broadest sense, it can be counted as part of what is known as functional dysphagia. Functional swallowing disorders can generally occur at any age. In this case, there are problems with swallowing, without an organic cause (such as cancer, nerve failure, inflammation) can be determined.
Frequency of dysphagia
According to the German Gastro League, around 80,000 to 160,000 people in Germany see their doctor every year because they suffer from new problems with the swallowing process. One in six of the over-65s is affected by dysphagia.
Dysphagia: causes and possible diseases
If the dysphagia is mainly when drinking, the cause is often the impaired neural control of the act of swallowing. The act of swallowing is regulated in higher-level centers of the brain, with the control signals being passed on to the respective muscles via a large number of nerves. A disorder in this area (e.g. as a result of a stroke) is called neurogenic dysphagia. Those affected also mostly choke.
In other cases, dysphagia is mechanical. For example, scarring as well as malignant and benign growths in the area of the esophagus can cause swallowing disorders.
Psychological factors can also play a role in the development of dysphagia.
Esophageal dysphagia
Oesophageal dysphagia is either caused by a disease of the esophagus itself or other diseases interfere with normal esophageal function.
|
Cause of dysphagia |
illness |
|
Disruption of esophageal movement |
Achalasia (chronic dysfunction of the esophagus) |
|
Esophageal spasm (simultaneous and increased contraction of the esophageal muscles) | |
|
Scleroderma (connective tissue disease with hardening of the esophageal wall) | |
|
eosinophilic esophagitis (immune-mediated chronic inflammation of the esophagus) | |
|
hypercontractile esophagus (excessively long, strong contractions of the esophagus muscles) | |
|
tumor |
Esophageal cancer |
|
Cardiac carcinoma (cancer of the stomach entrance) | |
|
Lung cancer, mediastinal tumor (growth in the middle of the chest) | |
|
Mesenchymal tumors such as the rare and malignant gastrointestinal stromal tumor (GIST) or muscle growths (myomas) | |
|
Inflammation |
Reflux disease |
|
Infections such as fungal infections (thrush), consumption (tuberculosis) | |
|
Crohn's disease (chronic inflammatory disease that can affect the entire digestive tract) | |
|
Protrusions of the wall of the esophagus (diverticulum) |
Zenker's diverticulum (protrusion of the back wall of the upper esophagus or lower throat; typically dysphagia with tenderness and gurgling noise when drinking) |
|
Diverticulum at the bifurcation of the windpipe (bifurcation diverticulum) or above the diaphragm (epiphrenal diverticulum) | |
|
Pseudodiverticulum (mucosal protuberance due to muscle gaps) | |
|
Malformations |
Atresia (malformation of the esophagus: the esophagus is usually only partially present and may have connections to the trachea) |
|
Vascular malformations such as dysphagia lusoria, in which the right clavicle artery pulls up behind the esophagus and constricts it in the process | |
|
Operations |
Fundoplication (operation of a reflux disease in the late stage, in which part of the stomach is wrapped around the esophagus and sutured) |
|
Vagotomy (cutting of the esophageal nerve vagus nerve) | |
|
miscellaneous |
Chemical burns with subsequent scarring of the esophagus |
|
Schatzki ring (narrowing of the lower esophagus by mucosal tissue as a result of a diaphragmatic hernia = hiatal hernia) | |
|
Plummer-Vinson syndrome (loss of the mucous membrane on the tongue, mouth, throat and esophagus as a result of iron deficiency; typical consequences are burning tongue and odynophagia) |
Oropharyngeal dysphagia
Oropharyngeal dysphagia is mostly neurogenic (neurological) and can be caused by various diseases. Some examples:
- stroke
- Parkinson's disease
- Multiple sclerosis (MS)
- Traumatic brain injury (TBI)
- viral or bacterial inflammation (such as borreliosis), tumors or degrading (degenerative) diseases in the central nervous system (CNS)
- Acute (inflammatory nerve disease), Miller-Fisher syndrome (rare variant of Guillain-Barré syndrome that affects the cranial nerves)
- Amyotrophic lateral sclerosis (ALS; chronic degenerative disease of the CNS) and progressive bulbar paralysis (special form of ALS)
- Myasthenia gravis, Lambert-Eaton syndrome (in both muscle weakness as a result of impaired nerve signal transmission)
- Botulism (severe bacterial poisoning)
- Muscular dystrophies (diseases that cause muscle wasting)
- Nerve damage (neuropathies), for example caused by the diabetes mellitus or alcohol
Of course, benign or malignant growths in the oropharynx can also lead to oropharynegal dysphagia. The biggest risk factors are nicotine and alcohol consumption.
