Inflammation of the stomach lining
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Abdominal complaints such as a feeling of fullness or pain in the upper abdomen are typical of gastric mucosal inflammation. The patients have no appetite and often feel sick. Gastritis can be acute or chronic. Often, even sparing the stomach improves the symptoms; in more severe or chronic cases, medication can help. Read here how to recognize inflammation of the gastric mucosa and what you can do.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K29K52

Brief overview
- Symptoms: bloating, pain in the upper abdomen, loss of appetite, nausea, heartburn, belching, less often digestive problems
- Causes: irritating substances (e.g. alcohol, medication), stress, stomach germ Helicobacter pylori, autoimmune reactions
- Treatment: light food, acid binders, proton pump inhibitors, relaxation exercises
- Diet: light food, avoiding alcohol and hot spices, steaming instead of frying
- Dangers: Danger to life with bleeding ulcers, long-term increased risk of stomach cancer
Inflammation of the gastric mucosa: symptoms
Gastritis can cause various unspecific complaints. The main symptoms are typical of both acute and chronic gastritis. However, they occur suddenly in the acute form, while chronic gastric mucosal inflammation develops slowly.
Common symptoms of gastritis are:
- Bloating
- Pain in the upper abdomen
- decreased appetite
- nausea
- Vomit
- heartburn
- Eructation
- Bad breath
Less common are:
- Flatulence
- bland taste in the mouth
- early onset of satiety
- Back pain
- diarrhea
-
"Medicines can make you vulnerable"
Three questions for
Dr. med. Peter Strauven,
Specialist in general and nutritional medicine -
1
Who is particularly prone to stomach inflammation?
Dr. med. Peter Strauven
These are, for example, people who drink a lot of alcohol. But there are also drugs that make you susceptible. These include blood thinners, acetylsalicylic acid, or pain relievers like ibuprofen and diclofenac. As a side effect, they attack the lining of the stomach. Last but not least, the Helicobacter pylori bacterium can also trigger inflammation of the gastric mucosa.
-
2
How long do I have to go easy on my stomach if I have gastritis?
Dr. med. Peter Strauven
In the case of significant gastritis, an acid blocker is taken for at least three weeks. The gastric mucosa can regenerate in this way. Base preparations also help in mild cases. Either way, the following applies: You support recovery by refraining from smoking and alcohol as well as avoiding stress. If you are then symptom-free, you should take care to keep your stress levels within limits.
-
3
Can I prevent inflammation of the stomach lining?
Dr. med. Peter Strauven
Under no circumstances take acid blockers preventively! This inhibits, among other things. digestive performance: the stomach needs acid for digestion. Basically, you keep your stomach fit with a harmonious life. That means: a regular daily routine, exercise, alcohol in moderation, if possible, no smoking and enough sleep. And: “Well chewed, half digested” - eat three times a day in peace, without hurrying and not while standing.
-
Dr. med. Peter Strauven,
Specialist in general and nutritional medicineDr. med. Peter Strauven - specialist in general and nutritional medicine and MSc in preventive medicine - runs a holistic private practice in Bonn with a focus on gastrointestinal diseases.
↓
Symptoms of Chronic Gastritis
In the case of chronic gastritis, depending on the causes, a distinction is made between types A, B and C as well as various special forms.
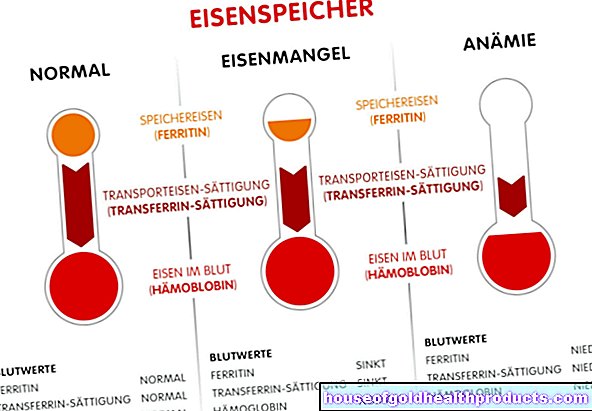
Symptoms of type A gastritis
With type A gastritis, less stomach acid is produced. This can cause indigestion. In addition, this form of gastritis results in a vitamin B12 deficiency, which triggers what is known as pernicious anemia, a special form of anemia. Symptoms are, among other things, paresthesia, tiredness and exhaustion.
