Type 1 diabetes
and Martina Feichter, medical editor and biologist Updated onDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Type 1 diabetes is the rarer form of diabetes. The pancreas no longer produces enough or no insulin at all. Those affected therefore have to inject the hormone insulin regularly throughout their life in order to lower their high blood sugar level. Read more about the causes, symptoms, diagnosis, treatment and prognosis of type 1 diabetes here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E10
Type 1 Diabetes: Brief Overview
- Cause: autoimmune disease (antibodies destroy the insulin-producing beta cells in the pancreas); Genetic changes and other factors (such as infections) are likely to be involved in the development of the disease
- Age of onset: mostly childhood or adolescence
- Frequent symptoms: intense thirst, increased urination, weight loss, dizziness, nausea, weakness, in extreme cases impaired consciousness up to unconsciousness
- Investigations: Measurement of blood sugar and HbA1c, oral glucose tolerance test (oGTT), search test for autoantibodies
- Treatment: insulin therapy
Type 1 diabetes: causes and risk factors
Type 1 diabetes is also called juvenile (adolescent) diabetes because it usually appears in children and adolescents, sometimes also in early adulthood. In those affected, the body's own antibodies destroy the insulin-producing beta cells in the pancreas. Type 1 diabetes is a so-called autoimmune disease.
As soon as these autoantibodies have destroyed around 80 percent of the beta cells, type 1 diabetes becomes noticeable in the form of greatly increased blood sugar levels: The destruction of the beta cells results in a lack of insulin. This hormone normally ensures that sugar (glucose) circulating in the blood reaches the body's cells, where it serves as a source of energy. Because of the lack of insulin, the sugar accumulates in the blood.
Why the immune system attacks the beta cells of the pancreas in people with type 1 diabetes mellitus is not yet fully understood. Scientists suspect that genes and other influencing factors play a role in the development of type 1 diabetes.
Type 1 diabetes: genetic causes
According to current medical guidelines, around 10 percent of type 1 diabetes patients have a first-degree relative (father, sister, etc.) who is also suffering from diabetes. That speaks for a genetic predisposition. Researchers have already identified several genetic changes that have been linked to the development of type 1 diabetes. As a rule, there are several genetic changes that together lead to type 1 diabetes mellitus.
A group of genes that are almost exclusively on chromosome 6 seems to have a particularly great influence: the so-called human leukocyte antigen system (HLA system) has a significant influence on the control of the immune system. Certain HLA constellations such as HLA-DR3 and HLA-DR4 are associated with an increased risk of diabetes 1.
In general, however, type 1 diabetes is apparently less inheritable than type 2. In identical twins, both identical twins almost always develop type 2 diabetes. In type 1 diabetes, this is only observed in about every third identical twin pair.
Type 1 diabetes: other influencing factors
The development of type 1 diabetes could also be influenced by various external factors. In this context, researchers are discussing:
- too short a period of breastfeeding after giving birth
- giving cow's milk to children too early
- too early use of gluten-containing foods
- Toxins like nitrosamines
Infectious diseases could possibly also contribute to or at least promote the malfunction of the immune system in type 1 diabetes. Suspected include mumps, measles, rubella and infections with Coxsackie viruses.
It is also noticeable that type 1 diabetes mellitus often occurs together with other autoimmune diseases. These include, for example, Hashimoto's thyroiditis, gluten intolerance (celiac disease), Addison's disease and autoimmune gastric mucosal inflammation (type A gastritis).