Virus, bacterial, or fungal infections can also cause swallowing disorders. Tonsillitis and / or pharyngitis (tonsillitis / pharyngitis) and, in the advanced stages, an abscess (peri / retrotonsillar abscess) usually trigger odynophagia. If the defense system is directed against the body's own structures - for example against the vessels of the digestive tract in the case of vasculitis - problems can also arise during the swallowing process.
In addition, a greatly enlarged thyroid (goiter, “goiter”) can initially narrow the trachea and finally the junction between the pharynx and esophagus. A very dry mouth (xerostomia) also leads to dysphagia symptoms. Massive misaligned teeth and poor dentures also hinder the act of swallowing.
Ultimately, some drugs also cause dysphagia. In addition to anesthetics such as muscle relaxants, these include active ingredients against psychoses, Parkinson's disease, epilepsy and irritable bladder.
Consequences of dysphagia
The act of swallowing is a vital process with the help of which food and water are supplied to the body. Problems with the swallowing process can therefore have serious consequences. Dysphagia leads to malnutrition (malnutrition), especially in older patients. A lack of water causes dangerous dehydration (dehydration, desiccosis).
If porridge gets into the lungs and can no longer be coughed up properly, pneumonia is the result (aspiration pneumonia). This can be so intense that those affected die from it.
Dysphagia: when do you need to see a doctor?
There are always situations in which bites are difficult to swallow. This may be due to the fact that the food is not properly chopped up or - if swallowed quickly - has only been mixed with a small amount of saliva and is then difficult to "slide" down. However, if you suffer from painful dysphagia, you should consult a doctor. This also applies if the swallowing disorders occur more frequently or suddenly, are accompanied by a fever or do not improve.
Which doctor for dysphagia?
If you have difficulties getting the food to or into your esophagus, you should see an ear, nose and throat doctor (ENT). However, if the food feels stuck behind the breastbone or if you feel every bite "slide down", a gastrointestinal specialist (gastroenterologist) can help.
If you suffer from additional complaints or if you are not sure, a visit to your general practitioner or a resident specialist in internal medicine (internist) is advisable. If you feel noticeably weaker and dull and can barely lift your arms and legs, you probably have muscle weakness. In these cases, a neurologist should be consulted.
When not to postpone a visit to the doctor
Sudden swallowing disorders are always a warning sign. This is especially true if you also experience severe pain (in the chest area) or if you have temporarily lost consciousness. If, in addition to dysphagia, you can suddenly no longer move various parts of the body properly, this is an emergency and you should call an emergency doctor immediately.
Dysphagia: what does the doctor do?
The doctor first asks the patient and collects his or her medical history (anamnesis). The doctor also asks various questions in order to get initial information about the type and cause of the dysphagia. Some examples:
- How long have the swallowing disorders existed?
- Is Your Dysphagia Painful?
- Does the food or liquid often come out through the nose when trying to swallow?
- Did the swallowing problem occur suddenly?
- Do you suffer from other complaints besides dysphagia?
- Do you have any previous illnesses, such as reflux disease with heartburn?
- Do you sweat profusely at night?
- Have you been able to measure elevated temperatures at home?
The doctor will then do a physical exam. He pays particular attention to changes in visible areas of the digestive tract: He examines the oral cavity and the throat. He also examines the neck for possible swelling and checks the larynx.
In the so-called water swallow test, the patient is given a few milliliters of water to drink. Then he should speak. Among other things, the doctor pays attention to:
- Changes in the tone of your voice, for example seething
- The water escapes through the nose
- excessive gag reflex
- strong cough (as a sign of aspiration)
There are numerous checklists and scoring systems with which the doctor can record his examination results. The severity of dysphagia can be determined, for example, with the Gugging Swallowing Screen (GUSS). The swallowing process is checked with pulpy, liquid and solid food. For a more precise assessment, the doctor can also examine the act of swallowing with a movable probe (laryngoscope for fiberendoscopic swallowing examination FEES). In this way, he can also see whether parts of food get into the windpipe.
