Medicines for rheumatism
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Rheumatism medication can relieve symptoms such as pain and sometimes also have a positive effect on the course of the disease. Which rheumatic drugs are useful in individual cases depends, among other things, on the type of rheumatic disease. Read here which drugs are available for rheumatism, when they are used and what help herbal anti-rheumatoid drugs can offer!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M15M45M07M79M10M31M08M35M05M32M06
Rheumatism: drugs selected individually
Which drugs are used for rheumatism depends, among other things, on the type of disease. Because "rheumatism" is a collective term for numerous different diseases of the musculoskeletal system that are not caused by an acute injury or a tumor. They are usually associated with pain and often limited mobility. Some rheumatic diseases also affect internal organs or the whole body.
Depending on the clinical picture, different rheumatoid drugs can be considered. When making the selection, the doctor also takes into account the stage of the disease and individual factors such as concomitant diseases or pregnancy.
Rheumatism drugs: the drug groups
Basically, the following groups of active ingredients are available as rheumatism drugs:
- Pain medication
- Glucocorticoid preparations ("cortisone")
- Basic Drugs (DMARD)
Sometimes other drugs are used depending on the rheumatic disease (such as drugs to lower the uric acid level in gout).
A doctor's prescription for rheumatism medication is often required. Common pain relievers such as ibuprofen, diclofenac or paracetamol are available without a prescription - sometimes with restrictions. Diclofenac, for example, requires a prescription for internal use above a certain dosage. Diclofenac preparations are freely available in lower doses and for external use.
Also take over-the-counter medication only after consulting a doctor if you are chronically ill, pregnant or suffer from stomach problems, allergies or blood clotting disorders!
Pain medication
The main symptom of rheumatic diseases is pain. That is why pain medication is an important part of drug therapy for rheumatism. Doctors differentiate between non-steroidal anti-inflammatory drugs (NSAIDs) and pure pain relievers (analgesics).
The attending physician will select a suitable pain medication in the appropriate dosage for each patient. If necessary, he also prescribes two or more preparations.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are very common anti-rheumatic drugs: They can, among other things, very quickly and effectively relieve pain (analgesic effect) and also inhibit inflammation (anti-inflammatory).
This is of particular advantage in the case of inflammatory rheumatic diseases such as rheumatoid arthritis, ankylosing spondylitis or psoriatic arthritis. But NSAIDs can also be taken for other rheumatic diseases, such as an acute gout attack - gout also belongs to the rheumatic group of forms, more precisely to the metabolic diseases that are associated with rheumatic complaints.
There are two groups of NSAIDs:
- Classic NSAIDs (unselective inhibitors of cyclooxygenase COX), e.g. acetylsalicylic acid (ASA), ibuprofen, naproxen, diclofenac, indomethacin, phenylbutazone
- Selective COX-2 inhibitors (coxibs): further development of the classic NSAIDs; Etoricoxib, celecoxib and parecoxib are approved in Germany
Of all NSAIDs, diclofenac, ibuprofen and naproxen are used in rheumatism therapy.
Side effects
NSAIDs can cause serious gastrointestinal problems such as ulcers and bleeding. This applies primarily to classic NSAIDs and less so to coxibs. The risk of gastrointestinal complications arises particularly when the preparations are taken for a long time and in higher doses or several NSAIDs are combined with one another. People over the age of 60 and those with previous gastrointestinal illnesses are also susceptible to such side effects.
Other possible side effects of NSAIDs include disorders of kidney function (acute kidney failure, analgesics), cardiovascular problems (such as increased blood pressure, heart attack, stroke; not ASA or naproxen; however, diclofenac is contraindicated) and water retention in the tissue (edema).
Pure pain relievers (analgesics)
Sometimes pure painkillers for rheumatism, so-called analgesics, are also administered. Because, unlike NSAIDs, they have no influence on inflammation, they are preferred for rheumatic diseases that are not caused by inflammation. This is the case, for example, with painful joint wear without inflammation processes (non-activated osteoarthritis).
But even with inflammatory rheumatic diseases, pure analgesics can sometimes be useful - for example in the case of contraindications for NSAIDs and if treatment with basic medication alone cannot sufficiently relieve rheumatic pain. The doctor will also prescribe analgesics for patients who cannot tolerate NSAIDs.