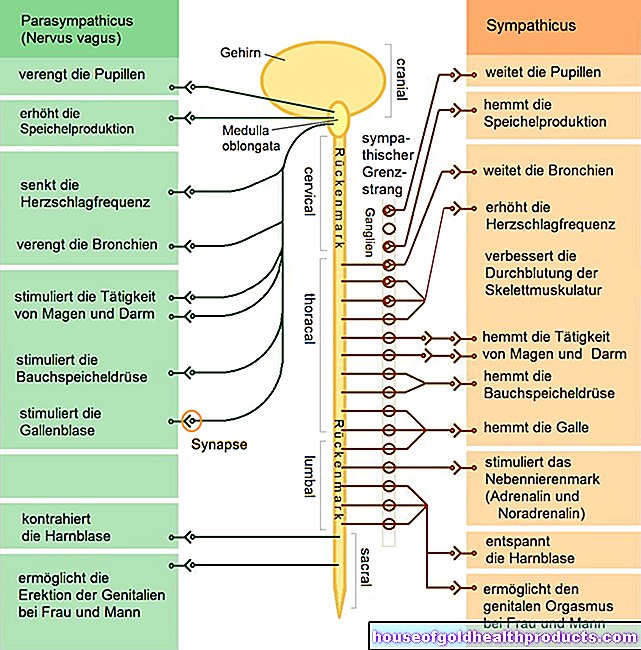
Finally, there is also evidence that damaged nerve cells in the pancreas could be involved in the onset of type 1 diabetes.
Between type 1 and type 2: LADA diabetes
LADA (latent autoimmune diabetes in adults) is a rare form of diabetes that is also considered late-onset type 1 diabetes. However, there is also overlap with type 2 diabetes:
As with "classic" type 1 diabetes, diabetes-specific autoantibodies can also be detected in the blood with LADA - but only one type (mostly glutamate decarboxylase antibody = GADA), while type 1 diabetics usually have at least two different types of diabetes - Have antibodies.
Another thing they have in common with type 1 diabetes is that LADA patients are usually rather slim.
While type 1 diabetes almost always appears in childhood and adolescence, LADA patients are usually older than 35 years when diagnosed. This is similar to type 2 diabetes (the age of onset is usually after the age of 40).
In addition, LADA patients such as type 2 diabetics often show evidence of a metabolic syndrome. This is characterized by disorders of the lipid metabolism and high blood pressure, for example.
The slow disease development of LADA is also more comparable to type 2 diabetes. For many LADA patients, a change in diet and treatment with blood sugar-lowering tablets (oral anti-diabetic drugs) are initially sufficient to lower the elevated blood sugar levels. This is also the treatment for many type 2 diabetics. LADA patients only need insulin injections as the disease progresses - in type 1 diabetes, these are essential from the start.
Because of the various overlaps, LADA patients are often diagnosed as type 1 or type 2 diabetics. Sometimes LADA is simply viewed as a hybrid of both main types of diabetes. In the meantime, however, it is more likely that in LADA both clinical pictures are present and develop in parallel.
Idiopathic type 1 diabetes
Idiopathic type 1 diabetes is very rare. The patients have a permanent insulin deficiency, but have no detectable autoantibodies. They tend to have their body or blood repeatedly over-acidic (ketoacidosis). This form of diabetes is highly inheritable and occurs predominantly in people of Asian or African origin.
Type 1 diabetes: symptoms
People with type 1 diabetes are usually slim (as opposed to type 2 diabetics). They typically show severe thirst (polydipsia) and increased urine output (polyuria). The trigger for both of these symptoms is the greatly increased blood sugar level.
Many sufferers also suffer from weight loss, fatigue and lack of drive. In addition, dizziness and nausea may occur.
When the blood sugar level is very high, type 1 diabetes patients develop impaired consciousness. Sometimes they even fall into a coma.
You can read more about the signs and symptoms of type 1 diabetes in the article Diabetes mellitus symptoms.
Type 1 diabetes: examinations and diagnosis
If you suspect type 1 diabetes mellitus, the right person to contact is your general practitioner (pediatrician if necessary) or a specialist in internal medicine and endocrinology / diabetology. He will first have a detailed conversation with you or your child to collect the medical history (anamnesis). He has the complaints such as frequent thirst or increased urination described in detail. He also asks about any previous or accompanying illnesses and about diabetics in the family.
Tests for type 1 diabetes
The interview is followed by a physical examination. The doctor will also ask for a urine sample and make an appointment with you for a blood sample. This has to be done soberly. That means: In the eight hours before the (morning) blood draw, the patient is not allowed to eat anything and, at most, consume unsweetened, calorie-free drinks (such as water). The doctor can use the blood and urine samples to diagnose diabetes. Sometimes an oral glucose tolerance test (oGTT) is also useful.
