Vaccines: manufacture and approval
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Vaccines are used for your own protection and that of others: They can prevent you from getting sick yourself and from possibly infecting others. Read here what types of vaccines there are, how they are made and how they have to prove their effectiveness and safety!

What are vaccines?
Vaccines are drugs that are supposed to make the body immune to certain pathogens. So you can protect against infection, which is why one speaks of vaccination.
Experts classify vaccines according to various criteria. A distinction is made between live vaccines and dead vaccines according to the viability or ability of the pathogens contained to reproduce. You can read more about this in the article "Live and dead vaccines".
Recombinant vaccines contain a genetically engineered and particularly typical component of a pathogen (subunit antigen). If so-called vector viruses (live, but not disease-causing viruses) carry this typical antigen on their surface, some experts speak of a recombinant live vaccine.
Gene-based vaccines only introduce the genetic blueprint for a pathogen's antigens into the body. Using these instructions, the body should then produce the foreign antigens itself, which ultimately trigger an immune response. These types of vaccines include DNA and mRNA vaccines, as well as vector vaccines. They were first approved against Covid-19 (coronavirus vaccination).
How are vaccines made?
Normally, the relevant pathogens are grown on a large scale for the production of vaccines. These are then processed, in whole or in part, into a vaccine. There are also some vaccines that contain antigens of a pathogen or their blueprint produced using genetic engineering.
Way of development
Vaccine development generally takes place in several steps:
- Analysis of the respective pathogen and identification of a suitable antigen that elicits an immune response
- Investigation and definition of the vaccine "design" (dead or live vaccination? Whole pathogens or components of them? Use of genetic engineering?)
- Extensive tests in the laboratory, for example on animals, and then on humans; As before drug approval, these take place in three phases. Scientists are testing dosage, tolerability and immune response on more and more volunteers.
- Approval procedure at the vaccination authority
The vaccination should always trigger a stable immune response, which ideally produces better and longer lasting immune protection than the actual infection. However, this must not lead to an excessive defensive reaction that would ultimately do more harm than good. In vaccine development, the tolerance of the vaccine is also important.
Making a vaccine
The vaccine itself is produced in the following way:
- Cultivation of the pathogens against which the vaccine is to act, or genetic engineering of the desired antigens or the appropriate antigen blueprint
- “Harvesting” the antigens, for example viruses from cell cultures or antigens from yeast cells, or the genetic blueprint and subsequent processing
- Supplementation of other components, e.g. to strengthen the vaccine effect (adjuvants), and merging of the components in combination vaccines
- Bottling and packaging
Cultivation of pathogens
The pathogens required for the production of vaccines against bacterial infectious diseases (such as meningococci, typhoid bacteria) can be grown directly in nutrient media. These culture media provide the pathogens with everything they need to survive and multiply. They are then processed into a vaccine in several steps.
The production of vaccines against viral infectious diseases (such as flu, measles, mumps, rubella) is more complicated because viruses can only multiply in living cells. For the cultivation of the huge amount of pathogens that are required for vaccine production, one therefore needs living host cells:
Chicken eggs
Chicken eggs are traditionally used to cultivate viruses: some viruses ("seed viruses") are injected into a fertilized chicken egg, which is then incubated in an incubator. During this time, the pathogens multiply inside. After a few days, they are isolated in complex processes and processed into a vaccine.
The chicken eggs used are not normal eggs that are suitable for consumption and are available in grocery stores. Instead, the eggs for making viral vaccines come from chickens that are kept on special farms under controlled conditions. They have to meet very high quality standards and be completely free from other pathogens (“sterile chicken farming”).
The manufacture of egg-based vaccines is proven, but also time-consuming: it can take six to twelve months for the manufacturing process to be completed. In addition, huge quantities of the special eggs are required for vaccine production - if only for the flu vaccine, which is almost exclusively made in this way. Around the world, around half a billion hen eggs are required for this every year. Because for a single dose of flu vaccine you need one or two eggs.