The pure pain relievers are divided into two main groups:
- Non-opioid analgesics: They inhibit the sensation of pain in the peripheral nervous system (for example in the legs and arms). The best known is paracetamol, which is often used as an antipyretic agent due to its good antipyretic properties. Another representative is, for example, metamizole.
- Opioid analgesics: They inhibit the sensation of pain directly in the central nervous system (brain and spinal cord). There are low-potency opioids such as tramadol, tilidine (/ naloxone) and codeine, as well as high-potency opioids, the most powerful pain relievers. Well-known representatives are, for example, fentanyl, morphine and oxycodone.
Side effects
The main side effect of acetaminophen is liver damage. Therefore, this pain reliever must not be taken if someone already has impaired liver function (e.g. as a result of chronic hepatitis or liver cirrhosis). With the active ingredient metamizole there is a particular risk of blood formation disorders (agranulocytosis).
Opioid analgesics can cause fatigue, nausea, vomiting, constipation and urinary retention, among other things. Opioids also reduce breathing and make you sleepy, which is life-threatening in the event of an overdose. In principle, they can also be addictive. However, if they are used under medical supervision and as a sustained release preparation or patch (slow release of active ingredients), the risk of psychological dependence is very low.
However, from a certain dose, physical dependence can develop. Therefore, treatment with opioid analgesics must never be stopped abruptly - physical withdrawal symptoms would be the result. Instead, the dosage must be gradually reduced if you want to end the therapy ("tapering off" the therapy).
cortisone
Cortisone preparations imitate the effects of the body's own hormone cortisol (cortisol or hydrocortisone) and its precursor cortisone (cortisone). In this way, among other things, they can inhibit inflammation (more strongly than NSAIDs). They also have an inhibitory effect on the immune system (immunosuppressive effect), which helps against excessive immune reactions.
This means that cortisone preparations are primarily suitable for the treatment of inflammatory rheumatic diseases (autoimmune diseases). These are based on a malfunction of the immune system in which the defense cells attack the body's own tissue (e.g. rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, polymyalgia rheumatica).
Side effects
Short-term use of cortisone most commonly results in dizziness, nervousness, headache and / or euphoria. Psychological changes with hallucinations, delusions or states of anxiety only occur very rarely.
With prolonged use, cortisone preparations can trigger a variety of side effects. These include, for example, an increased risk of infection, osteoporosis, increased blood sugar levels (with the risk of cortisone diabetes), muscle weakness, cataracts, glaucoma, skin changes (such as paper-thin skin, acne), high blood pressure and water retention (edema). In addition, long-term therapy with cortisone can lead to a full moon face, bull neck and obesity in the trunk area (trunk obesity).
Most of the side effects only occur when taking cortisone over a long period of time and in high doses.
Make sure you take a stomach protection, especially if you combine NSAIDs with cortisone preparations! Talk to your doctor about this!
Basic Drugs (DMARD)
The basic drugs ("Disease Modifying Anti Rheumatic Drug", DMARD) form the basis of drug therapy for a certain group of rheumatic diseases: inflammatory rheumatic diseases.
Pain medication and cortisone supplements can quickly relieve patients' symptoms. However, they do not influence the course of the disease - in contrast to basic drugs (basic therapeutic agents): These can stop the progression of a rheumatic-inflammatory disease or at least slow it down. In the best case scenario, permanent consequences of illness such as joint destruction or organ damage can be prevented. To do this, however, these rheumatoid drugs must be taken for a longer period of time.
In particular, the early start of treatment with DMARD rheumatoid drugs can sustainably improve the prognosis.
Doctors distinguish three groups of DMARDs:
- Classic basic drugs: conventional synthetic DMARDs ("conventional synthetic DMARDs"), in short: csDMARDs
- Biologics: biotechnologically produced DMARDs, in short: bDMARDs
- Targeted synthetic basic drugs: "targeted synthetic DMARDs", in short: tsDMARDs
Sometimes only one basic drug is prescribed alone (monotherapy), in other cases two or more DMARDs are given (combination therapy). This depends on the type, duration and stage of the inflammatory rheumatic disease, the degree of inflammatory activity and any concomitant diseases.
