Chronic fatigue syndrome
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Chronic Fatigue Syndrome (CFS) is a severe neuroimmunological disease that is primarily characterized by long-lasting, enormous exhaustion. This can be accompanied by many other complaints such as insomnia, sore throat or muscle pain, difficulty concentrating and an increased susceptibility to infections. The exact causes of CFS have not yet been conclusively clarified. Read here how chronic fatigue syndrome develops and how it is diagnosed and treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. G93
CFS: description
The term Chronic Fatigue Syndrome (CFS) is a serious and multifaceted neuroimmunological disease (neuroimmunological = affecting the nervous and immune system). The main symptoms are crippling mental and physical exhaustion and fatigue that cannot be explained by a known physical cause or specific mental disorder. In addition, those affected have a wide variety of other complaints.
Typically, CFS symptoms worsen after little physical or mental exertion. Rest or rest do not bring lasting improvement. The performance and quality of life of patients are often severely impaired for years. Many of those affected can no longer work and are bedridden. Some require extensive care. The level of suffering associated with this disease is often high because it is sometimes not recognized or is not taken seriously by the person concerned.
In the past, CFS was widely viewed as a mental illness. However, this is considered refuted - CFS is now regarded as a multi-system disease that affects, among other things, the immune system and energy metabolism.
Controversy over the correct name
There are different definitions and classification criteria for CFS. The naming of the clinical picture is (internationally) also not uniform and partly controversial:
For example, Chronic Fatigue Syndrome (CFS), especially in Great Britain and Scandinavia, is often referred to as myalgic encephalomyelitis (ME) - an extensive inflammation of the central nervous system (encephalitis myelitis = brain and spinal cord inflammation) with muscle involvement (myalgic) is considered to be the cause of the disease . Other experts prefer to use the combined term ME / CFS.
In Germany one often speaks of the chronic fatigue syndrome, sometimes also of the chronic fatigue syndrome. However, these terms are rejected by many experts and those affected as trivializing - the severe persistent weakness or fatigue of CFS patients has nothing to do with simple exhaustion or tiredness. In addition, those affected suffer from many other complaints, not only from pathological exhaustion.
In addition, CFS must not be confused with fatigue, which is often associated with cancer or other serious, chronic diseases and is known as fatigue syndrome. Although this causes similar complaints, it has a different cause. There are also similarities with the symptoms of other diseases such as fibromyalgia, which is a rheumatic disease.
frequency
How often a chronic fatigue syndrome occurs in Germany or other countries cannot be precisely determined - the information varies considerably, possibly because there are no standardized diagnostic criteria and the disease is often not recognized. According to the Federal Association of Chronic Fatigue Syndrome, an estimated 300,000 people in this country have chronic fatigue syndrome. This estimate is obtained if the corresponding American studies on the frequency of CFS are applied to Germany. Around 17 million people around the world are believed to have CFS.
Women are affected significantly more often than men. CFS can occur at any age. Very often those affected are between 29 and 35 years old when the disease breaks out (mean age of onset).
CFS: symptoms
Chronic fatigue syndrome (CFS) is a complex clinical picture that usually develops suddenly - often after a viral infection. But there are also those affected in whom CFS has gradually developed over a long period of time.
Experts use different catalogs of criteria for the diagnosis of "chronic fatigue syndrome". For example, the "Canadian Consensus Criteria" (CCC) and the International Consensus Criteria (ICC) are frequently used:
Canadian CFS Criteria
According to the Canadian Consensus Criteria (CCC), Chronic Fatigue Syndrome must have all of the following symptoms:
- Fatigue: new, inexplicable, persistent, or recurring physical or mental exhaustion that significantly reduces the patient's level of activity
- Post-exertional malaise and / or fatigue: After exertion, there is unusual exhaustion, increased feeling of illness, pain and / or worsening of other symptoms. It takes the patient more than 24 hours to recover.
- Sleep disorders: e.g. not restful sleep, disturbed day-night rhythm
- Pain: e.g. muscle and / or joint pain, novel headache
In addition, there must be at least two neurological or cognitive manifestations, for example confusion, impaired concentration and short-term memory, word-finding disorders, disorders of movement coordination (ataxias).
