PMS
and Sabine Schrör, medical journalistSophie Matzik is a freelance writer for the medical team.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
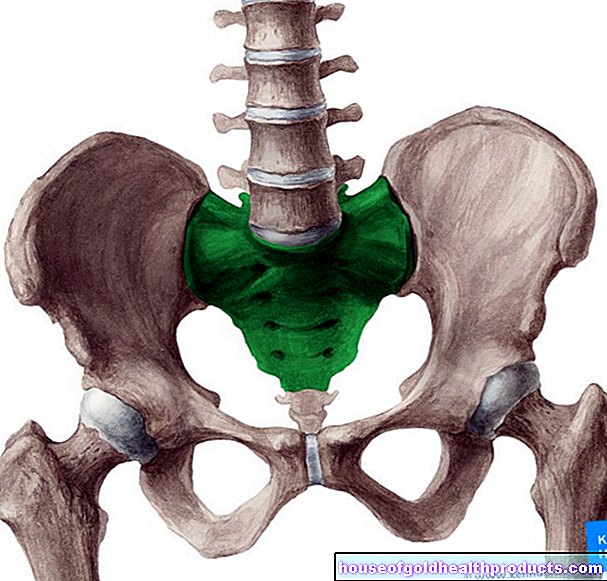
More about the experts All content is checked by medical journalists.PMS (Premenstrual Syndrome) describes physical symptoms such as pelvic pain and / or psychological impairments through to depressive moods that occur before the start of menstrual bleeding. The reasons for this have not yet been fully explored. However, female hormones seem to play a central role. Read everything you need to know about PMS here: symptoms, causes and risk factors, treatment and prognosis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N93N94

Brief overview
- What is PMS PMS is short for Premenstrual Syndrome. It occurs about two weeks to a few days before the start of the menstrual period and is associated with physical and / or psychological symptoms. When your period starts, the symptoms go away. PMS affects around 80 percent of women of childbearing age.
- Symptoms: physical complaints such as pelvic pain, nausea, headache. Psychological symptoms such as sadness, mood swings, depressive moods. The symptoms vary from woman to woman and from cycle to cycle.
- Causes: Not fully understood. Cycle-related fluctuations in the blood levels of female hormones (estrogen, progesterone) probably play a central role.
- Risk factors: stress, relationship problems, unbalanced diet, family history
- Treatment: adequate sleep and exercise, a balanced diet, relaxation and meditation exercises, hot water bottles and hot teas. In severe cases, medication (painkillers, possibly antidepressants, diuretics). Medicinal plants and homeopathics often have a supportive effect.
- Prognosis: PMS is not a disease in the classical sense and therefore cannot be "cured" by medical treatment. After the menopause, the symptoms usually go away.
PMS: symptoms
PMS affects around 80 percent of all women of childbearing age. You will get various physical and / or psychological complaints two weeks to three days before the start of your menstrual period, which will disappear again when your period starts. The type and extent of symptoms vary from woman to woman. Also, they can vary from month to month.
Physical PMS symptoms
Possible physical symptoms of PMS include:
- Abdominal pain
- Sensation of pressure in the lower abdomen
- Diarrhea or constipation
- Circulatory problems, dizziness
- Hot flashes, sweats
- Back pain
- blemished skin, pimples
PMS can also change appetite: some women suffer from food cravings, while others complain of loss of appetite and a feeling of fullness. Nausea before your period and a bloated stomach are also possible. Some women also report gaining weight before their period. This is based less on increased food intake than on the storage of water in the tissue.
Breast tenderness and pre-period breast pain are also possible signs of PMS. Doctors speak of mastodynia here. Stinging or pulling pains are characteristic. Often the breast is enlarged because of the hormonal imbalance before the period, water is stored in the breast tissue. When menstrual bleeding begins, this water retention (edema) recedes.
A distinction must be made between mastodynia and mastalgia. These are chest pain independent of the menstrual period (i.e. independent of the cycle). They can be caused by cysts, a breast infection or breast cancer.
Headaches before your period are also not uncommon with PMS. Many women experience pressure pain in the middle of the head before their menstrual period. For some people, the headache grows into a migraine. In general, before the menstrual period, women can react much more sensitively to stimuli such as bright light, noise, smells or touch, which are then often perceived as extremely unpleasant. In addition, PMS sufferers have less time to deal with time pressure or stress.
