TBE
and Martina Feichter, medical editor and biologistFabian Dupont is a freelance writer in the medical department. The human medicine specialist is already doing scientific work in Belgium, Spain, Rwanda, the USA, Great Britain, South Africa, New Zealand and Switzerland, among others. The focus of his doctoral thesis was tropical neurology, but his special interest is international public health and the comprehensible communication of medical facts.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
TBE (early summer meningoencephalitis) is a meningitis or encephalitis, triggered by the TBE virus. This is transmitted through tick bites. TBE usually heals without consequences. But there are also patients who suffer from long-lasting symptoms (such as paralysis) or die of TBE. Read more about the topic here: What is TBE? Where are the TBE areas? What symptoms does TBE cause? How is TBE diagnosed and treated?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. Z24A84
Brief overview
- What is TBE? TBE stands for early summer meningoencephalitis. This is a virus-related acute inflammation of the meninges (meningitis) and possibly also of the brain (encephalitis) and the spinal cord (myelitis).
- Symptoms: Usually no symptoms or only flu-like symptoms. Otherwise symptoms depending on the spread of the inflammation in the central nervous system, e.g. fever, headache, stiff neck, photophobia, dizziness, nausea and vomiting, swallowing and speech disorders, paralysis, seizures, etc.
- Diagnostics: doctor-patient discussion (anamnesis), blood tests, taking and analyzing a nerve water sample (liquor puncture), possibly magnetic resonance imaging (MRI)
- Treatment: only possible symptomatically, for example with pain relievers and antispasmodics. In the case of neurological symptoms such as paralysis, physiotherapy, occupational therapy or speech therapy may be required. In severe cases, treatment in the intensive care unit.
- Prognosis: TBE usually heals without consequences. However, the more extensive the inflammation in the central nervous system, the more likely it will be severe and long-lasting symptoms (such as paralysis). The latter can also persist for life. About one in a hundred patients dies from TBE that affects the nervous system.
TBE: description
Early summer meningoencephalitis (TBE) is an acute inflammation of the meninges and often also of the brain and spinal cord. It is triggered by the TBE virus. In Germany, ticks almost always transmit TBE. This is why the disease is also called tick encephalitis. It is rarely transmitted through virus-infected raw milk from goats, sheep and - extremely rarely - cows. TBE infection from person to person is not possible.
TBE: Rare, but dangerous
Not every tick bite (colloquially: tick bite) leads to a TBE infection and not every infection leads to disease: in the risk areas of Germany, on average, only about 0.1 to 5 percent of ticks carry the TBE virus. On a small scale, however, the infection can fluctuate very strongly - in some areas up to 30 percent of all ticks carry the TBE pathogen.
When infected ticks bite people and transmit the virus in the process, only about a third of those affected actually develop clinically recognizable early summer meningoencephalitis (with symptoms such as headache, fever, etc.). Most infected people, on the other hand, show no symptoms at all.
However, one should bear in mind that the disease can be severe and even fatal: the healing process can take months. Sometimes permanent neurological impairments (such as difficulty concentrating) remain. TBE infestation of the nervous system leads to death in about one in a hundred patients.
TBE: frequency
In 2018, 583 TBE diseases were registered in Germany. The number of cases varies from year to year. For example, there were fewer than 200 TBE diseases in 2012, more than 540 in 2006 and more than 480 in 2017.
Mainly people become infected with TBE during leisure activities in nature, for example when camping or hiking. Most diseases are observed in spring and summer.
Children get tick bites more often than adults and are therefore generally more at risk of developing TBE. With them, however, the infection is usually mild and heals without permanent damage.
Do not confuse it with Lyme disease
TBE must not be confused with another tick-borne disease: Lyme borreliosis. This is a disease caused by bacteria (Borrelia). It occurs nationwide and is much more common than TBE: Up to 30 percent of ticks in Germany carry the borreliosis pathogen (the infection can vary over a small area but can vary widely). Borreliosis is easily curable if diagnosed in good time.
