COPD
and Martina Feichter, medical editor and biologistDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
COPD (chronic obstructive pulmonary disease) is a chronically progressive disease of the lungs. It is characterized by inflamed and permanently narrowed airways. Typical COPD symptoms are coughing with phlegm and shortness of breath when exercising, later also at rest. The greatest risk of COPD are smokers and passive smokers. You can find out everything you need to know about the causes, symptoms, diagnosis and treatment of COPD here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J44
COPD: quick reference
- Main cause: smoking (chronic smoker's cough)
- Typical symptoms: shortness of breath, cough, sputum
- Possible complications: frequent bronchial infections and pneumonia, cor pulmonale, emphysema
- Investigations: lung function test, blood gas analysis, chest x-ray (chest x-ray)
- Treatment: Depending on the COPD stage, stop smoking, medication, exercise, breathing and physiotherapy, long-term oxygen therapy, operations (including lung transplantation)
COPD: description
COPD is often played down as "smoker's lung" or "smoker's cough". COPD is a serious lung disease that, once started, progresses and often leads to premature death.
COPD is widespread: In Germany, around ten percent, or eight million people, suffer from it. Experts predict that this number will rise to ten million by 2020. COPD is one of the most common causes of death.
COPD: definition and important terms
What is COPD exactly? The abbreviation stands for the English term "chronic obstructive pulmonary disease". In German this means "chronic obstructive pulmonary disease" or in technical terms "chronic obstructive bronchitis" (COB). The terms "chronic bronchitis" and "pulmonary emphysema" are associated with COPD:
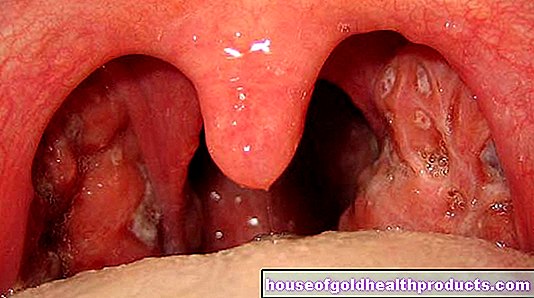
Chronic bronchitis: According to the WHO, chronic bronchitis is present if cough and sputum (productive cough) persist for at least three months in two consecutive years. One speaks of “simple chronic bronchitis” if coughing and sputum occur only once due to overproduction of mucus in the lungs. At this stage, the changes in the lungs can still regress if the cause (for example, smoking) is eliminated. If this does not happen, the chronic bronchitis can develop into COPD.
Chronic bronchitis
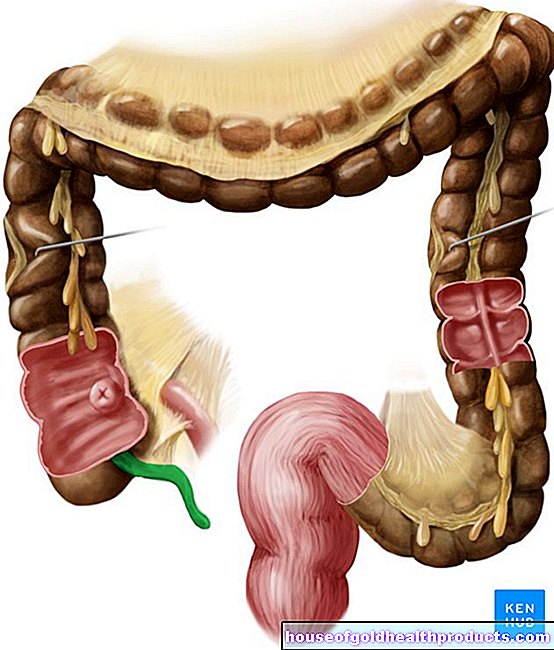
COPD: The lung disease is usually a combination of chronic obstructive bronchitis and pulmonary emphysema - hence the term "chronic obstructive pulmonary disease". The changes in the lungs cannot be completely reversed at this stage.
Pulmonary emphysema: Pulmonary emphysema is an over-inflated lung. In the course of COPD, the wall structure of the alveoli (alveolar septa) can be destroyed, which irrevocably expands the air spaces. The lungs then no longer look like a vine with grapes (like a healthy person), but like a large balloon. Doctors speak of emphysema (overinflation of the lungs).
Pulmonary emphysema in COPD
Exacerbated COPD: The term exacerbation stands for a relapsing, sudden worsening of COPD. Symptoms such as chronic cough, shortness of breath and mucous sputum increase acutely. Exacerbations can be a stressful and threatening event for patients. An exacerbated COPD is a sign that lung function is deteriorating rapidly. The infection-exacerbated COPD is also accompanied by a viral or bacterial infection.
COPD: causes and risk factors
COPD can have various causes. In the vast majority of cases it is "homemade" - through smoking.
Main cause: smoking
The main cause of COPD is active or passive smoking. Around 90 percent of all COPD patients are smokers or ex-smokers. The lungs and bronchi suffer most from constant nicotine consumption. The risk of COPD in smokers and ex-smokers is seven times higher than in people who have never smoked. About 20 percent of long-time cigarette smokers develop COPD. Every second smoker in over 40-year-olds suffers from “smoker's cough”. Men are affected much more often than women.