Mental PMS Symptoms
Most of the time, PMS is not only associated with physical, but also psychological complaints. Affected women are often irritable in the period before their menstrual period. They also get tired more quickly, need more breaks and more sleep than usual. Other psychological PMS symptoms that are commonly seen include:
- sudden fits of anger
- depressive moods
- greater anxiety
- Disinterestedness
- Listlessness
- inner unrest
- Difficulty concentrating
- sleep disorders
- Hyperactivity
Many women also feel overwhelmed more quickly in the period before their menstrual period. They worry more and feel like they are out of control. Many are also sad or depressed. Often this also affects self-esteem. This increases the overall negative feeling, which in turn can exacerbate other PMS symptoms such as anxiety, difficulty concentrating and sleeping. The women affected often get caught in a cycle of negative emotions.
The sadness or depressive mood before the period often has no objective reason. It can suddenly disappear again. These inexplicable mood swings often lead to problems with partner, family, or friends.
If you have psychological PMS symptoms, it does not mean that you are mentally ill. The mental changes - just like the physical ones - are caused by the changed hormone level, among other things. Just like the physical symptoms of PMS, the psychological symptoms also go away one to two days before the menstrual period.
Common symptoms in PMS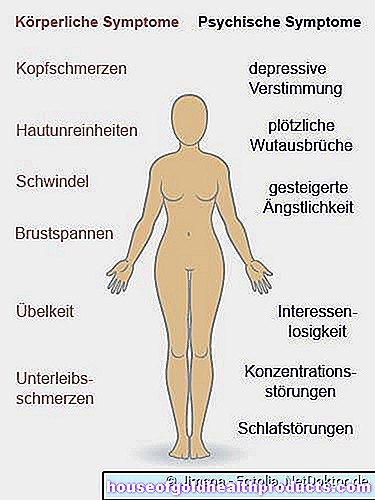
PMS or pregnant?
Some PMS symptoms, such as mood swings, lower abdominal pain, nausea, and food cravings, could also indicate pregnancy. But especially at the beginning of a pregnancy, there are other symptoms that are clearly distinguishable from PMS. These include, above all, morning sickness, a permanently slightly elevated temperature and extreme exhaustion. And at the latest when the next menstrual bleeding does not occur, the question will be answered: PMS or pregnant?
Premenstrual Dysphoric Disorder (PMDS)
In around five percent of people with PMS, the burden of premenstrual syndrome is so great that it affects the normal daily routine, work and family life. These particularly severe cases are known as premenstrual dysphoric disorder (PMDS). In contrast to PMS, it is considered a disease.
-
"Chocolate improves the mood"
Three questions for
Dr. med. Marc Schmidt,
Specialist in Obstetrics and Gynecology -
1
How do I know if I have PMS and not just in a bad mood?
Dr. med. Marc Schmidt
PMS (Premenstrual Syndrome) refers to symptoms such as mood swings, breast tenderness or a feeling of fullness (bloating), which occur only before the start of the menstrual period and disappear again when the bleeding begins. So they are clearly associated with menstruation.
-
2
Why do you get the feeling that chocolate helps?
Dr. med. Marc Schmidt
Eating chocolate increases sugar and insulin levels. This indirectly leads to a "better feeling", but does not change anything about the actual PMS. As a preventive measure, you can try to eat a balanced diet, get enough sleep and exercise. Sometimes monk's pepper (Agnus castus) also alleviates the occurrence of the symptoms.
-
3
As an expert, do you have any tips on the subject?
Dr. med. Marc Schmidt
If the symptoms persist despite the tips mentioned, a hormonal disorder could also be the reason. A thyroid dysfunction or an increase in the hormone prolactin sometimes - like the beginning of the menopause - lead to luteal weakness, which triggers PMS. If you suspect this may be the case, have your hormone levels checked.
-
Dr. med. Marc Schmidt,
Specialist in Obstetrics and GynecologyDr. Schmidt specializes in gynecological endocrinology and reproductive medicine and runs his own specialist practice in Munich.
PMS: causes and risk factors
The causes of PMS have not yet been clearly clarified. Doctors suspect that several factors trigger the symptoms. This is called a multifactorial emergence or multifactorial genesis.
The role of hormones
Hormones seem to be primarily responsible for PMS. These are the body's own messenger substances that transmit messages between different organs and / or the brain. The female sex hormones estrogen and progesterone are particularly relevant for menstrual periods. Together with other female hormones, they ensure that an egg cell matures in each cycle, ovulation (release of the egg cell from the ovary) takes place and the uterine lining is prepared for the implantation of a fertilized egg cell. If fertilization does not occur, the egg cell including the prepared uterine lining is rejected with the menstrual period.
