pre-eclampsia
and Martina Feichter, medical editor and biologistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Preeclampsia (formerly: EPH gestosis) is a serious disease in pregnant women. It is one of the so-called hypertensive pregnancy diseases. These are diseases with high blood pressure in pregnancy. Women with preeclampsia also have protein in their urine and water retention in their tissues (edema). Read more about symptoms, treatment, prognosis and prevention of preeclampsia here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. O14
What is preeclampsia?
Preeclampsia is one of a number of diseases that are associated with high blood pressure during pregnancy. It used to be called EPH gestosis, where E stands for "Edema" (English for edema = water accumulation), P for "protein" and H for "hypertension" (= high blood pressure). The abbreviation summarizes the typical preeclampsia symptoms. The term gestosis generally stands for a pregnancy-related illness.
Preeclampsia: causes and risk factors
The exact cause of preeclampsia is not known. But there are different explanations for the development of the disease. Presumably, the affected women have impaired adaptation of the organism to pregnancy.
Preeclampsia: Who is at Risk?
Preeclampsia occurs in around three to five percent of all pregnant women who are expecting a child for the first time (first-time women). In pregnant women who have already given birth to one or more children (multiparous women), the risk of preeclampsia is only about 0.5 percent. However, it increases again when multiparous women have a new life partner and have a child with him for the first time. This indicates that immunological factors are involved in the development of the disease.
Other risk factors for preeclampsia include:
- Family predisposition (if, for example, the mother of the pregnant woman also had an EPH gestosis)
- Multiple pregnancy
- artificial insemination (in vitro fertilization) or egg donation
- Late births (> 40 years)
- Obesity (Obesity): Body Mass Index (BMI) 30 or higher
- Preeclampsia in a previous pregnancy (risk of recurrence 11.5 to 27%)
- pre-pregnancy high blood pressure
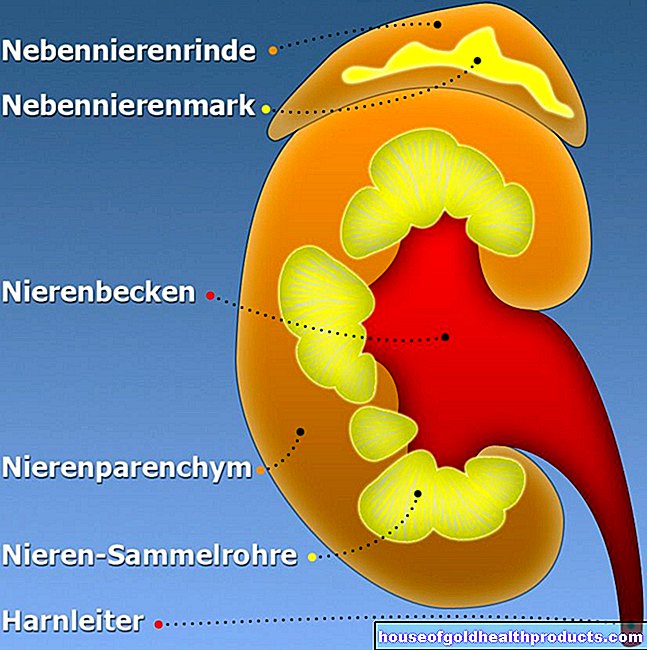
- Kidney disease
- Diabetes mellitus
- Antiphospholipid syndrome or other autoimmune diseases
- Malformations of the unborn child such as hydrops fetalis (accumulation of fluid in the child's body), trisomies (such as trisomy 21)
- increased vascular resistance in the arteries of the uterus
Preeclampsia: symptoms
Basically, several forms of gestures can be distinguished, depending on the point in time in pregnancy at which they occur. Depending on the form, the symptoms that appear can be different:
- Premature gestosis: It occurs in the first trimester of pregnancy (2nd to 4th month of pregnancy). This variant is often accompanied by insatiable vomiting (hyperemesis gravidarum).