TBE: symptoms
If TBE viruses were transmitted in a tick bite, it takes some time before the first symptoms appear: the pathogen must first spread through the body and reach the brain. On average, it takes about one to two weeks between infection (tick bite) and the onset of the disease. This period of time is called the TBE incubation period. In individual cases, it can take up to 28 days for early summer meningoencephalitis to break out.
Two-phase course of the disease
In most patients, TBE runs in two phases:
The first signs of TBE are flu-like symptoms such as a general feeling of illness, fever, headache and body aches. Occasionally, there is also abdominal pain. The symptoms are often dismissed as a cold or flu. After about a week the symptoms will subside and the fever will decrease again.
In a small proportion of patients, the fever rises again after a few days. It marks the beginning of the second phase of the disease. This is expressed as follows:
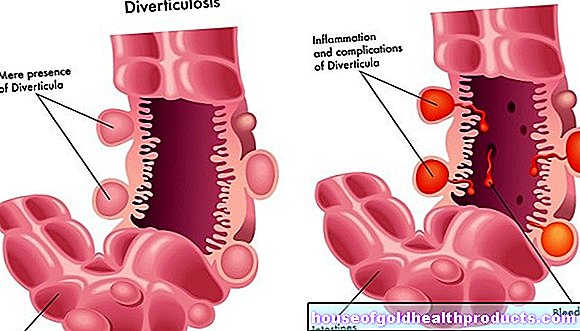
- Isolated meningitis develops in around 50 percent of patients.
- In around 40 percent of patients, meningitis is accompanied by inflammation of the brain (encephalitis). Doctors then speak of meningoencephalitis.
- In around ten percent of patients, the spinal cord is also inflamed. Then it is meningoencephalomyelitis.
- Very rarely, the inflammation in TBE is limited to the spinal cord alone (myelitis) or to nerve roots that arise from the spinal cord (radiculitis).
70 to 95 percent of all TBE-infected people show no symptoms (asymptomatic infection) or the second phase of the disease does not occur.
The exact symptoms of TBE in the second stage depend on the spread of the inflammation:
TBE symptoms in isolated meningitis
In the case of pure meningitis (meningitis), the symptoms of TBE do not differ significantly from those of other viral meningitis. However, they are often more pronounced: The patients complain of a severely impaired general condition as well as fever, fatigue and headache. Rigid neck and the associated photophobia are of particular diagnostic relevance. These are typical signs of meningitis. TBE can also cause symptoms such as dizziness, vomiting and nausea.
TBE symptoms in meningoencephalitis
If, in addition to the meninges, the brain is also affected by the inflammation (meningoencephalitis), further TBE symptoms appear: The focus is on a disorder of movement coordination (ataxia), impaired consciousness and paralysis of the arms, legs and cranial nerves. The latter can cause hearing, swallowing or speech disorders, for example. In addition, the inflammation of the brain can also cause seizures.
TBE symptoms in meningoencephalomyelitis
The most severe TBE symptoms can occur in meningoencephalomyelitis, i.e. when the meninges, brain and spinal cord are inflamed at the same time. The spinal cord is the connection between the brain and the rest of the body. If inflammation occurs here, the consequences can often be seen all over the body:
Usually flaccid paralysis occurs in the arms and legs. Most of the time there are also swallowing and speech disorders as well as paralysis of the facial and neck muscles. Respiratory paralysis is one of the most feared TBE symptoms in this disease process. It can lead to death!
TBE symptoms in children
In children and adolescents, TBE usually only occurs with unspecific symptoms that are similar to those of a flu-like infection. Severe TBE symptoms are less common than in adults.In the young patients, the disease usually heals without any consequential damage.
Consequential damage from TBE
In most cases, TBE heals without any consequences. However, some patients continue to suffer for weeks or months from symptoms such as headaches, tiredness, difficulty concentrating, seizures or paralysis. Often these complaints are only temporary. But they can also be permanent.
Severe disease progression and permanent damage from TBE occur particularly in older adults. They are almost never observed in children.
Double infection: TBE plus Lyme disease
TBE viruses and Lyme disease bacteria are rarely transmitted at the same time as a tick bite. Such a double infection is usually severe. Those affected can suffer permanent neurological damage.