The concentration of estrogen in the blood is highest during ovulation. Many women feel ovulation by a painful pulling in the lower abdomen. In addition, more prolactin is formed during this time. This hormone causes the mammary glands to swell, sometimes causing tension pain in the breasts.
The hormonal changes during the cycle can also cause electrolyte and fluid changes in the body. This could at least be responsible for some PMS complaints. The substances that are produced when the hormone progesterone is broken down are also suspected of triggering PMS symptoms. In addition, people with PMS may be more sensitive to the interactions between progesterone and certain neurotransmitters in the brain such as serotonin.
Other possible causes of PMS
Other factors that could contribute to the development of premenstrual syndrome are:
- low melatonin levels
- Underactive thyroid (hypothyroidism)
- Disorders of the autonomic nervous system
- stress
- Problems in the partnership
- unbalanced diet
- Nicotine use
- little movement
- some hormonal contraceptives
In addition, a family history of mental illness (e.g. depression) is a risk factor for premenstrual dysphoric syndrome (PMDS).
PMS: examinations and diagnosis
If you suspect you have PMS you should discuss this with your gynecologist. The doctor will first ask you about your medical history (anamnesis). Describe your symptoms as precisely as possible so that the doctor can get an exact picture. You should prepare yourself for these questions:
- How long before the menstrual period do the symptoms first appear?
- Are you in pain and if so, where exactly?
- Do the symptoms always occur before your period starts?
- Do you only have physical complaints or do you also feel mentally impaired?
A PMS diary can help in preparation, in which you note over several cycles which symptoms occur and when. This is how you can give your doctor precise information. This will help him rule out other causes for your symptoms.
A physical examination follows after taking the medical history. With a gynecological palpation examination and an ultrasound examination of the uterus and neighboring organs, the doctor can rule out organic diseases such as a tumor as the cause of the symptoms. The doctor will also (possibly together with other specialists) examine whether the symptoms are possibly caused by an underactive thyroid, endometriosis or depression. The onset of menopause must also be ruled out, as PMS-like symptoms can also occur during this time.
A blood test can provide additional information. The expert can use various blood values to determine whether your symptoms are due to hormonal causes. In general, women with PMS symptoms show increased levels of inflammation during symptoms.
PMS: treatment
PMS treatment depends on how intense the symptoms are. In mild cases, it usually helps if you get enough sleep and exercise regularly. A balanced diet is also recommended: Eat a diet rich in carbohydrates, low in salt and easily digestible. Avoid coffee, alcohol and nicotine, as these can exacerbate the PMS symptoms. Pain in the lower abdomen can be relieved with a hot water bottle or hot tea. Many women also use targeted relaxation exercises or meditation.
In severe cases, however, when the symptoms interfere with everyday life, such symptomatic therapy is not enough. Then the PMS should be treated with medication. Pain relievers such as ibuprofen, hormone preparations such as the pill and mood-enhancing drugs (antidepressants) are available for this. Massive water retention (edema) can be treated with water tablets (diuretics). In the case of severe psychological symptoms, psychiatric treatment can be useful.
Sometimes food supplements, for example with magnesium or iron, can also relieve the symptoms. Discuss the use of such preparations with your doctor.
PMS: Homeopathy and Medicinal Plants
Many women rely on complementary healing methods when it comes to PMS. Even if their effectiveness has often not been scientifically proven, many sufferers still report an improvement in their symptoms.
Homeopathy knows various remedies that can be used for PMS. Depending on the type of symptoms, these include, for example, Calcium carbonicum (water retention, especially with swollen breasts), Pulsatilla (sadness with frequent crying), Natrum muriaticum (irritability, sensitivity, crying) and cyclamen (painful swollen breasts, migraine-like headaches, etc.). Women can seek advice from an experienced therapist on the selection of suitable homeopathic remedies.
Herbalism can also help with PMS symptoms. For example, the effectiveness of herbal preparations with monk's pepper has been scientifically well researched. Such preparations are used, for example, when an increased prolactin level causes pain and tension in the breasts. Preparations with St. John's wort help with mildly depressed mood. Valerian and lemon balm are recommended for sleeping problems and nervous restlessness. A doctor or pharmacist can recommend suitable medicinal plants for their PMS symptoms and give advice on how to use them.
PMS: course and prognosis
An exact prognosis for PMS is not possible. Because it is not an acute illness that can be completely cured with therapy. At the latest with the menopause, however, the PMS symptoms generally disappear completely. Until then, in most cases, PMS symptoms can be brought under control with relaxation, adequate sleep and exercise, and a balanced diet.
Tags: skin care anatomy dental care