According to the Canadian criteria, another prerequisite for diagnosis is that at least one symptom occurs in at least two of the following categories:
- Autonomous manifestations: e.g. extreme paleness, dizziness, nausea and irritable bowel syndrome, bladder disorders, palpitations with or without cardiac arrhythmias
- Neuroendocrine manifestations: e.g. often low body temperature, sweating, intolerance to heat and cold, loss of or increased appetite, noticeable change in weight, worsening of symptoms with stress
- Immunological manifestations: e.g. sensitive lymph nodes, recurring sore throat, recurring flu-like symptoms, new hypersensitivity to food, drugs and / or chemicals
Last but not least, the symptoms must have existed for at least six months (in children for three months) so that the diagnosis "chronic fatigue syndrome" can be made.
International CFS criteria
According to the International Consensus Criteria (ICC), it is not a prerequisite for a diagnosis of "Chronic Fatigue Syndrome" that the symptoms have persisted for at least six months. The doctor can certify CFS earlier if the following criteria are met:
- Post-exertional neuroimmune exhaustion (PENE), i.e. after physical or mental exertion there is a disproportionate worsening of the symptoms (physical and mental exhaustion, muscle pain, cardiac arrhythmia, etc.), which can last for hours to days. Neither sleep nor rest help against it. PENE is considered a cardinal symptom that must be present in any case with a chronic fatigue syndrome.
- at least 1 symptom from the neurological impairment categorye.g. pain, sleep disorders, memory and concentration disorders, muscle weakness, disorders of movement coordination, sensitivity to smells, noises, light or touch
- at least 1 symptom from the immunological, gastrointestinal and urogenital impairment categorye.g. chronic respiratory infections, increased susceptibility to infections, food intolerance, irritable bowel syndrome, urination disorders
- at least 1 symptom from the category disruption of energy production and ion transporte.g. cardiac arrhythmias, palpitations, low blood pressure, dizziness, inability to adapt the circulation to an upright body position (orthostatic intolerance), sweating, shortness of breath, intolerance to heat / cold and strong temperature fluctuations
CFS: causes and risk factors
What exactly causes a chronic fatigue syndrome has not yet been conclusively clarified. According to recent studies, it appears to be an autoimmune disease (dysregulation of the immune system) and a serious disruption of the energy metabolism in the mitochondria ("power plants" of the cells). This is indicated by several studies in recent years. In addition, various factors are discussed that make CFS susceptible (predisposing), trigger or perpetuate it.
Preceding (predisposing) factors
A chronic fatigue syndrome is usually preceded by an infection. This infection often falls in a phase that is characterized by stress or high physical activity.
In addition, some experts suggest that some people have a genetic susceptibility (predisposition) to CFS. This is indicated by twin studies. So far, however, no specific risk genes for chronic fatigue syndrome have been identified.
Triggering factors
Most patients cite an infection as the cause of chronic fatigue syndrome. There are cases in which CFS occurred, for example, after an infection with Epstein-Barr virus (infectious mononucleosis) or enterovirus (e.g. flu infection), after dengue fever, Q fever or Lyme borreliosis.
In addition to such infections, severe injuries, operations, pregnancy or childbirth are sometimes the trigger for a chronic fatigue syndrome.Stressful events such as the death of a loved one or unemployment can also trigger CFS.
Sustaining Factors
Physical overload and psychological stress can exacerbate the symptoms of chronic fatigue syndrome. Also, if patients can no longer work, receive little social support, and / or become depressed because of CFS, it can make the disease worse. The same applies if those affected are not taken seriously by those around them (family, friends, colleagues, doctors, etc.).
Operations and accidents can also lead to an acute increase in symptoms. Another problem is the increased susceptibility to infections that often goes hand in hand with CFS: After an infection, many patients suffer more and more from the symptoms of chronic fatigue syndrome for weeks. Allergies and food intolerance can also have a negative impact on the condition of those with CFS.