Cell cultures
Viruses for vaccine production can be obtained faster and more efficiently from animal cell or tissue cultures. They come from monkeys, hamsters, dogs or human fetuses. There are also cell lines that have been genetically immortalized in the laboratory and can therefore be used in the long term for the cultivation of vaccine viruses.
For fully automated production on a large scale, researchers have developed techniques to cultivate the cell lines in large containers (fermenters or bioreactors) - floating in a liquid medium to which all substances are continuously added that the cells need to survive and divide.
Employees use probes to monitor the nutrient supply and, if necessary, adjust it to the growing number of cells. Special pumps continuously filter out cell waste products and used nutrient solution. As soon as a certain cell density is reached, the viruses required for a vaccine are added. They infect the cells, which allows them to multiply in large numbers.
Growing viruses in cell cultures instead of chicken eggs has another advantage in addition to the shorter production time: Corresponding vaccines are guaranteed to be free from chicken protein and are therefore also suitable for people who are allergic to chicken protein. For example, there are cell culture-based flu vaccines.
Genetic engineering
Pathogens do not always have to be multiplied in order to be able to produce a vaccine from them. Once scientists have deciphered the genetic blueprint of their antigens, this or parts of it can be recreated in the laboratory using genetic engineering methods. The artificially produced blueprints are smuggled into bacteria or yeast cells, for example, which then produce the foreign antigens. Such "recombinant vaccines" are available against herpes zoster (shingles), hepatitis B and human papillomavirus (HPV).
Or researchers can use it to gain the blueprint for the desired antigen, which is supposed to turn on the immune system in the human body after the vaccination. If necessary, these construction plans are further processed (e.g. the obtained genetic DNA is translated into messenger RNA) and "packaged". Tiny fat droplets are used for this, or the DNA / RNA snippets are channeled into harmless carrier viruses (vectors). This “packaging” is important because the genetic blueprints are very sensitive and are quickly broken down.
Admission and Security
The approval of a new vaccine is strictly regulated and controlled. The manufacturer has to submit numerous documents on the safety and effectiveness of the new drug to the competent authority (see below: Vaccination authorities). These primarily include:
- Data on the quality of the vaccine with regard to the manufacturing process and the associated quality assurance and control measures
- Data on preclinical testing of the vaccine on animals
- Data on the effectiveness and side effects of the vaccine as found in human clinical studies
There are precise guidelines for quality assurance of the production processes and environment for vaccines and other pharmaceuticals. This "Good Manufacturing Practice" (GMP) includes a documentation of all work steps as well as a regular review of the laboratories, devices, suppliers and the raw material.
The licensing authority reviews and assesses all submitted documents and then decides whether the new vaccine will be approved or not. You can find out more about the approval procedures for drugs in our article "Approval for drugs".
Post-approval monitoring
Even after it has been approved, the authorities keep an eye on a vaccine. In Germany, the Paul Ehrlich Institute (PEI; see below) is responsible for this. It reviews the quality, effectiveness, and safety of each batch of vaccine. The batch is only released for the market if the experts have nothing to complain about on any point.
In addition, doctors are obliged to report any unforeseen side effects of a vaccination to the PEI. It is possible that very rare side effects or long-term effects of the vaccination were not recorded in the clinical approval studies. On the basis of the reported side effects, the PEI can, if necessary, request additional warnings from the manufacturer in the package insert, order the recall of an individual vaccine batch or completely revoke the approval for the vaccine.
The vaccination authorities
A new vaccine must overcome numerous hurdles and meet strict safety regulations before doctors can give these people. For this reason, a control authority was created in Germany over 100 years ago that takes care of the testing and approval of vaccines: the Paul Ehrlich Institute (PEI) in Langen near Frankfurt am Main.
It works closely with the European Medicines Agency (EMA) based in Amsterdam. In this country, the Standing Vaccination Commission (STIKO) at the Robert Koch Institute takes care of the risk-benefit assessment of a vaccination and vaccination recommendations.