You can read more about these examinations in the article Diabetes Test.
Detection of autoantibodies
In order to differentiate between type 1 and type 2 diabetes, for example, the doctor also has typical autoantibodies determined in the blood. Those that are directed against different structures of the beta cells are:
- Islet Cell Antibodies (ICA)
- Antibodies against beta cell glutamate decarboxylase (GADA)
- Antibodies against tyrosine phosphatase
- Antibodies against the zinc transporter of the beta cells.
Children with type 1 diabetes in particular often also have antibodies against insulin.
Autoantibodies in the blood don't have to be diabetic. If the doctor finds antibodies, however, this can be an indication that pathological hypoglycaemia will soon develop.
Type 1 diabetes stages
The Juvenile Diabetes Research Foundation (JDRF) and the American Diabetes Association (ADA) already speak of type 1 diabetes when the patient has no symptoms, but antibodies in the blood. They differentiate between three stages of the disease:
- Stage 1: The patient has at least two different autoantibodies
- Stage 2: The blood sugar levels (on an empty stomach or after eating) are increased ("prediabetes")
- Stage 3: Hypoglycemia is present
Type 1 diabetes: treatment
Type 1 diabetes is based on an absolute insulin deficiency, which is why patients have to inject insulin for life. Human insulin and insulin analogues are generally recommended. They are given with a syringe or (usually) with what is known as an insulin pen. The latter is an injection device that resembles a filler. Some patients also use an insulin pump, which provides insulin to the body continuously.
For type 1 diabetes patients, a thorough understanding of the disease and insulin use is very important. Therefore, every patient should attend a special diabetes training course immediately after the diagnosis.
Diabetes education
In a diabetes training course, patients learn more about the causes, symptoms, consequences and treatment of type 1 diabetes. They learn how to correctly measure blood sugar and how to inject themselves with insulin. Patients are also given tips for living with type 1 diabetes, for example with regard to exercise and nutrition. Since the blood sugar drops through exercise, the patients have to monitor their blood sugar values closely and practice the correct adjustment of the insulin and sugar intake.
With regard to nutrition, patients learn, for example, how much insulin the body needs and when for which food. The decisive factor here is the proportion of usable carbohydrates in a food. It affects the amount of insulin that has to be injected.
The so-called carbohydrate unit (KHE or KE) plays an important role in this. It is equivalent to ten grams of carbohydrates and increases blood sugar levels by around 30 to 40 milligrams per deciliter (mg / dL). Instead of the carbohydrate unit, the bread unit (BE) was mainly used in the past. One BE corresponds to 12 grams of carbohydrates.
You can find out everything you need to know in the articles "Diabetes - Nutrition" and "Bread Units".
By the way: Attending a diabetes training course is also recommended for carers in facilities that are attended by type 1 diabetics. These are, for example, teachers or educators at a day care center.
Conventional insulin therapy
With conventional (conventional) insulin therapy, the patients inject insulin according to a set schedule: The insulin is injected two or three times a day at set times and in set doses.
One advantage of this fixed scheme is that it is easy to use and particularly suitable for patients with limited learning or memory. Another advantage is that there is no need to have constant blood sugar measurements.
On the other hand, this fixed scheme leaves the patient relatively little room for maneuver, for example if they want to change their meal plan spontaneously. So a relatively rigid lifestyle is required. In addition, blood sugar cannot be adjusted as evenly with conventional insulin therapy as it is possible with intensified insulin therapy (see below). Consequential damage to diabetes mellitus is therefore more likely with this scheme than with intensified insulin therapy.
Intensified insulin therapy (basic bolus principle)
As part of an intensified insulin therapy, a long-acting insulin is usually injected once or twice a day. It covers the fasting need for insulin and is also called basic insulin (basal insulin). Immediately before a meal, the patient measures his or her current blood sugar level and then injects normal insulin or short-acting insulin (bolus insulin). Its dose depends on the previously measured blood sugar level, the carbohydrate content of the planned meal and planned activities.
The basic bolus principle requires good cooperation from the patient (adherence). The blood sugar has to be measured several times a day in order to avoid hypoglycemia or hypoglycemia. You need a little spade in your finger for that. The blood drop that emerges is examined for its sugar content using a measuring device.