Symptoms of type B gastritis
Type B gastritis usually only shows unspecific symptoms. Some patients develop bad breath and, as the process progresses, additional diseases such as:
- Duodenal ulcer (duodenal ulcer)
- Stomach cancer (gastric cancer)
- MALT lymphoma (mucous membrane-associated cancer of the lymphoid tissue)
Symptoms of type C gastritis
Chronic gastric mucosal inflammation of type C usually only causes unspecific symptoms. Many patients report discomfort in the upper abdomen. The symptoms often correspond to those of an irritable stomach.
Inflammation of the gastric mucosa: causes and risk factors
Gastritis occurs when the protective lining of the stomach is damaged. These can be stomach-irritating substances or factors that stimulate an overproduction of corrosive gastric acid.
Acute gastritis triggers are, for example:
- excessive consumption of alcohol
- excessive consumption of nicotine
- Frequent consumption of foods that irritate the stomach, such as coffee or hot spices
- Frequent or high dose use of certain medications, for example pain relievers or anti-inflammatories such as cortisone
- mental stress
- Food poisoning from bacteria such as staphylococci or salmonella
- mechanical irritation, e.g. from a nasogastric tube or other foreign body
- Chemical burns from acids or alkalis
- Physical stress such as long-term ventilation, head trauma, burns, brain diseases, major operations, shock (circulatory collapse)
- Competitive sport ("runners stomach")
If bacteria such as staphylococci or salmonella are the cause, inflammation of the stomach lining can be contagious. The pathogens are then excreted in the stool, and other people can become infected, for example by sharing the toilet.
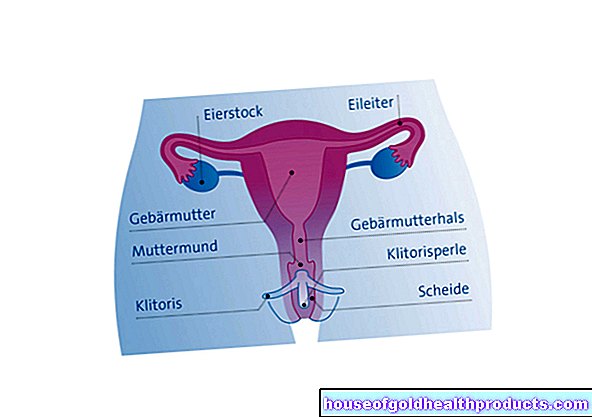
This is how the stomach is built
Causes of Chronic Gastritis
Type A gastritis
Type A gastritis is also known as autoimmune chronic gastric mucosal inflammation. Autoimmune means that the body's own defense system turns against the body itself: It forms antibodies that attack the body's own structures. Type A gastritis is the rarest form of chronic gastric mucosal inflammation, accounting for around 5 percent of cases.
They attack the parietal cells that produce stomach acid. Therefore, less stomach acid is released. Other antibodies are directed against the intrinsic factor. This protein is produced in the stomach and is necessary for the absorption of vitamin B12. The result is a vittamin B-12 deficiency.
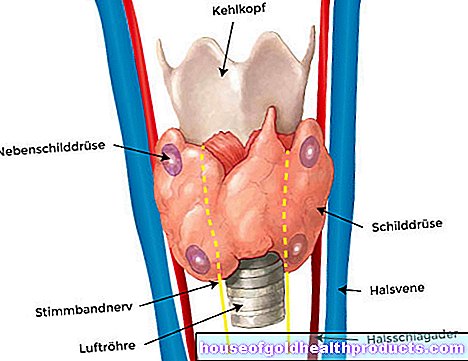
Type A gastritis makes up about five percent of chronic gastric mucosal inflammation. It can be inherited and mainly affects northern Europeans. The inflammation is often localized in the main part of the stomach. Many patients also suffer from other autoimmune diseases, for example
- Addison's disease
- Type I diabetes mellitus
- Hashimoto's thyroiditis (autoimmune inflammation of the thyroid gland)
Type B gastritis
About 80 percent of chronic gastritis cases are of type B. They are mostly caused by the bacterium Helicobacter pylori (H. pylori). The stomach germ can be transmitted through saliva or stool. Related pathogens are also less frequently the cause of type B gastritis such as Helicobacter heilmannii, which is transmitted from dogs or cats to humans.
Inflammation of the stomach lining caused by bacteria
Chronic gastritis of type B mainly affects the stomach section between the stomach body and the stomach outlet (stomach antrum).
Type C gastritis
Chronic gastric mucosal inflammation of type C accounts for about 15 percent of chronic gastric mucosal inflammation. It is caused by chemical irritation of the stomach. These include above all pain relievers such as acetylsalicylic acid (ASA), ibuprofen or diclofenac. They belong to the group of non-steroidal anti-inflammatory drugs (NSAIDs).