Paul Ehrlich Institute (PEI)
The Paul Ehrlich Institute is assigned to the Federal Ministry of Health. It oversees all vaccines and biomedical drugs (e.g. therapeutic antibodies, blood and tissue preparations, drugs for gene therapy).
The following tasks fall within the area of responsibility of the PEI:
- Approval of the clinical trial of vaccines
- Processing of approval applications for new vaccines as well as follow-up applications and requested changes to existing approvals
- State testing and approval of vaccine batches
- Evaluation of drug safety (collecting and assessing the side effects reported by doctors)
- Research in the fields of allergology, bacteriology, biotechnology, immunology, hematology, transfusion medicine, veterinary medicine and virology
- Advising national, European and international bodies on risk assessment and the development of guidelines
European Medicines Agency (EMA)
The EU Medicines Agency (European Medicines Agency) has similar tasks at European level to the Paul Ehrlich Institute in Germany. One of their main tasks is to approve and monitor medicinal products within the EU - not only vaccines and biomedical medicinal products, but also other medicinal products. In addition, like the PEI, the EMA collects reports on side effects that occur. In addition, it can - if necessary - withdraw the approval of a drug or request improvements by the manufacturer.
The EMA works closely with national regulatory authorities in EU countries - as well as with the Directorate-General for Health of the EU Commission and with sister agencies such as the European Center for Disease Prevention and Control (ECDC).
Standing Committee on Vaccination (STIKO)
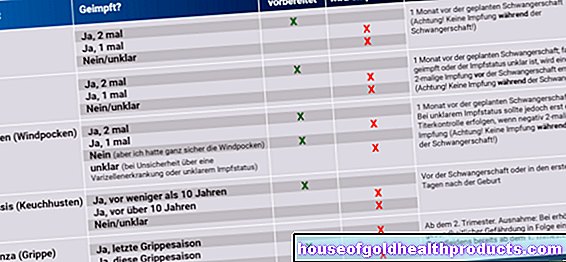
When and how vaccinations should be administered depends largely on the vaccination recommendations of the Standing Vaccination Commission (STIKO) at the Robert Koch Institute. For example, the STIKO publishes vaccination calendars for all age groups. It does not recommend individual vaccines, but basically assesses for which preventable diseases a vaccination makes sense - and for whom.
The STIKO recommendations are initially not legally binding. If the Federal Joint Committee (G-BA) approves the assessment, the recommended vaccination is included in the catalog of mandatory benefits of the statutory health insurance.
Like the Paul Ehrlich Institute and the European Medicines Agency, the Standing Vaccination Commission is also involved in recording unexpected side effects - even if only indirectly. The STIKO develops criteria for distinguishing common vaccination reactions (e.g. reddening of the skin) from serious events. Furthermore, the STIKO gives advice on how to deal with vaccine delivery bottlenecks, i.e. a shortage of vaccines.
Vaccines: New Developments
Vaccines are currently approved against around 30 diseases. In some cases, pharmaceutical companies are working on even better vaccines against some of these diseases. New vaccines against pneumococci are in work that will protect against even more subtypes of the bacterial pathogen than previously available pneumococcal vaccines.
In addition, research is being carried out on completely new vaccines - that is, vaccines against diseases that have not yet been vaccinated against, for example AIDS. Researchers are also working on a vaccine against noroviruses. These pathogens are common triggers of gastrointestinal infections with diarrhea and vomiting worldwide.
Scientists are also intensively researching new processes that enable faster and more efficient vaccine production. The focus here is on the gene-based vaccines mentioned above. As part of the corona pandemic, the authorities approved vaccines of this new generation for the first time (coronavirus vaccination).
Last but not least, therapeutic vaccines are also the subject of research. The aim is not to prevent a disease, but to treat it - for example, cervical cancer caused by HPV. Scientists also want to bring therapeutic vaccines to market. Against HIV, for example, they are supposed to "push" the patient's immune system so that it can keep the viruses under control.
Tags: foot care vaccinations Menstruation