Alpha-1 antitrypsin deficiency
Smoking is not always the cause of the complaints. In some patients, the chronic lung disease is based on a genetic deficiency in the protein alpha-1-antitrypsin (AAT): This blood protein inactivates so-called proteases - enzymes that are supposed to break down tissue destroyed during inflammation processes. In people with a deficiency of AAT, however, the proteases can damage the lung tissue unchecked. The result is chronic inflammation with narrowing of the bronchi, just like with COPD caused by harmful substances. As the disease progresses, emphysema can develop. In addition, an AAT deficiency can lead to liver damage and promote cirrhosis of the liver.
AAT deficiency is about as common as type 1 diabetes in Europe, but it does not receive the same amount of attention. This is why the hereditary disease is often not recognized and treated in good time.
Other causes of COPD
Another possible cause of COPD is air pollution. Above all, nitro gases and sulfur dioxide (SO2) play a role here. Studies have shown that living on busy streets with high levels of particulate matter increases the risk of COPD. Frequent infections in childhood also increase the likelihood of developing COPD.
Chronic lung disease can also be caused by harmful dusts, vapors, smoke or gases to which some people are exposed in the workplace. In the case of non-smokers, the risk of developing COPD later is increased by a factor of 2.4.In smokers, the risk of illness is even 18 times higher.
A very rare cause of COPD is the congenital lack of antibodies (antibody deficiency syndrome).
COPD: Mechanism of Development
The starting point for COPD is usually obstructive bronchitis: inhaled pollutants inflame the small airways, the bronchioles. The lungs secreted more mucus as protection. The mucus is usually carried by the cilia in the direction of the exit (throat). These are the finest, mobile hairs (cilia) on the surface of special cells that line most of the airways (ciliated epithelium).
Pollutants such as nicotine destroy the cilia, so that the ciliated epithelium gradually loses its ability to clean and transport. Eventually it is replaced by a more resilient squamous epithelium, causing the lung tissue to thicken. The wall of the alveoli becomes thin and unstable when you breathe out. If the person concerned tries to exhale with all his strength, the alveoli collapse. Ultimately, this process leads to the airways constricting permanently. The consequences are shortness of breath and poor performance.
COPD: a vicious circle
People who cannot or do not want to stop smoking encourage the vicious cycle of COPD. Basically, it is determined by two factors:
On the one hand, the excessively produced mucus can block the small airways. As a result, when you breathe in, the air you breathe just barely gets into the alveoli due to the negative pressure. When you exhale, however, the air can no longer be pressed out completely, so that residual air still remains in the blisters. The next time you take a breath, more air remains in the bubbles. This slowly increases the pressure in the lungs. As a result, the small alveoli connect with one another and become larger and larger, so-called emphysema bubbles. Overall, this reduces the surface of the bubbles.
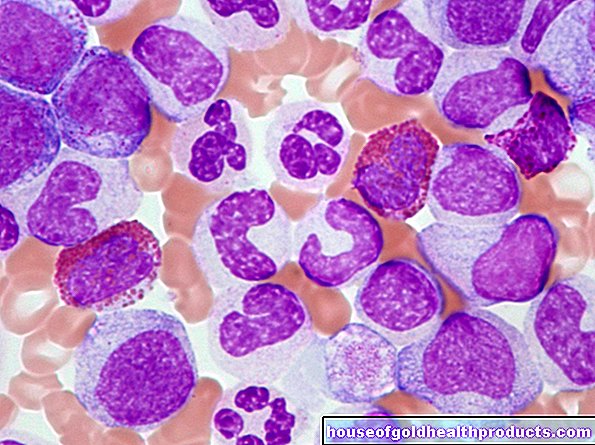
On the other hand, inhaled pollutants and lung infections destroy the lung tissue. Proteases and protease inhibitors play a role here. Proteases are enzymes that break down proteins and can therefore be damaging to cells. Protease inhibitors, in turn, inhibit the breakdown of protein and thus have a protective effect. Alpha-1 antitrypsin is the main protease inhibitor. Lung infections cause more proteases to be released. Nicotine, in turn, incapacitates the protease inhibitors so that they cannot perform their protective function. As a result of this imbalance of proteases and protease inhibitors, the lung tissue becomes more unstable and the wall structure of the small alveolar sacs (alveolar septa) perishes.
Consequences of COPD
COPD has serious consequences:
For the lungs, COPD means a loss of elasticity and an increase in residual volume (volume of air that remains in the lungs after exhaling and cannot be freely exhaled).
The small airways are increasingly obstructed and place extreme stress on the respiratory muscles. This increases the amount of carbon dioxide in the blood (hypercapnia).
With the alveolar septa, the pulmonary capillaries are also lost. These are tiny connecting vessels between arteries and veins. Because the airways are inadequately ventilated, less oxygen reaches the blood vessels. As a result, the blood vessels constrict and the lungs are ultimately less supplied with blood. Doctors also call this mechanism the Euler-Liljestrand reflex. It prevents blood from passing through the lungs without being supplied with oxygen. Due to the narrowed pulmonary arteries, the blood pressure in the pulmonary circulation increases, which in turn puts a strain on the right heart. The result is a so-called cor pulmonale (lung heart). It causes shortness of breath under exertion or even at rest.