The doctor also scans the surrounding lymph node regions. Here, for example, cells of malignant growths can settle (lymph node metastases).
Reflection of the esophagus and stomach in dysphagia (EGD)
To rule out the exact cause of dysphagia, the doctor performs an esophagus and gastroscopy (esophagogastroduodenoscopy, EGD). During this examination, the esophagus, stomach and duodenum are examined from the inside with the help of a special probe. The patient is in twilight sleep. The probe (endoscope or gastroscope) is a thin, flexible tube with a tiny video camera attached to the end. The endoscope also has a lamp and a rinsing and suction device.
With this device, the doctor can assess the structures and especially (malignant) changes in the esophagus or stomach that can cause dysphagia. A so-called working channel also enables him to take tissue samples using forceps. In addition, it can also expand causes of dysphagia such as constrictions (bougienage). He obliterates excess tissue with the help of a laser or electricity.
If the reflection is normal, the doctor will carry out further tests to get to the bottom of the dysphagia.
Measurement of esophageal pressure in dysphagia
In some cases, there is no evidence of swallowing disorders in the ÖGD. Causes such as achalasia or an esophageal spasm can then be determined by what is known as an esophageal manometry. The pressure is measured at every inch of the esophagus. In this way, the movement sequences, i.e. the act of swallowing, can be represented.
In addition to movement disorders of the esophagus, malfunctions of the upper or lower sphincter muscle (pharynx-esophagus and esophagus-stomach) can also be detected by measuring the esophageal pressure.
The pressure measurement is carried out using a special plastic catheter under local anesthesia. This tube is soft, about five millimeters thick, and is inserted through the nose. The measurement takes about 20 minutes.
Impedance-pH-metry in dysphagia
The patient usually notices reflux disease through heartburn. But for proper treatment it is important to know what exactly flows back into the esophagus (reflux). This is often acidic gastric juice. Non-acidic fluids or bile from the intestines can also flow into the esophagus and cause discomfort there. In the esophagus, reflux can eventually inflame the mucous membrane, lead to constrictions and ultimately cause dysphagia.
The extent and type of reflux can be determined with the help of impedance pH metry. Here, too, the doctor inserts a special measuring probe through the nose into the esophagus. It remains there for about 24 hours. The measurement data registered by the probe are recorded on a storage device.
X-ray for dysphagia
Here the doctor takes an X-ray of the neck and chest. In the case of dysphagia, there is a special X-ray examination, the so-called swallow cinematography (X-ray swallow):
The patient is given a test food that contains an X-ray contrast medium. While swallowing he is constantly "x-rayed". The doctor can see which way the contrast agent pulp is taking on a screen. In addition, it can be determined whether the test food is stuck at a certain point, for example accumulates in a diverticulum, or whether the patient “chokes” (the chyme ends up in the windpipe).
Further examination methods for dysphagia
Depending on the cause of the dysphagia, additional tests may be helpful. Under certain circumstances, the doctor will arrange for an ultrasound examination using a gastroscope. In this way he can reveal subtle changes in the wall of the esophagus.
In the case of malignant growths, imaging using computer (CT) or magnetic resonance imaging (MRT) is useful. Doctors check whether other organs are also affected or whether the cancer is growing into neighboring body structures.
If the dysphagia is caused by diseases of the brain, nerves or muscles, a neurologist will carry out further tests, for example measuring the nerve conduction velocity.
This is how the doctor treats dysphagia
There are a number of different options for dysphagia therapy. Which treatment makes the most sense in each individual case and what the prognosis looks like depends primarily on the cause of the dysphagia.
For example, malignant growths are removed in an operation. Sometimes this is done in combination with radiation and chemotherapy (radiochemotherapy). Benign growths or inflammation-related changes in the esophagus can usually be treated as part of an esophagectomy. For example, lasers, stents or inflatable balloons are used.
In certain cases, drugs are prescribed for dysphagia: some substances support or strengthen the movements of a weak esophagus (prokinetics). Anticonvulsants (antispasmodics) help against excessive muscle contractions in the digestive tract, painkillers against odynophagia. In the case of reflux disease, active substances that inhibit gastric acid (proton pump inhibitors, antacids) can prevent the development of dysphagia if used in good time.