Classic basic drugs (csDMARDs)
This group includes rheumatoid drugs with different modes of action. Some of them were originally developed against other diseases and only later found their way into rheumatism therapy. However, the following applies to all classic basic medications: They do not work immediately, but only after a few weeks or months.
Methotrexate (MTX) is an important csDMARD. The active ingredient, which was actually introduced as a cancer drug, is now also used - in lower doses - as a rheumatoid drug. Methotrexate is even the classic basic drug most frequently used worldwide for inflammatory rheumatic diseases. It is taken once a week.
Taking folic acid a day or two after methotrexate reduces side effects.
Other classic basic medications for rheumatism are, for example:
- Leflunomide (common alternative to MTX if it is not tolerated or if it cannot be taken due to contraindications)
- Sulfasalazine (also helps with inflammatory bowel diseases such as Crohn's disease)
- Chloroquine or hydroxychloroquine (actually malaria drugs)
- Azathioprine (also used as a cancer drug and used to suppress the immune system after organ transplants and in autoimmune diseases)
- Ciclosporin (used to suppress the immune system after organ transplants and for autoimmune diseases)
Gold supplements were also used as DMARDs in the past. Because of their strong side effects, they are largely avoided today.
You can find more information about the respective medication, for example side effects, in the associated medication articles.
Biologics (bDMARDs)
Biologics are biotechnologically produced proteins - obtained from living cell cultures. They can switch off certain inflammatory messengers or block their binding sites and thus their effect. There are different types of biologics that are used (among other things) as anti-rheumatic drugs:
- TNF-alpha inhibitors: They block the inflammatory messenger substance tumor necrosis factor-alpha. This group of active ingredients includes, for example, adalimumab, etanercept and infliximab.
- Interleukin blockers: They inhibit the effects of various interleukins. These are messenger substances of the white blood cells (leukocytes) to regulate immune reactions. Examples of interleukin inhibitors are tocilizumab and anakinra.
- Immune cell inhibitors: They are specifically directed against immune cells that play a role in inflammatory rheumatic diseases: Abatacept prevents the activation of T lymphocytes, while rituximab and belimumab reduce the number of B lymphocytes.
Biologics as rheumatism drugs are very effective: The drugs administered as syringes or infusions work faster than classic basic drugs (csDMARDs) and effectively slow the progression of the disease. However, they are very expensive.
Rheumatism biosimilars
Copycat biologics, so-called biosimilars, are somewhat cheaper. Patent protection for many biologics has now expired. Therefore, they can be "copied" by any pharmaceutical company. These replicas - the biosimilars - are just as safe and effective as the respective original preparation.
However, they are not identical, but differ slightly from the original structure - unlike so-called generics (production in living cell cultures can never be copied identically). Just like the originals, biosimilars are administered either as a syringe or an infusion. There are biosimilars available for example for etanercept, infliximab or rituximab.
Treatment with biologics / biosimilars is usually combined with methotrexate. The classic basic drug can increase the effect of biologicals. At the same time, it can prevent the immune system from forming antibodies that eliminate the biological agents (foreign proteins) before they can take effect.
Side effects
Biologics and biosimilars can make you more susceptible to infections (including "sleeping" infections) such as tuberculosis because they depress the immune system. That is why the doctor usually only prescribes these anti-rheumatoid drugs if, for example, treatment with classic basic drugs - including methotrexate - has not had sufficient effect (another reason for this is the high cost of the biotechnological drugs).
Another possible side effect of biologics / biosimilars is hypersensitivity reactions. In addition, the drugs can impair the function of various organs (such as the liver, kidneys).
Targeted Synthetic Base Drugs (tsDMARDs)
Targeted synthetic DMARDs are among the newest drugs for rheumatic diseases with an inflammatory background. They specifically interrupt an inflammatory signal path within cells. The following are currently approved in Germany:
- The JAK inhibitors tofacitinib, baricitinib and upadacitinib: They block enzymes called Janus kinases and are used, for example, in rheumatoid arthritis, and tofacitinib in psoriatic arthritis.
- the PDE-4 inhibitor apremilast: This active ingredient inhibits the enzyme phosphodiesterase-4 and is approved for the treatment of psoriatic arthritis.