COPD: symptoms
An adult's lungs hold an average of five to six liters. We only breathe in and out half a liter of it without physical exertion. The lungs therefore have relatively large reserves. A gradual deterioration in their function therefore usually goes unnoticed for years. Those affected often neglect the first symptoms of COPD as a "smoker's cough" that they can no longer get rid of. However, it is important for the course of the disease to recognize and treat COPD symptoms early on.
By the way: If COPD is caused by an AAT deficiency and the lungs are additionally burdened by smoking or infections, the disease progresses faster than normal. Typical COPD symptoms then show up much earlier.
Typical COPD symptoms
Typical symptoms of COPD are cough and sputum. Shortness of breath also occurs, initially only during exercise, especially if the COPD symptoms worsen (exacerbation). Blue lips or fingers are signs of cyanosis, which is a decreased supply of oxygen as a result of deteriorating lung capacity.
Here are the most important COPD symptoms again:
- Shortness of breath, initially only when exercising, later also at rest.
- Cough that gets worse and more persistent over time.
- Sputum that is getting thicker and harder to cough up.
Based on the characteristic COPD symptoms, shortness of breath, coughing and expectoration, many doctors speak of AHA symptoms.
How does the smoker's cough arise?
The chronic cough (smoker's cough) in smokers is one of the characteristic symptoms of COPD and a risk factor for a deterioration in lung function. It arises as follows:
The cilia in the lungs are gradually destroyed by smoking and lose their cleaning function. Therefore, the body has to cough up the secretion that has accumulated, especially at night. The typical smoker's cough is therefore particularly agonizing in the morning after getting up. In the course of the day, many patients are relatively symptom-free. The sputum is greyish in color in smokers.
COPD symptoms: complications
COPD is a chronic, progressive disease. Therefore, see your doctor regularly. If you are largely symptom-free, it is sufficient to have yourself examined once a year. However, if your condition worsens (increased cough, sputum and / or shortness of breath), you should contact your doctor immediately. In this way, deterioration and complications can be identified and treated in good time:
Infections and shortness of breath
Long-term COPD typically results in recurring bronchial infections and pneumonia. The decreased lung function can also lead to constant shortness of breath.
Cor pulmonale
In the late stages of COPD, the so-called cor pulmonale can occur: The right half of the heart enlarges and loses its functional strength - right heart weakness develops. Consequences of this are, among other things, retention of water in the legs (edema) and in the abdomen (ascites) as well as congested neck veins. Heart failure and respiratory muscle failure are serious, life-threatening complications.
Drumstick fingers and watch glass nails
So-called drumstick fingers with watch glass nails can appear on the hands. These are rounded fingernails with arched fingernails. They are the result of a reduced oxygen supply.
Pulmonary emphysema and barrel chest
As COPD progresses, lung tissue is destroyed and the lungs become over-inflated (pulmonary emphysema). Often this is expressed by a barrel chest. The rib cage is barrel-shaped and the front ribs are almost horizontal. The barrel chest is one of the typical symptoms of emphysema.
COPD Symptoms: Pink Puffer and Blue Bloater
According to the external appearance of the COPD sufferer, two types can be distinguished: the “pink buffer” and the “blue bloater”. These are two clinical extremes; in reality, mixed forms predominantly occur:
|
Type |
Appearance |
|
Pink buffer |
Pulmonary emphysema is in the foreground in the case of the "pink wheezer". The over-inflated lungs lead to constant shortness of breath, which overstrains the auxiliary breathing muscles. The affected person therefore consumes a lot of energy. The typical “pink buffer” is therefore underweight. Occasionally, dry cough occurs. The oxygen levels in the blood are not reduced because enough carbon dioxide is exhaled. The leading cause of death is failure of breathing. |
|
Blue bloater |
The "blue cough" (also called "bronchitis type") suffers mainly from cough and sputum, the COPD is in the foreground. He is usually overweight and cyanotic, so the lips and nails are discolored bluish due to lack of oxygen. Nevertheless, the shortness of breath is only slightly pronounced. The "blue bloater" has an increased risk of right heart failure. |
COPD symptoms of an exacerbation
In the course of COPD, the symptoms of COPD can worsen again and again - known as an exacerbation. The exacerbations can be divided into three degrees of severity: mild, moderate and severe. The COPD symptoms go beyond the normal daily fluctuation and usually last longer than 24 hours.
Responsible for an acute worsening of the COPD symptoms are, for example, viral and bacterial infections, air pollution (smog), damp and cold weather, accidents with injuries to the chest and drugs that negatively affect breathing.
Signs of worsening COPD symptoms include:
- Increase in breathlessness
- Increase in cough
- Increase in sputum
- Change in the color of the sputum (yellow-green sputum is a sign of a bacterial infection)
- general malaise with tiredness and possibly fever
- Chest tightness
Signs of a severe exacerbation are:
- Shortness of breath at rest
- decreased oxygen saturation in the lungs (central cyanosis)
- Use of the auxiliary respiratory muscles
- Water retention in the legs (edema)
- Clouding of consciousness up to coma
The symptoms of COPD are more pronounced in autumn and winter. Every acute exacerbation means a potential danger to life for the person concerned, since the lungs can fail within a short time with increasing oxygen deficiency and exhaustion of the respiratory muscles! Those affected with acute worsening of COPD symptoms should therefore urgently be examined by a doctor - they need more intensive treatment.