CFS: examinations and diagnosis
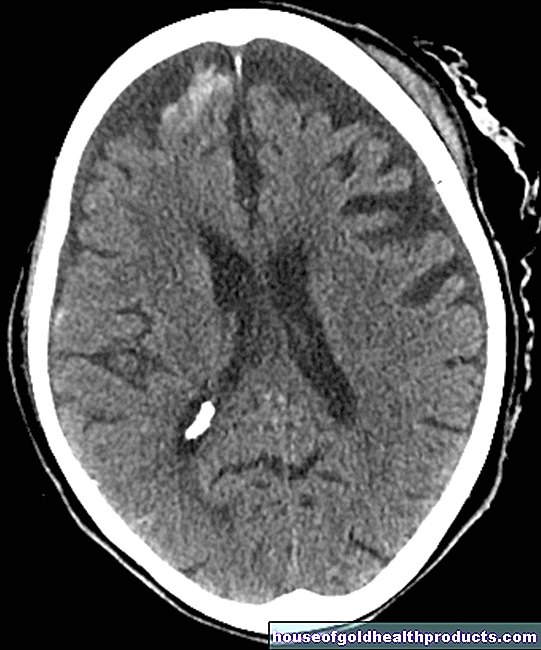
Chronic fatigue syndrome is difficult to diagnose and, in many cases, goes undetected. There are no special laboratory tests or tests with the help of apparatus to confirm the diagnosis of CFS. In addition to the exact recording of the medical history (anamnesis) with all occurring symptoms, the main aim is to rule out other diseases that can cause similar symptoms such as chronic fatigue syndrome. These include, for example:
- Thyroid, heart and liver diseases
- Anemia, for example due to iron deficiency
- Diabetes (diabetes mellitus)
- neurological diseases such as multiple sclerosis (MS)
- rheumatoid diseases (such as rheumatoid arthritis)
- Infectious diseases such as chronic hepatitis or borreliosis
- Tumor diseases
- severe mental illness (such as depression)
- Alcohol, drug, or medication abuse
- severe obesity (severe obesity)
Various tests, such as a physical exam, ultrasound, and blood tests may be necessary to rule out these factors. Once this is done, the doctor can use a catalog of criteria (see above under "Symptoms") to check whether the patient has the necessary characteristics of the chronic fatigue syndrome. If so, the diagnosis of CFS can be made.
CFS: treatment
Experts have not yet reached an agreement on how best to treat chronic fatigue syndrome. One thing is certain: CFS therapy should be individually adapted. It is based on the most stressful symptoms (e.g. sleep disorders, pain) and concomitant diseases and should include both medicinal and non-medicinal measures.
Medicines such as pain relievers can be used for joint pain and headaches, for example. If depression occurs along with the illness, treatment with antidepressants may also be necessary. If the patient has a (chronic) infection, this should be treated specifically, for example with antibiotics for a bacterial infection. If a deficiency in certain vitamins or minerals (such as vitamin D, zinc, iron) can be proven, it can make sense to compensate for the deficit with appropriate preparations.
Note: Targeted drugs for CFS are not yet available. Scientists are currently researching, for example, the effectiveness of drugs that regulate the immune system.
In general, a regular daily routine is recommended for CFS. Overexertion is strongly discouraged as it can worsen the symptoms. For the same reason, those affected should avoid emotional distress whenever possible.
Relaxation methods such as autogenic training or other methods of reducing stress often prove to be helpful. For example, they can help CFS patients with insomnia. In addition, a change in diet (sufficient vitamins and minerals, high protein, sufficient unsaturated fatty acids) and avoiding and eliminating harmful substances sometimes seem to reduce the symptoms of CFS in some cases.
CFS: disease course and prognosis
It is difficult to predict how a chronic fatigue syndrome (CFS) will progress in individual cases.
In most cases, the disease starts suddenly, often as a result of an infection: The persistent exhaustion and poor performance can be so pronounced that those affected hardly leave the house. Chronic fatigue syndrome can improve again after months or years - it is usually impossible to say whether it is spontaneous or due to a specific treatment. The regained efficiency is often not permanent: the chronic fatigue syndrome has a high relapse rate; Especially after infections, physical strain and periods of stress, the paralyzing and persistent exhaustion can return. Some of those affected by CFS are permanently restricted in their everyday life due to the disease (up to and including disability).
In rarer cases, chronic fatigue syndrome does not appear suddenly, but creeping in. Over time, the symptoms get worse. If a chronic fatigue syndrome takes this course, the chances of recovery are significantly worse.
Tags: toadstool poison plants alcohol drugs magazine






.jpg)