Vaccination against TBE
There is a vaccine against early summer meningoencephalitis. This is a dead vaccine: it consists of inactivated pathogens that can no longer cause disease. Nevertheless, they stimulate the immune system to produce specific antibodies against TBE viruses. These then prevent a "real" TBE infection in the long term.
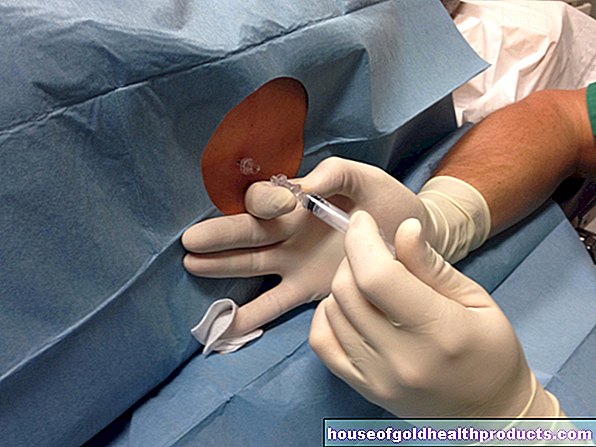
To build up this vaccination protection (basic immunization), three vaccinations are necessary: Depending on the vaccine and age, certain intervals are recommended for the administration of the three vaccine doses. Three years after completing the basic immunization, the TBE vaccination should be refreshed with a single dose. The further booster vaccinations should normally be given every five years. From the age of 50 or 60 (depending on the vaccine), refreshment is recommended every three years.
Experts recommend the TBE vaccination on the one hand to all people who live in TBE risk areas (see below), as well as to certain professional groups (foresters, hunters, etc.). On the other hand, the vaccination makes sense for travelers to TBE areas if there is a possibility of TBE infection (for example during planned hiking tours).
You can find out more about the effects and side effects of vaccination against early summer meningoencephalitis in the article TBE vaccination.
TBE areas
In Germany, TBE occurs mainly in Bavaria, Baden-Württemberg, Hesse, Lower Saxony, Thuringia, Rhineland-Palatinate, Saarland and Saxony. TBE viruses are also found sporadically in other federal states such as Brandenburg, Berlin, North Rhine-Westphalia and Saxony-Anhalt. Only in Bremen and Hamburg has nobody contracted TBE so far.
TBE high risk areas
There is also the possibility of TBE transmission in many other countries, for example in Austria, Switzerland, the Czech Republic, Hungary, Croatia, Poland, Sweden and Finland. In contrast, infection rarely occurs in Italy, France, Denmark and Norway.
You can find out more about the spread of TBE viruses at home and abroad in the article TBE areas.
TBE: causes and risk factors
The cause of early summer meningoencephalitis is an infection with the TBE virus. It belongs to the so-called flaviviruses such as the causative agents of dengue fever, Japanese encephalitis and yellow fever. In contrast to these tropical diseases, TBE is indigenous to Germany.
TBE viruses come in three subtypes: The Central European subtype is common here. The Siberian and Far Eastern subtypes occur in the Baltic States, on the coasts of Finland and in Asia. All trigger similar clinical pictures.
TBE: ways of infection
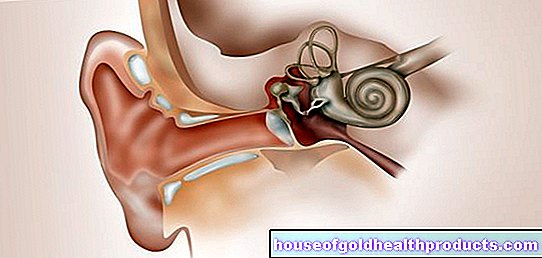
TBE is mainly transmitted to humans through tick bites. Ticks are parasites that feed on the blood of a host organism. They live mainly in forest and meadow areas up to an altitude of about 1,500 meters. They prefer warm and moist places. Ticks especially like to stay in tall grass and undergrowth: Adult ticks usually frolic at a height of 30 to 60 centimeters above the ground; they are rarely found at a height of up to 1.5 meters.