COPD stages
At the end of 2011, a new classification of COPD was presented by the GOLD (Global Initiative for Chronic Obstructive Lung Disease). Previously, only the impairment of lung function and the symptoms were decisive for the GOLD-COPD stages.
The GOLD classification from 2011 also took into account the frequency of a sudden worsening of COPD (exacerbation rate) and the result of patient questionnaires when classifying the stages.
In 2017, GOLD finally revised its recommendations again. Although the same parameters are still taken into account, the COPD stages are now more finely divided.
COPD stages: classification until 2011
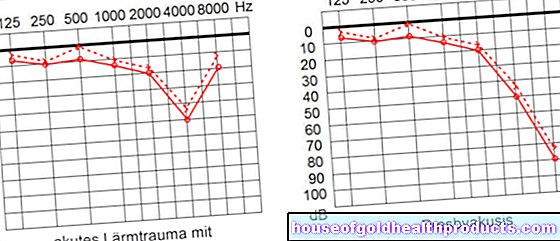
There are four stages of COPD in total. The classification is based on the lung function, which is measured with the help of the spirometer. The one-second capacity (FEV1) is determined. This is the largest possible lung volume that can be exhaled within a second.
|
Severity |
Symptoms |
One-second capacity (FEV1) |
|
COPD 0 |
chronic symptoms: |
noticeable |
|
COPD 1 |
with or without chronic symptoms: |
inconspicuous (not less than 80 percent |
|
COPD 2 |
with or without chronic symptoms: |
restricted |
|
COPD 3 |
with or without chronic symptoms: |
restricted |
|
COPD 4 |
chronically inadequate oxygen supply |
highly limited |
COPD 1
With a one-second capacity below 80 percent of the normal value, one speaks of mild COPD, i.e. COPD grade I. Typical symptoms are mostly chronic cough with increased mucus production. However, it is also possible that both symptoms do not appear. Difficulty breathing is usually not noticed yet. Often those affected do not even know that they have COPD.
COPD 2
COPD grade II is moderate COPD. Difficulty breathing can occur during intense physical exertion. The symptoms are usually more pronounced, but they can also be completely absent. The one-second capacity is between 50 and 80 percent of normal. Patients who do not do physical activity may not even notice the worsening of the disease.
COPD 3
At this stage of COPD, COPD is already severe and many alveoli are no longer functional. The one-second capacity in patients with COPD grade III is between 30 and 50 percent of the normal value. The symptoms of cough and sputum are more noticeable, and even with little exertion, those affected become breathless. But there are also patients who do not have a cough or sputum.
COPD 4
If the one-second capacity is below 30 percent of the normal value, the disease is already well advanced. The patient is in the end-stage of COPD, i.e. COPD grade IV. The oxygen content in the blood is very low, which is why patients suffer from shortness of breath even at rest. As a sign of the end of the COPD stage, damage to the right heart may have already developed (cor pulmonale).
COPD stages: classification from 2011
The classification of the COPD GOLD stages from 2011 was still based on lung function, measured using the one-second capacity. In addition, the GOLD now also took into account the frequency of exacerbations and symptoms recorded with the help of a questionnaire (COPD assessment test), such as shortness of breath or restricted exercise capacity. According to the new findings, there were four patient groups: A, B, C and D.
The measured one-second capacity initially roughly determined whether a patient was assigned to groups A / B (with COPD 1 or 2) or C / D (with COPD 3 or 4). The severity of the symptoms and the number of exacerbations then finally determined whether it was stage A or B or C or D.
Example: A patient with a one-second capacity between 50 and 80 percent of the normal value would correspond to a COPD stage GOLD 2 and would therefore be assigned to group A or B. If he had severe symptoms in the context of COPD, he would be assigned to group B, with only slight symptoms to group A. The same applies to groups C and D for one-second capacities of less than 50 percent (GOLD 3 and 4).
COPD stages: COPD assessment test
The COPD Assessment Test (CAT) is a questionnaire that helps you and your doctor to assess the influence of COPD on your quality of life. The test only takes a few minutes and consists of eight questions, for example whether you cough, have mucus or are restricted in your domestic activities. The extent to which the individual points apply is indicated with points between zero and five. Overall, a total number of points between 0 and 40 can be achieved. For the staging of COPD, it depends on whether the patient scores more or less than ten points.
Determination of the COPD stages since 2017
GOLD has been subdividing the COPD stages even more precisely since 2017. In contrast to the 2011 classification, the one-second capacity (still as GOLD stage 1 to 4) is now specified separately and in addition to groups A to D. This allows a more precise classification and thus a better adapted treatment.
Example: While according to the 2011 classification, a patient with a one-second capacity of less than 50 percent automatically belonged to groups C or D, this is not necessarily the case according to the new classification. If he has only minor complaints and at most one exacerbation per year, he can even belong to group A. However, the one-second capacity still plays an important role and is also specified. With a one-second capacity of 40 percent of the normal value (Gold 3), the sample patient would correspond to a COPD stage GOLD 3A according to the new classification.