A great advantage of the intensified insulin therapy is that the patient is free to choose the food and the range of motion. This is because the dose of bolus insulin is adjusted accordingly. If the blood sugar levels are permanently well adjusted, the risk of secondary diseases decreases significantly.
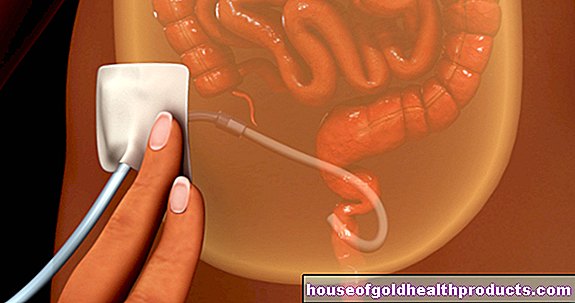
By the way: A more recent development is a small glucose sensor that is attached to the skin and reaches into the subcutaneous fatty tissue (e.g. on the stomach). It measures tissue sugar every one to five minutes (continuous glucose monitoring, CGM). The measurement results are transmitted by radio to a small monitor, where the patient can read them. This can be supported by the intensified insulin therapy (sensor-supported insulin therapy, SuT). Various alarm options warn the patient if there is a threat of hypoglycaemia or hypoglycaemia. The manual blood sugar measurements are still necessary because there is a physiological difference between tissue and blood sugar.
Insulin pump
A diabetes pump is often used, especially in young diabetics (type 1). This is a programmable, battery-operated, small insulin dosing device that the patient always carries with him in a small bag, for example on his belt. The insulin pump is connected via a thin tube (catheter) to a fine needle that is inserted into the subcutaneous fat tissue on the abdomen.
The pump is programmed to deliver small amounts of insulin to the body throughout the day. They cover the daily basic requirement (fasting requirement) of insulin. A freely selectable amount of bolus insulin can also be injected with meals at the push of a button. The patient must calculate this beforehand. He takes into account the current blood sugar level (he has to measure it), the planned meal and the time of day.
The pump should be set up and adjusted in a specialized diabetes practice or clinic. The patient must be trained intensively before use. The insulin cartridges in the pump are regularly replaced or refilled.
The insulin pump gives children in particular a lot of freedom. If necessary, you can also disconnect the diabetes pump for a short time (for example for showering). However, the pump should definitely be worn when exercising.Many patients report that their quality of life has improved significantly thanks to the insulin pump.
However, the pump must be worn all the time, even at night. If the catheter becomes clogged or kinked or the device fails unnoticed, the insulin supply is interrupted. This can quickly lead to dangerous hypoglycaemia and, as a result, hyperacidity (diabetic ketoacidosis). In addition, insulin pump therapy is more expensive than intensive insulin therapy.
By the way: The continuous glucose monitoring (CGM) mentioned above can also be combined with an insulin pump. The glucose sensor used in the subcutaneous fatty tissue transmits the measured values of the tissue sugar directly to the pump and warns of possible hypoglycaemia or hypoglycaemia. Doctors speak of sensor-assisted insulin pump therapy (SuP). Regular blood sugar measurements are still necessary here as well.
Insulins
There are different types of insulins available to treat diabetes mellitus. Often it is human insulin, which is artificially produced and has the same structure as the body's own insulin. Insulin analogues are also available for the treatment of diabetes. They are similar to human insulin, but differ slightly in structure.
Few diabetics use animal insulin from pigs or cattle - mostly due to an intolerance to the preparations described above. However, this is no longer manufactured in Germany and has to be imported.
Insulins can be classified according to their onset of action and their duration of action. There are, for example, short-acting and long-acting. You can read the most important information about the different insulin preparations in the Insulin article.
Type 1 diabetes: disease course and prognosis
Type 1 diabetes is an autoimmune disease that lasts a lifetime. However, some scientists believe that type 1 diabetes may be curable at some point in the future. For years they have been researching various therapeutic approaches - but so far without a breakthrough.