The backwashing of bile into the stomach (bile reflux) can also result in chronic type C gastritis.
Rare forms of chronic gastritis
In rare cases, chronic gastritis can also have other causes. Among other things, there are the following special forms:
- Eosinophilic (allergic) gastritis: for example, if you are allergic to cow's milk or soy
- Lymphocytic gastritis: possibly caused by H. pylori or celiac disease, leads, among other things, to Ménétrier's disease (giant fold gastritis) or anemia (anemia)
- Granulomatous gastritis: in inflammatory diseases such as Crohn's disease, sarcoid or tuberculosis
Inflammation of the gastric mucosa: therapy
Inflamed or irritated gastric mucosa can often be treated on your own with simple measures. If that is not enough, various medications can help.
The first measure to be taken in the case of gastritis is to omit anything that irritates the gastric mucosa. Coffee, alcohol and nicotine are therefore taboo during gastritis.
If the symptoms are severe, it can make sense to completely avoid food for one or two days. Usually you don't have an appetite anyway.
Otherwise it is often enough to eat light foods with easily digestible small meals.
If stress is the trigger for gastritis, relaxation methods such as autogenic training, meditation or Jacobson's progressive muscle relaxation can help.
Useful gastritis home remedies are also:
- Hot water bottle or grain pillow (cherry stone pillow)
- Chamomile tea (has an anti-inflammatory effect)
- Tea mixture of chamomile, peppermint and licorice (mix half a teaspoon each of licorice root and chamomile flowers with a teaspoon of peppermint leaves)
- Gruel (protects the stomach lining)
- Lemon balm or hop blossom tea (have a calming effect)
- Potato juice
- Healing earth
Rolling cure with chamomile tea: A rolling cure for stomach inflammation can also be helpful. To do this, drink two cups of chamomile tea. Then lie on your back for ten minutes. Then turn on your left side, right side, and stomach for another ten minutes each. Lie there for about half an hour after this roller cure. Use this home remedy every day for a week.
Treatment with medication
Antacids: If behavioral measures alone are not enough, antacids help. These active ingredients neutralize the aggressive stomach acid.
H2-receptor blockers: Another possibility are so-called H2-receptor blockers (such as cimetidine or ranitidine). They decrease the production of stomach acid. This allows the inflamed gastric mucosa to recover and is protected from further damage.
Proton pump inhibitors: So-called proton pump inhibitors (proton pump inhibitors, PPIs) are even more effective. They also reduce stomach acid production. Often used PPIs are for example omeprazole and pantoprazole. However, they should only be taken long-term in exceptional cases and in consultation with the doctor.
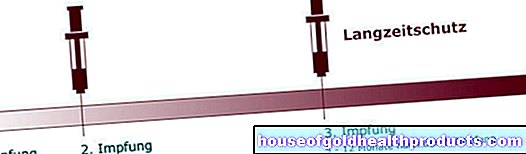
Antibiotics: If you have chronic type B gastritis, you have to get rid of the pathogenic bacteria. A combination of two or three antibiotics together with a proton pump inhibitor for seven days, for example, can drive out Helicobacter pylori in over 90 percent of cases.
Antispasmodic and anti-nausea agents: Anti-nausea agents (antiemetics) or antispasmodic, pain-relieving drugs (antispasmodics) help against other gastritis complaints.
Vitamin B 12: Chronic type A gastritis carries the risk of pernicious anemia. This is caused by a vitamin B12 deficiency. The patients therefore mostly receive vitamin B12 injections.
Treatment with alternative medicine
Homeopathy: Homeopathic remedies for inflammation of the gastric mucosa are, for example, Carbo vegetabilis and Lycopodium. They are supposed to alleviate the discomfort.
Schüßler salts: Schüßler salts against nausea or belching are, for example, No. 9 sodium phosphoricum, which is supposed to regulate the acid balance in the body, and No. 7 magnesium phosphoricum, which is said to have a relaxing, antispasmodic effect on the digestive organs.
Traditional Chinese Medicine: Treatment according to Traditional Chinese Medicine (TCM) - for example in the form of acupuncture - can also alleviate gastritis symptoms, as patients report
Emergency gastric bleeding!
Sometimes the damage to the mucous membrane in gastritis is so pronounced that bleeding occurs. In milder cases, this can be stopped with a gastroscopy. Heavy bleeding - recognizable by bloody vomiting or dark-colored stools (tarry stools) - can be life-threatening. They require emergency treatment. Sometimes only surgery can stop the bleeding.
nourishment
The main aim of gastritis is not to further irritate the stomach lining. Many patients with acute gastric mucosal inflammation do not have an appetite anyway, so they do not eat at all for a day or two. It is then important to take in sufficient fluids, for example chamomile tea or clear broth.