As has been the case since 2011, the doctor determines the severity of the symptoms with the help of the CAT questionnaire.
The new COPD stages are designed to ensure that each patient receives the optimal treatment for them.
|
Staging according to FEV1 |
& |
Allocation to groups according to complaints and exacerbations | ||
|
1 2 3 4 |
A. |
B. |
≤1 exac./ year | |
|
C. |
D. |
≥ 2 exac. / Year | ||
|
CAT <10 |
CAT ≥ 10 | |||
FEV1 = one-second capacity in the lung function test
CAT = COPD assessment test (result in the questionnaire on the symptoms)
COPD: examinations and diagnosis
If you suspect COPD, your family doctor will usually first refer you to a pulmonologist (pulmonologist). Whether you actually suffer from the lung disease COPD or another disease can be found out with special examinations. Above all, the differentiation between COPD and asthma is very important because the symptoms are very similar.
COPD diagnosis: initial examinations
The doctor will first ask you about your medical history (anamnesis). It can provide initial indications of an existing COPD. Possible questions from the doctor are:
- Since when and how often have you been coughing?
- Are you coughing up more mucus, possibly especially in the morning? What color is the slime?
- Does stress such as climbing stairs cause breathlessness? Has this already occurred in peace?
- Do you smoke or have you smoked? If so, how long and how many cigarettes a day?
- What do you do for a living? Are you exposed to pollutants in the workplace?
- Has your performance decreased?
- Have you lost weight?
- Do you suffer from any other illnesses?
- Do you have symptoms such as water retention (edema) on your legs?
This is followed by a physical examination: If there is COPD, the doctor hears certain breathing noises such as wheezing when exhaling while listening to the lungs with a stethoscope. Often a weakened breathing sound can be heard, which is also referred to by medical professionals as "silent lung". This occurs when the lungs are over-inflated (pulmonary emphysema) because the patient is then no longer able to breathe out the tidal volume. Moist rattling noises can be heard when the lungs are congested. When the lungs are tapped, if the lungs are over-inflated, a hollow-sounding (hypersonic) knocking sound occurs.
In addition, the doctor looks for signs of reduced oxygen supply (for example blue lips or fingers = cyanosis) and heart failure (for example water retention in the ankle area).
What is the difference between COPD and asthma?
COPD and asthma are not easy to tell apart. Asthma is a chronic inflammatory disease of the airways caused by hypersensitivity or allergy. A certain trigger then leads to the narrowing of the airways, which manifests itself as shortness of breath. The narrowed airways can recede spontaneously or through treatment. Asthma is usually noticeable in childhood or early adulthood.
In COPD, on the other hand, the disease develops insidiously; it is also not an allergy. In contrast to asthma, this narrowing of the airways can only be partially, but not completely, improved by medication.
COPD diagnosis: apparatus-based examinations
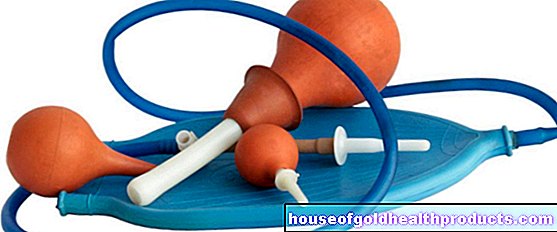
Various apparatus-based examination methods are used for a COPD test. Lung function tests (LuFu for short) such as spirometry, whole-body plethysmography and blood gas analysis are done to see how well the lungs are working. Pulmonary function tests are mainly used to diagnose COPD and to assess the course and therapy of the disease.
With spirometry, the patient breathes through the mouthpiece of the spirometer, which measures the tidal volume. The vital capacity and one-second air are measured, these are parameters for the lung function. The one-second capacity (FEV1) is the largest possible lung volume that can be forced out within one second. The vital capacity (FVC) is the total lung volume that can be forcefully exhaled after inhaling deeply. If the one-second capacity is less than 70 percent of normal, COPD is present.
Spirometry as a lung function test
In full-body body plethysmography, the patient sits in a closed cabin and breathes through a tube of the spirometer. The breathing resistance and the lung capacity are determined. With full-body body plethysmography, COPD can be differentiated from other diseases such as asthma.
An analysis of the blood gases shows the level of oxygen in the blood. Alpha-1-antitrypsin deficiency is specifically searched for in patients under 45 years of age with additional pulmonary emphysema. Professionals recommend doing this once in a lifetime test for every COPD patient. The determination can be carried out from a single drop of blood - similar to a blood sugar measurement. If it reveals the congenital deficiency, the diagnosis can be supplemented by a genetic test to detect the genetic change (mutation) on which the AAT deficiency is based.
Some lung and heart diseases cause symptoms similar to COPD. An X-ray examination, computed tomography (CT) and an EKG can therefore be carried out to confirm the diagnosis. X-rays and CT can detect pneumonia, pulmonary congestion, pneumothorax and tumors, for example. The EKG provides information about the heart function. There may be indications of increased lung pressure (pulmonary hypertension) and thus a right heart strain.