The ticks can "catch" the TBE pathogen when they suck blood from infected wild animals (especially small rodents such as mice). The animals carry the pathogen without developing TBE. If an infected tick bites a person during the next blood meal, it can use its saliva to introduce the TBE virus into the human bloodstream.
TBE is very rarely transmitted through virus-contaminated raw milk from sheep and sheep (less often from cows) and raw milk products made from it. This transmission route poses a risk of infection, especially in Eastern Europe, and is considered a rarity in Germany.
Direct transmission of TBE from person to person is not possible. That is why infected or sick people are not contagious!
TBE risk factors
All people who are outdoors a lot in a TBE risk area have an increased risk of TBE - for example in their leisure time (e.g. when hiking) or at work (hunters, foresters, forest workers, etc.). Overall, however, the probability of a TBE infection is low because - as mentioned above - only a small proportion of the ticks in risk areas carry the TBE pathogen.
How serious an infection will be in an individual case cannot be predicted. In most cases, TBE infection causes no or only mild symptoms. Serious courses rarely occur. Those affected are almost exclusively adults. Age plays an important role here: the older a patient is, the more often TBE takes a severe course and the more often it leaves permanent damage.
TBE: examinations and diagnosis
First, the doctor will have a detailed conversation with the patient in order to collect his medical history (anamnesis): In doing so, he will have the symptoms described in detail. In addition, the doctor asks about stays in a TBE risk area and possible tick bites in the previous weeks. However, many patients have already forgotten or not noticed the tick bite. The saliva of a tick contains, among other things, numbing substances, so that many people do not feel the tick bite. For the doctor this means: even if the patient cannot remember a tick bite, that does not rule out TBE.
After the anamnesis talk, blood tests are due: With TBE, various inflammation parameters are increased (number of leukocytes, sedimentation rate, CRP). In addition, specific antibodies against TBE viruses are searched for in the blood. Normally, specific IgM (immunoglobulin M) can be detected about two to four weeks after the tick bite. About one to two weeks later, specific IgG antibodies (immunoglobulin G) are also found in the patient's blood.
The diagnosis of TBE is established when both specific IgM and IgG are detectable in the blood, the patient shows the symptoms of the disease and is not vaccinated against TBE.
In rare cases, no specific IgMs are formed in a TBE infection, for example in the case of a weakened or drug-suppressed immune system. The diagnosis is then based on other parameters: The significant increase in specific IgG antibodies already provides a clear indication of the infection.
In addition, the doctor can take a sample of the cerebrospinal fluid (CSF) (CSF puncture). It is examined in the laboratory for specific antibodies and traces of the genetic material of the TBE virus. However, the viral genetic material is only detectable in the CSF during the first phase of the disease. Later, only the response of the immune system to the pathogen - in the form of specific antibodies - can be measured.
In some cases, the doctor will also take detailed images of the brain using magnetic resonance imaging (MRI). This is particularly helpful to differentiate encephalitis caused by TBE viruses from encephalitis caused by herpes simplex viruses.
TBE is notifiable. If an acute TBE is detected in a patient through direct virus detection (genetic material) or indirect virus detection (specific antibodies), the doctor must report this to the responsible health department (with the patient's name).
Examination of dead ticks?
There are companies that examine the ticks sent in for TBE viruses (or other pathogens). The idea behind it: if you discover a sucking tick on your own body, you can remove it and send it in for analysis. If symptoms develop, the test result should help the doctor make a diagnosis. But that doesn't make much sense for three reasons:
- Even if the tick is infected with the TBE virus, that does not necessarily mean that it has transmitted the pathogen to the patient.
- The methods used to detect TBE viruses (and other pathogens) in ticks vary in their sensitivity. Despite a negative test result (no TBE virus detectable in the tick), the tick can still be infected and have transmitted the virus.
- Even if the present tick does not actually carry any TBE virus - perhaps the patient was stung unnoticed by another tick, which was, however, infected.