Special exercises against swallowing disorders can help if these have existed since birth or after a stroke and cannot be reversed by surgical measures. This should enable those affected to eat and drink safely again. The aim is not only to ensure successful nutrition, but also to protect the respiratory tract.Those affected learn the exercises for dysphagia from specially trained therapists, such as speech therapists or speech therapists. Among other things, posture, tension and breathing behavior are trained.
Under certain circumstances, the dysphagia is so pronounced that the patient - at least temporarily - has to be fed artificially via gastric tubes or venous catheters.
Dysphagia: What Can You Do By Yourself?
In the case of dysphagia, it is unfortunately not possible to prevent symptoms that arise. At least stopping smoking and alcohol significantly reduces the risk of malignant cancer. In general, if you suffer from dysphagia or heartburn, you should consult a doctor early on. He can then carry out targeted examinations and initiate appropriate therapy.
The doctor will also tell you what you can do yourself to relieve the difficulty swallowing (depending on the cause). If you have persistent reflux symptoms, for example, you should fall asleep at night with your upper body elevated (around 20 degrees) and, if possible, on your left side.
In general, you should chew (preferably small) bites for a long time. As a result, the food is sufficiently chopped up and mixed with sufficient saliva. In this way you make the swallowing process easier, add digestive proteins to the chyme at an early stage and reduce the risk of overeating.
For some dysphagia patients, it is helpful to puree or pass the food. If there are swallowing problems, especially with liquids, you can thicken them with a special powder (available in drugstores, pharmacies or on the Internet).
Dysphagia diet
There is no special dysphagia diet. However, you should avoid dry, coarse-grained, grainy or sticky products. If you are not sure about a dish, test it when someone is around.
|
food |
suitable |
rather unsuitable |
|
meat and sausage |
fine meat such as poultry, sausages, meat loaf (depending on the preparation also pork, beef or veal); tofu for vegetarians |
dry or breaded meat, meat or sausage with large portions such as nuts, peppercorns or the like; for vegetarians, crumbly, chopped soy products |
|
fish |
Fillet and soft cooked fish |
whole fish (always watch out for bones!), breaded fish |
|
cheese |
especially sticky processed cheese or chunky additives such as nuts, herbs or pepper | |
|
Eggs |
Scrambled eggs or soft-boiled eggs |
hard-boiled eggs with crumbly yolks, crispy fried eggs |
|
Sweets |
Fruit puree, fine pudding, ice cream, creams, honey |
Nut nougat, jams with pieces, pralines |
|
Cereals and potatoes |
Toast, large noodles, semolina, bread without grains and crust, mashed potatoes dumplings |
Rice, grainy bread, small noodles, dry cakes, crispy oat flakes, fried potatoes, croutons, chips |
|
vegetables |
rather soft-boiled vegetables such as cauliflower, spinach, carrots, zucchini, savoy cabbage; also avocado, tomato meat, cucumber meat |
fibrous vegetables such as rhubarb, asparagus, leek, sauerkraut; Legumes such as peas, beans, lentils, corn |
|
fruit |
Apple, pear, apricot, nectarine, peach, melon, banana (all raw, without seeds, possibly without skin) |
fibrous fruits such as pineapple, citrus fruits, berries (especially with seeds) |
|
milk |
All dairy products, except ... |
… Yoghurt or quark with pieces of fruit or coarse herbs |
|
beverages |
rather thick juices and thick, still water |
carbonated or alcoholic beverages |
Of course, the exact selection of products depends on the cause of the dysphagia. Food intake should be facilitated by the right and appropriately prepared food. It also reduces the risk of aspiration (swallowing) and the associated dangerous secondary diseases such as pneumonia.
Always take dysphagia seriously!
In any case, swallowing disorders should always be taken seriously. Consult a doctor early on. Do not be afraid of medical interventions to clarify your complaints. A gastroscopy or other dysphagia examinations are usually safe and quick. Follow the therapeutic measures and recommendations of the doctor or therapist. In this way you reduce the problems with the swallowing process and can possibly completely eliminate the dysphagia.
Tags: fitness organ systems teeth