COPD: therapy
COPD therapy is a long-term therapy. It depends on the severity of the disease. Overall, COPD therapy includes drug and non-drug measures and has the following goals:
- Increase in physical resilience
- Symptom relief
- Prevention of acute deterioration (exacerbations)
- Improvement of the health status and quality of life of the person affected
- Avoid complications
COPD therapy
Most COPD patients are smokers. The most important component of COPD treatment is not using nicotine.
You should approach quitting smoking with medication and psychosocial support. You can get additional motivation by looking at the effects of COPD on smoking:
According to a scientific study, the lung function of COPD patients stabilizes when they stop smoking compared to patients who continue to smoke. In the first year, the lung function of the former smokers even increased again. The cough and sputum improved. Young smokers in particular benefited from quitting smoking. Patients who quit smoking also had a lower death rate.
However, these positive changes only occur if you completely renounce nicotine. For COPD therapy to be effective, it is not enough to simply smoke less than before.
COPD therapy: training
As part of COPD therapy, patients are recommended to take part in COPD training if possible. There they learn everything about the disease, its self-control as well as the correct inhalation technique and correct breathing, for example breathing with pursed lips (lip brake). In COPD training, patients also learn to recognize and treat an acute deterioration (exacerbation) in good time . It has even been proven that patient education in people with mild and moderate COPD improves the quality of life and reduces the number of exacerbations and thus the number of hospital stays per year. Such training courses are therefore important elements of COPD therapy and are offered by many health insurance companies.
COPD therapy: medication
Various groups of active ingredients are used as COPD drugs. They can alleviate symptoms and delay the progression of the disease through different mechanisms.
COPD therapy: bronchodilators
Bronchodilators are bronchodilator drugs that are very often used in COPD therapy. They reduce shortness of breath during exertion, reduce the number of exacerbations, help against inflammation and make the mucous membrane swell.
Doctors differentiate between short-acting and long-acting bronchodilators. Long-acting bronchodilators are superior to short-acting bronchodilators in COPD therapy, they are more effective and easier to use. They only need to be taken once or twice a day and are therefore well suited for regular needs.
Bronchodilators include anticholinergics, beta-2 sympathomimetics, and theophylline.
Anticholinergics: The best known representative is the short-acting ipratropium. It expands the bronchi, reduces mucus production, improves breathing and thus physical performance. The full effect occurs after 20 to 30 minutes.
The long-acting anticholinergic tiotropium bromide works for 24 hours. The active ingredient is therefore only taken once a day. It reduces lung hyperinflation, shortness of breath, exacerbations and hospital stays. Other long-acting anticholinergics are aclidinium bromide and glycopyrronium bromide.
Beta-2 sympathomimetics: Short-acting beta-2 sympathomimetics are used in acute respiratory distress. They work almost immediately. The substances used are called fenoterol, salbutamol and terbutaline.
Long-acting beta-2 sympathomimetics such as salmeterol and formoterol work for around twelve hours, indacaterol even around 24 hours. The active ingredients help against shortness of breath both during the day and at night. They also improve lung function, reduce lung hyperinflation, and decrease the number of exacerbations. This improves the quality of life for COPD patients. Cardiac arrhythmias can occur as side effects.
Theophylline: This active ingredient dilates the bronchi over the long term. It is only used in COPD treatment when a common drug combination such as anticholinergics plus beta-2 sympathomimetics is insufficient. The problem with taking it is that the level of the active ingredient can fluctuate, which greatly increases the risk of side effects. Doctors must therefore frequently check the amount of theophylline active substance in the blood (blood level). Because of the risks mentioned, theophylline is controversial and more of a reserve drug. It should only be used as a third choice in COPD therapy.
Combinations of bronchodilators: If the active ingredients mentioned do not work sufficiently when used individually, the inhalable slow-acting bronchodilators (such as tiotropium) and beta-2 sympathomimetics can be combined. This increases the bronchodilating effect. This can also be useful if, for example, the beta-2 sympathomimetic has excessive side effects such as palpitations and tremors. When combined with an anticholinergic, its dose can be reduced. This lowers the risk of side effects.
COPD therapy: cortisone
In addition to bronchodilators, cortisone (for inhalation) is also one of the active ingredients that are frequently used in COPD therapy. In long-term therapy, it prevents the inflammation of the airways and can thus prevent acute aggravations (exacerbations). Cortisone is used especially in patients who suffer from asthma in addition to COPD.
The use of inhaled cortisone is considered when the seconds capacity is less than 50 percent of normal and when additional steroids and / or antibiotics are used during exacerbations. The risk of side effects is low with this form of use.
Cortisone in tablet form is not recommended for long-term COPD therapy.
COPD therapy: mucolytics
Expectorant drugs (expectorants / mucolytics) are not generally recommended for COPD therapy. They are only used in the event of massive mucus build-up and acute infections. In this case, regular inhalation with saline solutions is also helpful. Bacterial infections usually also have to be treated with antibiotics.
COPD patients should also make sure they drink enough - but not excessively! This can namely put additional strain on the lungs and favor the derailment of a chronic front pulmonary.
COPD therapy: inhalation systems
Various inhalation systems are available for COPD therapy. In addition to metered dose aerosols and powder inhalers, nebulizers are also used.