- Gestational hypertension: This is high blood pressure caused by pregnancy. It appears from the 20th week of pregnancy with values above 140/90 mmHg and usually normalizes within about six weeks after the birth. Before the 20th week of pregnancy, the affected woman's blood pressure was in the normal range. Gestational hypertension can develop into mild, less often severe, preeclampsia.
- Late gestosis: This is the actual preeclampsia. It occurs at the earliest from the 20th week of pregnancy.
Typical preeclampsia symptoms are:
- High blood pressure (more than 140/90 mmHg)
- Excretion of protein in the urine (proteinuria over 300 milligrams per day) *
- Water retention (edema) in the tissue, causing swelling of the face, hands and feet
* If proteinuria is absent, preeclampsia is still likely if, in addition to high blood pressure, there are pathological findings in the kidneys, liver, lungs, blood system, placenta or the central nervous system.
In severe cases, pregnant women with preeclampsia also suffer from other symptoms such as nausea and vomiting, dizziness, visual disturbances or confusion.
Eclampsia
Sometimes preeclampsia turns into eclampsia. Then there are the following symptoms:
- strong headache
- Flicker before the eyes
- general malaise
- Seizures that have no neurological cause such as B. Epilepsy are to be assigned
Eclampsia is an emergency and needs immediate hospital treatment! In most cases, the pregnancy is then terminated by a caesarean section.
Identify and treat preeclampsia
The doctor usually recognizes preeclampsia on the basis of the typical symptoms: As part of prenatal care, the gynecologist checks, among other things, blood pressure, urine and body weight in every pregnant woman. He also looks out for risk factors like old age and obesity. A sudden increase in blood pressure, a rapid increase in weight of 21 kilograms in the III. The trimester (due to water retention), pronounced facial edema and protein in the urine are clear indications of preeclampsia.
If preeclampsia is suspected, the pregnant woman must be closely monitored. For blood pressure values of 150/100 mmHg or more, an inpatient stay in the hospital is necessary.
For mild preeclampsia before the 36th week of pregnancy (SSW), the therapy consists of rest and physical rest (sometimes bed rest). The pregnant woman also receives a protein-rich diet and should drink enough fluids. Your condition and that of your child will be closely monitored by a doctor.
Depending on the active ingredient, antihypertensive drugs can be problematic for child development. They are therefore only possible with blood pressure values of ≥ 150 mmHg systolic and / or ≥ 100 mmHg diastolic.
If the unborn child shows stress reactions in the contractions recorder (CTG), the pregnant woman is given medication that stimulates the child's lung maturation (usually a cortisone preparation). Then the woman is delivered as soon as possible, often by caesarean section. If possible, try to wait for at least the 37th week of pregnancy to be completed.
In severe preeclampsia, therapy focuses on three goals:
- preventing ecstatic seizures (usually with magnesium sulfate)
- checking maternal blood pressure (bed rest, antihypertensives)
- childbirth (as soon as possible from the 34th week of pregnancy)
By the way: In preeclampsia, delivery does not necessarily have to take place by caesarean section. If the condition of the pregnant woman and the child allow it, a "normal" (vaginal) birth may also be possible. However, this also depends on the severity and dynamics of the disease as well as the chances of success of the vaginal birth.
Preeclampsia: prognosis
The earlier preeclampsia occurs in pregnancy, the greater the risk that it will become severe. Without treatment, the disease can develop into eclampsia: the seizures that occur can be life-threatening for both the expectant mother and the unborn child. Pregnant women should therefore definitely attend the regular check-up appointments with the gynecologist: This way, any preeclampsia can be detected and treated at an early stage.
Preeclampsia: Prevention
In women with risk factors (such as severe preeclampsia in an earlier pregnancy), preeclampsia can be prevented to a certain extent with medication: The pregnant woman begins in early pregnancy (if possible before the 16th week of pregnancy) with a daily intake of 150 milligrams of acetylsalicylic acid ( ASS). The intake is continued until the end of the 34th to 36th week of pregnancy.
This ASA prophylaxis lowers the risk that the woman will develop preeclampsia before the 37th week of pregnancy. The risk of illness in later pregnancy remains unaffected.
Tags: baby toddler pregnancy elderly care