Hemangioma
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
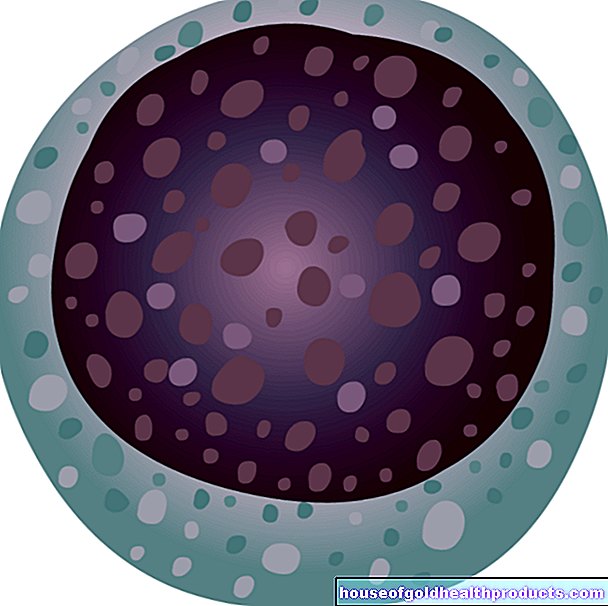
More about the experts All content is checked by medical journalists.The hemangioma (blood sponges, blood sponges) is a benign vascular tumor in newborns and infants. It shows up as a red patch of skin that can be raised. Such a hemangioma can appear anywhere on the body. In some cases it will go away on its own. Otherwise, various therapies can treat it. Read everything you need to know about hemangioma here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D18
Hemangioma: description
A hemangioma is a benign tumor of the blood vessels (angiodysplasia) that can lie at different depths in the skin. Colloquially it is also known as blood sponge or blood sponge. Hemangiomas do not metastasize, but their growth can press against organs and cause symptoms.
Hemangioma: types and frequency
A blood sponge occurs in infants and is either present from birth (congenital hemangioma) or occurs in the first few weeks of life (infantile hemangioma). The latter is more common than the congenital variant.
Girls are about three times more likely to have blood sponges than boys. About five percent of full term children and over 20 percent of premature babies have an infantile hemangioma.
A lymphangioma is similar to a hemangioma. The difference is that a lymphangioma arises from lymphatic vessels.
Hemangioma: symptoms
Hemangiomas are mostly found in the skin. Parents perceive them as red and blue dots, spots or knots on their baby. Blood sponges can be flat or raised. The infantile hemangioma develops in the first four weeks of life. It can then grow up to around 9 months of age.
Segmental hemangiomas can be found extensively in certain regions of the face or lower back. They often occur together with other malformations, for example brain hemangiomas or spine malformations (such as spina bifida = "open back").
Hemangioma: causes and risk factors
The exact mechanisms that lead to a blood sponge have not yet been conclusively clarified. However, hemangiomas occur more frequently in some families, which indicates an inheritable component in the development of the blood sponges.
If someone has more than ten blood sponges, it is called hemangiomatosis. Hemangiomas often occur in internal organs (e.g. in the liver, brain, lungs or gastrointestinal tract), so that further examinations are necessary. Genetic syndromes such as Kasabach-Merritt syndrome can also be associated with increased hemangiomas. In addition to the formation of large blood sponges on the extremities, there is a drop in the number of blood platelets (thrombocytopenia).
Hemangioma: examinations and diagnosis
If you notice a red spot on your child's skin, the pediatrician is the right contact. He asks you in detail about the medical history (anamnesis) of the child. He will ask you the following questions, among others:
- When did you first notice the skin change?
- Has the size or color changed since then?
- Does anyone in your family have or have had a hemangioma?
The doctor will then examine your child. He takes a close look at the red skin and also looks for changes in the rest of the skin. The doctor will also listen to your child's heart and lungs and check their movements. In this way, any associated malformations can be recognized.
Further investigations
The medical history and clinical examination are critical to making the diagnosis of hemangioma. Then the blood sponge should be photo-documented to determine changes over time.
In addition, further examinations are necessary in some cases. This includes an ultrasound examination (sonography).This can be used to detect hemangiomas in the abdomen, such as in the liver. Magnetic resonance imaging (MRI) can be used to diagnose hemangiomas in the brain.
Hemangioma: treatment
There are several ways to treat a hemangioma. When choosing the method, the most important thing is where the blood sponge is and how big it is. Rapid therapy is advisable if the tumor restricts the function of organs, for example eyes, ears, nose, mouth, feet or hands.
Some hemangiomas should also be treated early for cosmetic (on the face) or care reasons (in the genital area).
Cold and laser therapy
Small, flat hemangiomas up to a maximum of one centimeter in diameter are usually treated with cold therapy (cryotherapy). So the blood sponges are frozen. As a result, a blister or crust can form. Before treatment, the affected skin area should be numbed with a plaster with local anesthetic.
Laser therapy with a dye laser (FPDL) or pulsed flash lamp (IPL) can also be used for very small blood sponges. However, it has now receded into the background in favor of the effective drug treatment with propanolol.
Medication
If someone has a larger hemangioma or multiple blood sponges, drug treatment is often given, with the active ingredient propranolol. This is a beta blocker - a vasoconstricting drug that is usually used for cardiovascular disease. It has been officially approved for hemangioma therapy since 2014 because it was discovered by chance that it also works quite well against blood sponges.
Propranolol should be administered under inpatient supervision. The dose is initially very low and is then increased slowly to avoid cardiovascular disorders. In addition, the patient's heart must be examined using electrocardiography (EKG) and cardiac ultrasound (echocardiography) before starting therapy. So one wants to rule out that there is a heart disease that would speak against a therapy with propranolol.
In the past, blood sponges were also treated with glucocorticoids (cortisone) or chemotherapy drugs, but these are now considered out of date.
surgery
An operation is only indicated in the case of a hemangioma if, after the other therapies have been completed, remnants of the blood sponges remain or scars have formed. An operation should also be performed if the blood sponge could acutely restrict the function of an organ due to rapid growth (e.g. nasal breathing).
Additional measures
Infantile hemangiomas are accompanied by ulceration in the anus or genital region? Then - in addition to propanolol therapy - a care concept that dries out the lesion can be helpful: After every urination or bowel movement, the affected area is rinsed with disinfectant (octenidine dihydrochloride) and then left to air dry. Then you apply an antiseptic (polyhexanide) to the sore area and cover it sterile with a paraffin gauze bandage.
Dehydration can also be achieved with poultices made from black tea.
Hemangioma: disease course and prognosis
The prognosis is good. Infantile hemangiomas usually regress on their own between the ages of 1 and 9. Often no residues remain visible. If the blood sponges are particularly large, however, the following may remain:
- scar
- swelling
- Pigment change
- Skin thinning
A congenital hemangioma is more likely to persist than an infantile one. But with the right therapy, you can get rid of it completely.
Tags: pregnancy birth dental care digital health



.jpg)