Inhaling a drug has the advantage that the active ingredient can easily reach the diseased areas of the lungs. As a result, the patient can breathe easier because the active ingredients relax the smooth muscles in the walls of the bronchi and thus reduce the muscle tone in the bronchi. The lungs are then less over-inflated. Typical COPD symptoms such as shortness of breath, cough and sputum are relieved.
COPD therapy depending on the stage of the disease
The guideline of the German Respiratory League recommends that COPD therapy should be gradually adapted, depending on the stage of the disease. From stage to stage, more COPD medication must also be used.
First you start with short-acting bronchodilators, which are only used when necessary. If the symptoms increase, long-acting bronchodialators are used to supplement the therapy. Doctors only prescribe inhaled cortisone when the COPD progresses and the symptoms increase significantly. Basically, one tries to avoid cortisone preparations as long as possible. Long-term oxygen therapy is usually necessary in the end-stage of the disease. Surgical intervention (emphysema surgery) can also be considered.
COPD therapy: vaccinations
Since people with COPD often suffer from infections, vaccinations against flu and pneumococci are recommended - regardless of the severity of the disease. Vaccination has been shown to reduce mortality and should always be considered.
COPD therapy: exacerbations
Depending on the severity of the exacerbation and the impairment of the patient, COPD therapy is carried out on an outpatient or inpatient basis.
In some cases, it is enough if the drug dose is increased. If the symptoms such as cough, shortness of breath and sputum increase anyway, you must speak to your doctor. Other warning signs are fever and yellow-green sputum. They are indicators of an infection that should be treated with antibiotics. If there is no improvement, inpatient COPD therapy is necessary.
Patients with a severe exacerbation (severe shortness of breath, FEV1 <30 percent, rapid deterioration, old age) generally have to be treated as inpatients in a clinic.
COPD therapy: rehabilitation
COPD patients experience increasing breathlessness when they are exerted. That is why most of them move less and less. The consequences: The muscles break down, the load capacity is reduced, and those affected become increasingly inactive and ultimately more immobile. In addition, physical restraint reduces the quality of life and social contacts are avoided. This can cause depression and, as a result, further worsening of breathing.
Targeted physical training is therefore very important in COPD. It can prevent the breakdown of muscles and resilience. There are various rehabilitation programs for COPD therapy, such as lung exercise or breathing and physiotherapy.
COPD therapy: exercise
Physical training increases the quality of life and the patient's resilience. In addition, the number of exacerbations decreases. Physical training such as endurance and weight training should therefore be an integral part of long-term COPD therapy. Training programs of four to ten weeks, in which the patients complete three to five exercise units per week under supervision, show particularly positive effects. In a lung sport group, for example, you can learn specific exercises that strengthen the respiratory muscles and thus make breathing easier.
COPD therapy: respiratory and physiotherapy
Here, COPD patients learn how to make it easier to breathe more easily at rest and under stress with special breathing techniques and certain postures. You will learn how the chest becomes more flexible and stuck mucus can be coughed up better. This improves the ventilation of the lungs. At the same time, optimal breathing prevents the respiratory tract infections that COPD patients often suffer from. The relaxed abdominal muscles are also systematically trained. Correct breathing behavior is important because it takes away the fear of breathlessness, increases self-confidence and increases performance.
Well-known body positions that facilitate breathing are the so-called coachman's seat and the lip brake.
Coachman's seat: Support yourself with your arms on your thighs or on a table top so that your whole chest can support your exhalation. Close your eyes and breathe calmly and evenly. The driver's seat reduces increased airway resistance and supports the function of the auxiliary respiratory muscles. In addition, in this position the chest is relieved of the weight of the shoulder girdle.
Lip brake: Breathe out as slowly as possible against the pressure of your loosely closed lips. The cheeks puff out a little. With this technique, the airflow is slowed down and the bronchi remain open. The lip brake increases the pressure in the lungs and prevents the airways from collapsing when you exhale.
COPD therapy: long-term oxygen therapy
In the advanced stages of COPD, the oxygen supply from the damaged lungs is no longer sufficient. The patient therefore suffers from constant shortness of breath. Long-term oxygen therapy is then useful; The patient receives oxygen bottles from which he inhales oxygen through a nasogastric tube. In this way, the oxygen concentration in the blood stabilizes and the shortness of breath is reduced. If long-term oxygen therapy is used for 16 to 24 hours a day, the prognosis improves in patients with chronic dyspnea.
COPD Therapy: Diet and Weight
Weigh yourself regularly to check that your weight is stable. Many COPD patients show unwanted weight loss. This can be a sign of an unfavorable course of the disease. Sometimes targeted nutritional therapy is then necessary to put on a few pounds again. If breathlessness is the reason someone eats too little, smaller and more frequent meals are advisable.
On the other hand, it can also lead to sudden weight gain. It is usually an indication of heart failure (more precisely: right heart failure).The cardiac output is then no longer sufficient to ensure normal blood circulation. The blood builds up, causing water to pass from the vessels into the tissue and be stored there (edema). This can happen to the ankles, for example. Affected patients should limit their calorie intake to 1200 to 1500 kilocalories per day in order to lose weight successfully.