Life expectancy
Type 1 diabetes life expectancy has increased enormously over the past few decades due to advances in treatment (intensified insulin therapy). Nevertheless, type 1 diabetics have a reduced life expectancy compared to the healthy population. For example, a study from Scotland found that 20-year-old patients with type 1 diabetes have a life expectancy that is around 11 years (men) and 13 years (women) lower than non-diabetics.
Complications
Various complications can occur in the context of type 1 diabetes. These include acutely life-threatening conditions (hypoglycaemia, ketoacidotic coma) and long-term effects of diabetes (see below). The better the patient's blood sugar levels are, the easier it is to avoid them.
Low blood sugar (hypoglycaemia)
The most common complication of type 1 diabetes is low blood sugar (hypoglycaemia) due to incorrect insulin calculation. It usually manifests itself through symptoms such as dizziness, weakness, nausea and trembling of the hands. Refraining from eating or doing extensive exercise can also lead to hypoglycaemia if the therapy is inadequately adapted.
Ketoacidotic coma
One of the most feared complications of type 1 diabetes is the ketoacidotic coma. In some cases, diabetes mellitus is only discovered when this condition occurs, which occurs as follows:
Due to the absolute lack of insulin in type 1 diabetes, the body cells do not have sufficient sugar (energy). In response to this, the body increasingly breaks down fatty acids from adipose tissue and proteins from muscle tissue in order to gain energy from them.
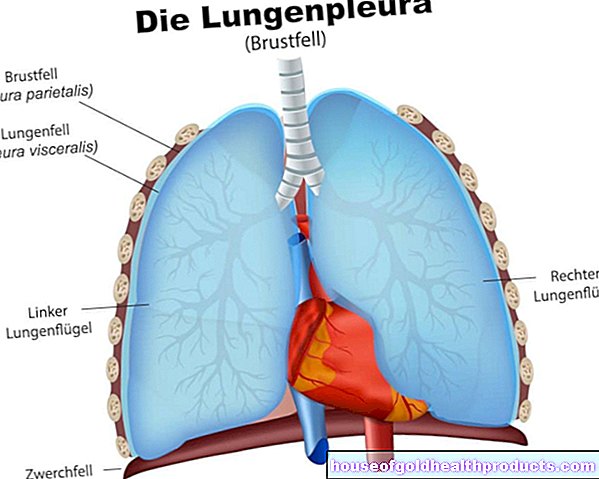
When they are metabolized, acidic breakdown products (ketone bodies) are produced. They cause the blood to become too acidic (acidosis). The body can exhale a certain amount of acid in the form of carbon dioxide through the lungs. The affected type 1 diabetes patients therefore show extremely deep breathing, the so-called Kussmaul breathing. The breath often smells like vinegar or nail polish remover.
In type 1 diabetes, the insulin deficiency can cause the blood sugar level to rise to values in the high hundreds. The body reacts to this by excreting more urine: it excretes excess glucose along with large amounts of fluid from the blood through the kidneys. As a result, it begins to dry out.
The severe loss of fluids and acidification of the blood may be associated with a loss of consciousness. This makes the ketoacidotic coma an absolute emergency! The patients must be treated immediately by intensive care.
You can read more about this metabolic imbalance in our article "Diabetic Ketoacidosis".
Consequences of type 1 diabetes
The secondary diseases of type 1 (and type 2) diabetes are usually based on a permanently poorly controlled blood sugar level. Over time, it damages the blood vessels. Doctors refer to this vascular damage as diabetic angiopathy. It can occur in all blood vessels in the body. In the kidney area, the vascular damage triggers diabetic nephropathy (diabetes-related kidney damage). If the retinal vessels are damaged, diabetic retinopathy is present. Further possible consequences of diabetes-related vascular damage are, for example, coronary artery disease (CHD), a stroke or peripheral arterial occlusive disease (PAD).
The excessively high blood sugar level in poorly controlled type 1 (or 2) diabetes can damage nerves over time (diabetic polyneuropathy) and lead to serious functional disorders. The most common complication in this context is diabetic foot syndrome. It can be associated with persistent wounds (ulcers) that are difficult to heal.
Tags: book tip baby toddler first aid