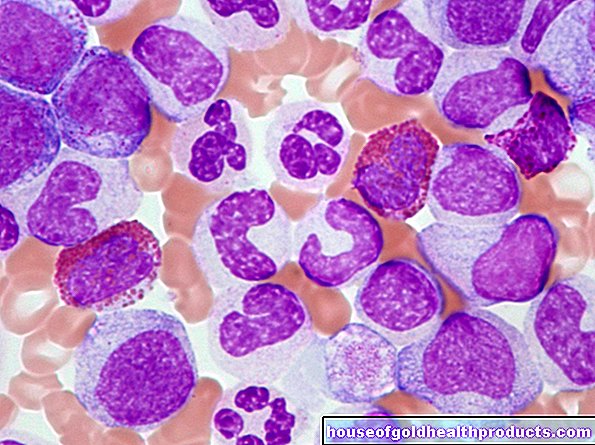
hemophilia
and Martina Feichter, medical editor and biologistDr. med. Fabian Sinowatz is a freelancer in the medical editorial team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Haemophilia (blood disease) is a blood clotting disorder that is usually inherited. The sufferers lack important blood coagulation factors or they are defective. As a result, hemophiliacs are prone to bleeding and bruise easily. The hemophilia cannot yet be cured. Thanks to modern therapies, however, hemophiliacs can lead a largely normal life. Read everything you need to know about hemophilia here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D66D67D68
Brief overview
- What is Hemophilia? A genetic blood clotting disorder (coagulopathy). It is also called hemophilia.
- Forms of haemophilia: The most common is haemophilia A, followed by haemophilia B. Other forms such as haemophilia C, von Willebrand-Jürgens syndrome and parahemophilia are less common.
- Cause: Deficiency or defect of coagulation factors (blood proteins that are necessary for the blood to clot). It is mostly inherited and rarely acquired (caused by a spontaneous gene mutation).
- Symptoms: increased tendency to bleed, which can easily lead to bleeding and bruising (hematomas). The bleeding also takes longer than normal. How severe the symptoms are depends on the severity of the haemophilia.
- Diagnostics: Measurement of various blood parameters (aPTT, Quick value, plasma thrombin time, bleeding time, number of blood platelets), determination of the activity of coagulation factors
- Treatment: replacement of the missing coagulation factor (in the form of factor concentrates); in certain cases other drugs (such as desmopressin for mild haemophilia A)
Hemophilia: description
Hemophilia is a congenital blood clotting disorder. Those affected (hemophiliacs, "hemophiliacs") are unable to form sufficiently functional coagulation factors. These are proteins in the blood that are necessary for the blood to clot. Due to the lack of coagulation factors, blood clots and wounds cannot easily form. Therefore, hemophilia patients are prone to bleeding. They also have wounds that bleed longer than normal. This can be dangerous under certain circumstances.
The medical term for a blood clotting disorder with an increased tendency to bleed is "hemorrhagic diathesis". The general name for a coagulation disorder is "coagulopathy".
Hemophilia: frequency
Hemophilia occurs almost exclusively in boys and men. It is relatively rare: only about two in 10,000 men have the hemophilia. There are around 10,000 people affected in Germany. Around 3,000 to 5,000 of them have a severe form of the disease.
Hemophilia: forms
There are different coagulation factors. Depending on which coagulation factor is affected in hemophilia, medical professionals differentiate between different forms of the disease.
Hemophilia A.
In hemophilia A there are problems with coagulation factor VIII (antihemophilic globulin A): Either the body cannot produce it in sufficient quantities or it is defective. About 85 percent of all hemophiliacs suffer from haemophilia A. Almost all of them are men.
Hemophilia B.
In hemophilia B, the coagulation factor IX (antihemophilic globulin B or Christmas factor) is missing. Here, too, the patients are mostly male. In the past, haemophilia B occurred more frequently in the English royal family and in the Russian tsarist family. That is why it is also called the "illness of kings".
Other forms of hemophilia
In addition to the main forms of hemophilia A and B, there are other hereditary coagulation disorders. One of them is the von Willebrand-Jürgens syndrome, also called von Willebrand syndrome (vWS). The focus here is on the von Willebrand factor: this coagulation factor is either too small or defective. As with hemophilia A and B, this leads to an increased tendency to bleed (hemorrhagic diathesis). In Germany, von Willebrand-Jürgens syndrome is found in up to one percent of the population. In contrast to the two main forms of hemophilia, this coagulation disorder affects men and women equally.
In rare cases, other coagulation disorders also occur, which are based on a lack of coagulation factors. They also have an increased tendency to bleed (hemorrhagic diathesis). These include:
- Haemophilia C: Deficiency of functional factor XI
- Parahemophilia: lack of functioning factor V
- Hypoproconvertinemia: Deficiency of functional factor VII
- Stuart Prower Factor Deficiency: Lack of working factor X
- Hageman Syndrome: Deficiency of Functioning Factor XII
- Fibrinase deficiency: deficiency in functional factor XIII
Hemophilia: symptoms
The symptoms of hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency) are the same - even if different coagulation factors are affected in each case. In general, one can say: the fewer functioning coagulation factors there are, the more pronounced the clinical picture.
Hemophilia: degrees of severity
The severity of the hemophilia depends on how much the activity of the coagulation factors is reduced compared to their function in healthy people. If the factor activity is only slightly reduced, those affected usually have no symptoms whatsoever. On the other hand, in symptomatic haemophiles, the factor activity is more reduced, which causes more pronounced signs. There are three degrees of severity of haemophilia (A and B):
Mild haemophilia:The factor activity is 6 to 45 percent of the normal activity of a healthy person; around 20 percent of all people with haemophilia have this severity. Those affected often do not notice much of their illness. This is why hemophilia is only discovered in many people in adolescence or adulthood, when operations or major injuries bleed longer than expected.