COPD Therapy: Aids
With advanced COPD, many patients can no longer cope with everyday life without outside help. In some cases, the independence can be maintained through aids. These include, for example, extensions for shoehorns and brushes as well as mobile walking aids (rollators).
COPD therapy: surgery
Surgery is considered in patients with advanced COPD who are increasingly suffering from hyperinflation and who are not helped by medication or rehabilitation. There are various surgical methods that can be used in COPD therapy:
Bullectomy
During a bullectomy, non-functional lung bladders are removed. The balloon-like enlarged bronchi (bullae) no longer participate in gas exchange and push away healthy neighboring lung tissue. If the bullae occupy more than a third of a lung, removing them can improve lung function and relieve breathlessness.
Before a bullectomy, a bronchoscopy, a series of pulmonary function tests, and computed tomography of the lungs are done.
Lung volume reduction
In the case of lung volume reduction, so-called lung valves are endoscopically inserted into the airways of the inflated lung sections. These valves close when you inhale and open when you exhale. This allows air to flow into the inflated areas and old air to escape again. This is said to reduce lung overinflation, relieve shortness of breath and improve lung function.
The lung volume reduction is only possible with a special form of emphysema (heterogeneous form). On the basis of preliminary examinations, it is determined whether this form of COPD therapy is suitable in individual cases or not.
Lung transplant
COPD is the most common reason for a lung transplant. On average, 60 COPD patients undergo a lung transplant each year. This operative measure of COPD therapy can extend life and improve the quality of life.
A lung transplant comes into question when all other COPD therapy measures (long-term oxygen therapy, home ventilation, etc.) have been exhausted and the life expectancy of the patient is significantly limited, according to the experts. Those affected have to wait around two years on average for a new lung.
Admission criteria to be placed on the waiting list for a lung transplant are, for example:
- abstinence from tobacco smoking for at least six months
- One-second capacity below 25 percent of normal
- Pulmonary hypertension
- Global respiratory failure (impaired gas exchange in the lungs, which reduces the oxygen partial pressure in the blood and increases the carbon dioxide partial pressure in the blood)
Exclusion criteria are too high a risk of complications in a lung transplant. Such is the case with:
- very overweight (BMI over 30 kg / m²)
- Coronary heart disease (CHD)
- Renal failure
- Cirrhosis of the liver
- Age over 60 years (in exceptional cases: 65 years)
COPD: disease course and prognosis
The prognosis of COPD depends on whether you can slow the progression of the lung disease. The most important element is to refrain from smoking. In COPD patients, this has a positive effect on symptoms, the course of the disease and life expectancy.
Non-obstructive bronchitis can often still be cured if you refrain from smoking or avoid exposure to harmful substances. The smoker's lung improves just a few hours after the last cigarette. The regeneration of the lungs is already visible after two weeks: the blood circulation has improved and the lung capacity has increased.
With a COPD lung, on the other hand, it is usually too late and lost lung tissue cannot be regained. In such cases, however, effective drug therapy can significantly reduce the symptoms. If a successful lung transplant is successful, COPD can be cured. However, the person affected then has to take medication that suppresses the body's immune system for a lifetime. Otherwise the new lung will be rejected.
COPD: prevention
To prevent the development of COPD, you should first and foremost quit smoking. Around 90 percent of all COPD patients have smoked for a long time or are still doing it.
The following tips also apply:
- In your free time as well as at work, make sure that you are not exposed to harmful influences such as dusty, cold or polluted air more than necessary. This also includes avoiding rooms polluted by tobacco smoke.
- Get vaccinated against influenza and pneumococci.
If you already have COPD, the following measures will help to avoid a COPD exacerbation (acute worsening):
- If you still smoke, give up. This significantly reduces the risk of exacerbations.
- Take part in a patient training course. There you will learn how to deal with the disease COPD and you will learn how to adjust your medication dose in the event of acute deterioration. This can reduce the number of hospital stays.
- Exercise regularly.
- Get vaccinated against influenza and pneumococci.
- Do breathing exercises (like the coachman's seat). It improves the breathing technique, the ventilation of the lungs and thus the oxygen supply. At the same time, optimal breathing prevents the respiratory tract infections that COPD patients suffer from.
- Have your back tapped (tapping massage). This promotes coughing up the mucus in smokers' lungs.
- Do not stay in smoke-filled rooms. Avoid places heavily contaminated with pollutants (dust, smoke).
- Contact the company doctor if there is a high level of pollution in the workplace. Let yourself be treated immediately!
- Watch your diet and weight. Every excess kilo puts a strain on the body. Conversely, being underweight also worsens the prognosis. In addition, a healthy diet supports the immune system.
- Also, support your immune system by avoiding harmful factors such as stress.
- Drink enough water and inhale with salt water regularly. This will help cough up the phlegm.
With these measures you can positively influence the course of COPD and your quality of life.
COPD: life expectancy
Life expectancy in COPD patients depends, among other things, on how much the airways are narrowed. In general, the tighter the constriction, the worse the prognosis.
In addition, there are a number of factors that influence patient life expectancy. For example, nicotine consumption, age and possible concomitant diseases play a role.
You can read everything you need to know about the life expectancy of COPD patients in the article COPD - Life Expectancy.
Tags: teenager sports fitness hospital