The targeted basic drugs (tsDMARDs) are used in tablet form. They come into consideration when classic basic medications do not work sufficiently (they are often prescribed in combination with methotrexate). In addition, tsDMARDs are suitable for the treatment of patients who cannot tolerate the other rheumatoid drugs of the basic therapy.
Side effects
Tofacitinib can cause headaches, upper respiratory infections, high blood pressure, diarrhea, and nausea. With baricitinib, high cholesterol, upper respiratory and urinary tract infections, and nausea are among the most common undesirable effects. Upadacitinib mainly causes upper respiratory infections, nausea and coughs.
In studies of apremilast, participants mainly reported (transient) gastrointestinal symptoms such as nausea and diarrhea. Upper respiratory infections and headaches were also more common side effects. In addition, apremilast can lead to weight loss.
Rheumatism drugs that suppress the immune system (immunosuppressants) make you more susceptible to infections. Therefore, pay attention to your vaccination status, which is usually also checked by the attending physician.
Other drugs for rheumatism
In the case of individual rheumatic diseases, other drugs can also be considered - in addition to or as an alternative to the above-mentioned drugs. Some examples:
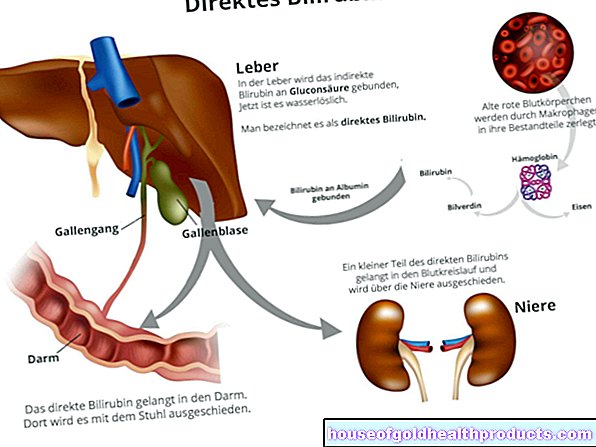
gout
In the case of gout, long-term treatment with drugs that inhibit the formation of uric acid (uricostatic drugs such as allopurinol) or stimulate its excretion (uricosuric drugs such as benzbromaron) can make sense. In the meantime, there are also combination preparations made from uricostatics and uricosurics.
An acute attack of gout is preferably treated with nonsteroidal anti-inflammatory drugs (NSAIDs). If necessary, the doctor may also administer cortisone - for example as tablets or as an injection directly into the affected joint.
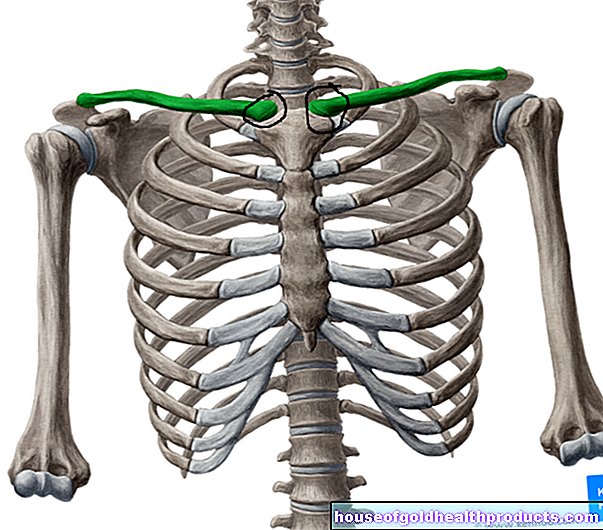
osteoporosis
Like gout, osteoporosis (bone loss) is one of the metabolic diseases associated with rheumatic complaints. Many patients take a vitamin D supplement and calcium to strengthen their bones. Osteoporosis-related pain can be relieved with pain relievers (such as NSAIDs).
Calcium and vitamin D can only work properly if the person concerned moves enough.
If a patient is at high risk of fractures, special osteoporosis medications can also be considered. These can either slow down bone loss (e.g. bisphosphonates, denosumab) or promote bone formation (teriparatide).