TBE: treatment
There is no causal TBE treatment, i.e. no therapy that specifically targets the TBE virus in the body. One can only support the body in its fight against the pathogen. The aim is to alleviate the TBE symptoms and prevent long-term damage as far as possible.
For example, TBE patients should keep bed rest. If the TBE triggers seizures, the doctor prescribes antispasmodic agents. Painkillers such as ibuprofen, diclofenac, paracetamol or metamizole help against severe headaches. These remedies also have an antipyretic effect. However, a general reduction in fever is not recommended. The significantly higher temperature helps the body fight the TBE pathogens.
If the headache is very persistent, TBE patients are sometimes given opiates. These are powerful pain relievers, but they can be addictive. They are therefore only used when absolutely necessary and in a very controlled manner.
In the case of neurological disorders such as movement or speech disorders, physiotherapy, occupational therapy or speech therapy can be useful.
In the case of severe TBE (for example with impaired consciousness or respiratory paralysis), patients must be treated in the intensive care unit.
TBE: course of disease and prognosis
In most cases, TBE proceeds without complications and heals completely. This is especially true if the infection causes meningitis.
If the brain is also inflamed (meningoencephalitis), many sufferers continue to suffer from symptoms such as headaches, increased fatigue, reduced resilience and emotional lability for weeks. In addition, there may be memory, concentration and coordination disorders, language and speech disorders and paralysis. These complaints often heal completely, even if some of them take months or a few years. In one to two out of ten TBE patients, however, meningoencephalitis leaves permanent damage.
About three years after meningitis and encephalitis as a result of TBE, it is no longer to be expected that existing symptoms will improve significantly.
TBE, which affects the brain, meninges and spinal cord equally (meningoencephalomyelitis), has the worst prognosis: In a study, 57 patients were followed up for ten years after the disease. The early summer meningoencephalitis healed completely in only 20 percent. About 50 percent of the patients suffered permanent neurological deficits. Around 30 percent died as a result of the disease.
Overall, the risk of death from early summer meningoencephalitis is around one percent.
Lifelong Immunity?
Experts assume that people who have survived TBE are immune to the pathogen, so they cannot contract TBE a second time. However, it is not known whether this immune protection will last for life. Anyone who is still exposed to the risk of TBE infection should therefore have their immune protection refreshed with a TBE vaccination every three to five years.
TBE: prevention
An effective protection against TBE is the TBE vaccination mentioned above. But there is more you can do to prevent infection - by avoiding tick bites as much as possible. To do this, you should heed the following advice:
- Wear closed-toe shoes, long trousers and long sleeves when staying in forests, bushes and tall grass. If you put your trouser legs into your socks, a tick may have to crawl around the outside of your clothing - that's where it will catch your eye more easily. For the same reason, light-colored clothing makes sense.
- Apply a tick repellent to your skin before going into the forest and meadows. Please note, however, that it only has a temporary effect and does not offer 100 percent protection.
- Do not touch wild animals such as mice or hedgehogs. They often have ticks!
- After being outdoors, you should check clothing and all of your skin for ticks. The bloodsuckers prefer soft, warm parts of the body. That is why they are often found in the back of the knees or groin, under the armpits, in the navel, in the crook of the elbows, in the genital area, behind the ears, as well as on the head and hairline.
Remove ticks properly
If you spot a sucking tick on your skin, remove it as soon as possible. To do this, use tweezers or a special instrument to remove ticks. If you have neither one nor the other at hand, you should still remove the blood suction device as quickly as possible, for example with your fingernails.
Grasp the tick by the head area and as close as possible to the skin and pull it carefully and straight out. Avoid turning or crushing the animal! Otherwise it can release its saliva with the pathogens into the wound. For the same reason, you should never douse sucking ticks with oil or glue!
After removing the tick, you should carefully disinfect the small wound.
Watch out for possible signs of TBE (or Lyme disease) in the following days and weeks. If they show up, you should see a doctor immediately.
Additional information
Guidelines:
- Guideline "Early Summer Meningoencephalitis (TBE)" of the German Society for Neurology