Penis fungus
and Martina Feichter, medical editor and biologistSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Penile fungus (Candida balanitis) is a fungal infection in men in the area of the glans. It is sometimes inaccurately called "vaginal thrush in men" because in both cases - vaginal and penile fungus - the same types of fungus cause the infection. Penile fungus is very uncomfortable, but with consistent therapy it usually heals completely within a few days. Read everything you need to know about the symptoms, causes, diagnosis, treatment and prognosis of penile fungus here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B37
Penile fungus: symptoms
Penile fungus causes symptoms similar to those of vaginal fungus: it initially manifests itself as reddening of the foreskin and glans. The inner parts of the foreskin are often swollen. Itching, burning, and even pain appear within a few days. Pain is particularly common during sexual intercourse or when urinating.
Furthermore, small blisters can form on the glans. Liquid collects in these. If the vesicles burst, the penis will get wet. Another sign of penile fungus are whitish to grayish deposits under the foreskin.
Note: If the fungal inflammation is limited to the glans, it is called candida balanitis. In uncircumcised men, the foreskin is usually also inflamed. Then it is a fungal balanoposthitis.
Penile fungus: causes
The triggers of penile fungus are yeast fungi. The yeast fungus Candida albicans is most often responsible for the infection - just as it does with the vaginal thrush in women. Other yeasts are less common (such as Candida glabrata).
Most of the time, yeasts are transmitted during sexual intercourse. Infection through contaminated objects is also possible, for example if affected men and healthy people share towels and bed linen.
Risk factors for penile fungus
The penis has a natural skin flora made up of various types of bacteria and other microorganisms. These create an environment in which other pathogenic germs cannot normally multiply well. With a healthy penile flora, penile fungus is very rare. It mainly develops when the skin flora of the penis is disturbed.
A weakened immune system is one of the most favorable factors for a fungal infection. This can for example be the result of diseases such as HIV or AIDS or diabetes (diabetes mellitus). In addition, a weak immune system can also be caused by certain drugs such as cortisone or cancer drugs from the group of cytostatic agents (chemotherapeutic agents).
Antibiotics can also favor penile fungus: These drugs generally have an inhibiting or killing effect on bacteria - including the beneficial bacteria in the skin flora in the intimate area. Antibiotic therapy can disrupt the balance of the natural skin flora and pave the way for penile fungus.
Excessive or inadequate genital hygiene is also considered a risk factor: Excessive hygiene disrupts the natural skin flora, so that pathogenic germs (such as yeasts) can spread more easily. Inadequate genital hygiene is just as unfavorable: the sebum glands under the penis foreskin form a yellowish-whitish secretion called smegma. If it is not removed regularly, it becomes a breeding ground for pathogens such as yeast - this can quickly lead to infections such as penile fungus.
In this context, boys or men with a narrowing of the foreskin (phimosis) are particularly susceptible to penile fungus: the narrowed foreskin often means that the smegma cannot be removed as thoroughly as it would be necessary.
Another risk factor for the development of penile fungus is frequent sexual intercourse. Those who frequently have unprotected sexual intercourse are at an increased risk of contracting sexually transmitted diseases such as penile fungus. It is particularly risky if you change sexual partners frequently.
Old age and being very overweight are also risk factors for penile fungus: Fungi (and other germs) can easily multiply in the skin folds of older or overweight men.
Penile fungus: diagnosis
If you suspect penile fungus, a urologist is the right contact. In a first conversation, he collects the medical history (anamnesis). You have the opportunity to describe your complaints in detail. The doctor then asks further questions such as:
- Do you often have unprotected sex?
- Do you frequently change partners during sexual intercourse?
- Have you been abroad recently?
- Have you ever had such complaints in the past?
A physical examination follows after taking the medical history. The doctor carefully examines the changes to the penis. The classic changes (reddening, whitish-grayish coatings) in connection with the symptoms described (such as severe itching) usually clearly indicate penile fungus.
To confirm the diagnosis, the doctor takes a smear (usually from the area under the foreskin). This smear is first examined under the microscope: under the high magnification, long, thread-like structures (fungal threads or hyphae) can be seen in the case of a fungal infection.
In some cases, looking into the microscope does not reveal exactly what type of pathogen it is. Then the smear is sent to a laboratory and a culture is created. That means: The pathogens in the smear are exposed to optimal growth conditions so that they can multiply. Then they can be determined more easily. It usually takes about a week to get the result. Non-specific therapy can, however, be started before the final diagnosis.
Penile fungus: treatment
Special agents, so-called antimycotics, are used to treat fungi. Antifungal drugs inhibit the growth of fungi or kill them directly. In the case of penile fungus, antimycotics are usually applied externally, for example in the form of ointments or creams. You will need to apply these to the affected areas regularly for a few days - your doctor will give you more detailed instructions on how to do this.
The penis should be kept as dry as possible during treatment. If the penis fungus gets wet, you can wrap the glans and foreskin with strips of gauze after applying the antifungal agent, which absorb the moisture.
You should avoid sexual intercourse during the entire treatment, as there is a high risk of infection for your partner. In addition, it makes sense that this person can also be examined for a fungal infection and, if necessary, treated. This prevents the two of you from infecting each other again and again.
Also, ensure adequate hygiene during treatment. Change towels and underwear every day and wash them at at least 60 degrees Celsius.
You should avoid the swimming pool and sauna until the fungal infection has completely healed.
Penile fungus: Surgical intervention for constriction of the foreskin
In men with narrowing of the foreskin who repeatedly have penile fungus, surgery may be useful. As with circumcision, the foreskin is removed. In this way, the glans can be cleaned better and kept dry in the future. The doctor and patient decide jointly about such an operation.
Penile fungus: prognosis
As a rule, the prognosis for penile fungus is favorable. The infection usually heals within a few days. To do this, however, it is important to consult a doctor immediately after the first symptoms appear. He can initiate the right therapy. In addition, the course of the disease and prognosis also depend on whether risk factors for the fungal infection can be eliminated or at least reduced. If there is a disease-related weakness of the immune system (e.g. HIV or diabetes), the underlying disease should be treated properly. If the foreskin is narrowed, surgery may be considered. If such risk factors for penile fungus are not eliminated or reduced, there is a risk that the fungal infection will recur even after successful treatment.
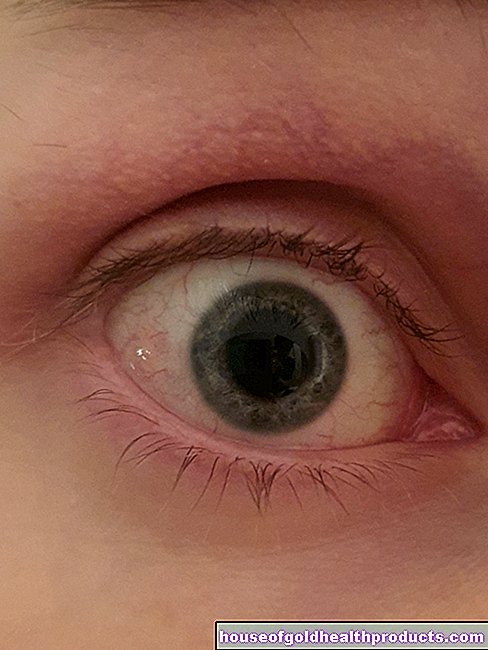
Tags: Diagnosis eyes baby toddler