Fibromyalgia
In fibromyalgia (generalized soft tissue rheumatism), classic pain relievers such as ibuprofen, diclofenac or paracetamol usually do not help at all or only little. Instead, doctors often prescribe antidepressants (especially amitriptyline) for patients. These can not only alleviate the psychological concomitant illnesses that are often associated with fibromyalgia (e.g. depression, fears) - pain and tiredness often also decrease under antidepressant therapy.
Some fibromyalgia patients also benefit from anti-seizure drugs (anti-epileptic drugs) such as pregabalin.
Herbal anti-rheumatic drugs
In addition to conventional medical treatment, some patients also use herbal remedies for rheumatic complaints. Sometimes the effect is medically recognized (such as that of the devil's claw against osteoarthritis complaints), in other cases the application is based on many years of experience in folk medicine. For example:
- African devil's claw root: According to the European Committee for Herbal Medicines, it is a traditional remedy for mild joint pain. It is therefore used as a support for osteoarthritis and rheumatoid arthritis, mostly as a ready-made preparation (e.g. capsules, tablets, ointment, balm). Devil's claw root tea is mainly recommended for those with mild digestive problems.
- Nettle: Preparations such as fresh plant juice, capsules and drops are taken to reduce inflammation, for example in inflammatory rheumatic diseases. Tea made from nettle leaves is also popular, often combined with other medicinal plants (such as willow bark).
- Willow bark: its anti-inflammatory and pain-relieving effect is based on the salicylic acid compounds it contains (starting point for the anti-inflammatory and pain reliever acetylsalicylic acid). In the form of capsules or as a tea, the medicinal plant is used, for example, for osteoarthritis and rheumatoid arthritis.
- Quivering aspen: Like willow, it contains anti-inflammatory and pain-relieving salicylic acid compounds - especially in the bark. This is therefore used, among other things, for rheumatic complaints, often in combination with other medicinal plants such as ash (also contains salicylic acid compounds).
- Birch: Birch leaf preparations (e.g. fresh plant juice, drops, capsules, tea) can support the treatment of rheumatoid arthritis and gout, for example.
- Arnica: The medicinal plant is only used externally! Rheumatic muscle and joint pain are treated with arnica cream, ointment or gel, for example. Arnica tincture is also available, which can be diluted and used for compresses.
- Frankincense: The resin of the frankincense tree has anti-inflammatory and pain-relieving properties, among other things. It may only be used in the form of standardized ready-to-use preparations (e.g. capsules), e.g. for rheumatoid arthritis.
- Cayenne pepper: Applied externally (e.g. as an ointment or active ingredient plaster), the hot substances contained trigger a pain and heat stimulus on the skin, which ultimately leads to longer-lasting pain relief - for example in osteoarthritis and rheumatoid arthritis.
Three pillars of phytotherapy for rheumatism
The use of herbal remedies for rheumatism complaints is often based on three pillars:
- Metabolic stimulation and detoxification: With the help of medicinal plants such as birch, nettle, goldenrod or dandelion, excretion via the kidneys is stimulated. The dandelion, like yarrow or milk thistle, also stimulates the flow of bile. Excretion via the intestines and skin can be promoted with wild garlic, garlic, elderberry and linden, for example.
- Internal use of herbal anti-rheumatic drugs: To relieve rheumatism-related pain and inflammation, for example, preparations based on devil's claw, nettle, incense or willow bark are taken. It usually takes about three weeks for them to take full effect.
- External use of herbal remedies for rheumatism: ointments, rubs, poultices etc. can locally and quickly relieve pain and inflammation and stimulate the metabolism, depending on the medicinal plant used. Arnica, comfrey, cayenne pepper and mustard are suitable for this.
Phytotherapy cannot replace traditional rheumatism treatment in conventional medicine.
Herbal anti-rheumatic drugs can help against the symptoms in a variety of ways. If you are considering additional herbal rheumatism therapy, you should seek advice from an experienced doctor or naturopath. He can tell you which preparations and applications make the most sense in your case. With the healing power of plants, conventional medical treatment with rheumatism drugs and other therapeutic measures (such as physiotherapy, physical procedures, regular exercise) can be effectively supplemented.
Tags: alcohol drugs menopause Diagnosis