The following tips on how to protect your stomach can also help:
- Avoid stomach-irritating substances such as citrus fruits, coffee, alcohol, hot spices
- Oatmeal, rusks, soups, rice and mashed potatoes are particularly gentle on the stomach
- It is better to have five small meals spread over the day than a few large ones
- Raw food puts a strain on sensitive stomachs. Steamed dishes are the most digestible.
- High-fat foods are unfavorable
For more information on nutrition for gastritis, read the article Inflammation of the gastric mucosa: Nutrition.
Examinations and diagnosis
If you have stomach problems, consult your family doctor first. If necessary, he will refer you to a stomach specialist, a gastroenterologist, as the process progresses. First, your doctor will ask you in detail about your medical history (anamnesis). For example, he asks:
- Since when are you having those complaints?
- Do you suffer from stomach pain, vomiting or diarrhea?
- Are you taking any medication such as pain relievers?
- Do you feel full?
Physical examination
Your doctor will then examine you.To do this, it listens to your stomach, registering both the intestinal noises and the pulse rate of the large blood vessels in the abdomen. Then he pats your stomach. In this way he can detect accumulations of air or fluid. When palpating the abdomen, the doctor pays attention to possible hardening. It also palpates your liver under the right costal arch and your spleen under the left costal arch.
Endoscopy
Gastritis can only be clearly diagnosed if the doctor takes a look inside the stomach. In a so-called endoscopy, a thin tube with a small camera at the tip is carefully pushed through the esophagus and into the stomach. In this way, the doctor can identify possible changes in the mucous membrane such as reddening, swelling or bleeding.
biopsy
With the help of fine instruments, the doctor can also take a tissue sample from the mucous membrane as part of the endoscopic examination. A pathologist examines these tissue samples under his microscope to determine the type of inflammation. He can see whether the inflammation is limited to the upper layers of the mucous membrane (surface gastritis) or whether the gastric glands have already been damaged (atrophic gastritis).
Test for Helicobacter pylori
He can also use the biopsy to perform a rapid urease test for the stomach germ Helicobacter pylori. It is the most common trigger for chronic gastric mucosal inflammation. For this purpose, urea is added to the tissue sample. If the bacterium is present, its enzyme (urease) will convert the urea into ammonia. This response can be measured.
Other tests to identify H. pylori as a cause of chronic gastritis include:
- Breath test: The patient is given radioactively labeled urea. H. pylori breaks it down, which means that radioactively labeled carbon dioxide can be detected in the exhaled air.
- Antigens in the stool: H. pylori proteins are excreted through the intestine. These can be detected in the stool.
- Antibodies in the serum: When infected with H. pylori, the immune system produces antibodies against the bacteria. These can also be detected in the patient's blood after infection.
Detection of auto antibodies
If type A gastritis is suspected, tests are carried out for appropriate auto-antibodies. If chronic bleeding occurs, the blood count may show microcytic anemia - a form of anemia with reduced red blood cells.
Course of the disease and prognosis
Acute gastric mucosal inflammation usually has a good prognosis. It often heals on its own after a few days or weeks without further treatment. But there are also severe courses, for example when patients have "erosive gastritis". If bleeding occurs in what is known as hemorrhagic gastritis, it can be life-threatening. In addition, inflammation of the lining of the stomach can develop into a stomach ulcer.
Chronic gastric mucosal inflammation usually lasts for several weeks, months or even years. With chronic gastritis, the constant irritation of the gastric mucosa increases the risk that cells will degenerate and cause stomach cancer. First, the cells of the gastric mucosa transform into intestinal-like cells. Then one speaks of intestinal (belonging to the intestine) metaplasia (transformation).
Anyone who has chronic gastritis should therefore have a gastroscopy performed regularly every three years. In this way, cancer and precancerous stages can be identified and treated in good time.
Additional information
Books
- Irmgard Fortis Nutrition in Gastritis, Maudrich, 2017
- Astrid Laimighofer: Light food for the stomach and intestines: How to gently build your diet according to the 3-step concept on Trias 2014
- Heide Steigenberger irritable stomach: Correct handling of gastritis, heartburn, stomach pressure and digestive disorders Kneipp Verlag, 2014
- Gastritis, gastric and duodenal ulcers - Issue 55, Robert Koch Institute, 2013
Guidelines
- Helicobacter pylori and gastroduodenal ulcer disease, German Society for Gastroenterology, Digestive and Metabolic Diseases, December 2016










.jpg)