Moderate haemophilia: Factor activity is 1 to 5 percent of normal activity; about 20 percent of all haemophiles are also affected. The symptoms usually become obvious in the first few years of life with unusually long bleeding and frequent bruises. As with mild haemophilia, bleeding is usually the result of injuries or surgery. Spontaneous bleeding is rare.
Severe hemophilia: Factor activity is less than 1 percent of normal activity. This applies to about 55 percent of all hemophiliacs. The hemophilia is usually already noticeable at birth: removing the umbilical cord triggers massive bleeding. Heavy nosebleeds are not uncommon in infancy. In addition, even the smallest injuries or bumps can cause profuse bleeding under the skin (bruises). Internal bleeding is also more common, for example painful bleeding into the large joints (such as knees, elbows). Typically, many bleeds have no apparent cause (spontaneous bleeding).
Hemophilia: Risks and Dangers
Bleeding into the joints (hemarthrosis) often occurs repeatedly, especially in severe hemophilia. As a result, the affected joint can deform, wear out prematurely (osteoarthritis) and gradually stiffen. People with advanced hemarthosis can barely move their arms and legs and are dependent on a wheelchair.
Another danger with haemophilia is bleeding into the muscles: it can damage the muscle tissue and lead to muscle weakness.
In principle, internal bleeding in haemophilia can occur in any organ area. Bleeding in the brain is rare but dangerous: for example, it can impair the ability to think and impair concentration. Severe cerebral hemorrhage can even be fatal! Bleeding in the abdomen can also be life-threatening under certain circumstances. Heavy bleeding in the oropharynx can affect the airways.
In addition to bleeding tendencies (hemorrhagic diathesis), hemophilia of any degree of severity can also lead to wound healing disorders.
Von Willebrand-Juergens Syndrome: Symptoms
People with von Willebrand-Jürgens syndrome also have an increased tendency to bleed. Most of the time, there is light bleeding under the skin (bruises), bleeding gums or prolonged bleeding after surgery, for example after a tooth extraction. But there are also patients who suffer from heavy bleeding.
Hemophilia: treatment
Hemophilia therapy depends on the type and severity of the hemophilia. The attending physician will create a suitable therapy plan for each patient. In addition to drug treatment, he can also recommend general measures. For example, it can be advisable, especially in the case of severe haemophilia, to take physical care and avoid certain (injurious) sports.
Hemophilia A and B
Today, so-called factor concentrates are available for the treatment of hemophilia. These are concentrates of blood coagulation factors VIII (for hemophilia A) or IX (for hemophilia B) obtained from blood plasma or genetically engineered. You will have to be injected into a vein (intravenously). Many sufferers learn to inject the factor concentrate themselves. This gives them a lot of independence in dealing with the disease.
In the 1960s and 1970s, many people in Germany contracted hepatitis and / or HIV from contaminated factor preparations. This can practically no longer happen today: blood plasma is strictly controlled and pretreated before it is administered. And with genetically engineered factor concentrates there is generally no risk of infection.
In the case of mild and moderate haemophilia, the administration of factor concentrate is only necessary if necessary (on-demand treatment): The anticoagulant is administered, for example, in the case of heavier bleeding or before a planned operation. Minor injuries such as abrasions do not need to be treated with factor concentrate. The bleeding can usually be stopped by applying light pressure to the bleeding area.
People with severe haemophilia, on the other hand, have to inject themselves with factor concentrate regularly (long-term treatment). Factor VIII in haemophilia A is administered two to three times a week. Factor IX in haemophilia B generally only needs to be injected once or twice a week because of its longer retention time in the blood.
Surgeries and acute injuries
Before operations (even if a tooth extraction is planned), preparatory therapy must be carried out for all haemophilia patients. A factor concentrate is usually administered for this purpose. This is the only way to prevent serious complications from excessive blood loss during surgery.
In the case of mild haemophilia A, instead of factor concentrates, a drug that stabilizes blood clotting can be given before a planned operation. This includes desmopressin, for example. This is an artificially produced protein. It stimulates the release of stored factor VIII from blood vessels. The drug can only be used for a few days, otherwise the stores will soon be empty.
Tip: Before a planned procedure, people with haemophilia should discuss with their haematologist or haemophilia center which preventive therapy is advisable in their case.
In the case of acute injuries in an emergency, in addition to local hemostasis measures (e.g. pressure bandages), the administration of factor concentrate is also necessary.
Factor concentrate: complications
Some people form antibodies (inhibitors) against the coagulation factors in the factor concentrate. This so-called inhibitor hemophilia is significantly more common in people with hemophilia A than in people with hemophilia B. The inhibitors inactivate the added coagulation factor. The therapy is then not as effective as desired. Haemophilia B also threatens severe allergic reactions and other complications.
The amount of inhibitors in the blood is given in the so-called Bethesda unit (BE). The higher the BE value, the more inhibitors there are in the patient's blood.
In haemophilia A, a slight build-up of inhibitors can often be compensated for by increasing the dose of factor concentrate. If inhibitors are formed in large quantities, immune tolerance therapy is recommended: the patient receives very high doses of the missing coagulation factor in a complex therapy regimen. The immune system should gradually get used to its presence and stop the formation of inhibitors.
The rare inhibitor hemophilia in hemophilia B is treated differently. For example, those affected receive drugs that affect the immune system (immunomodulators).
Painkiller
Serious hemophilia can cause severe pain for those affected. For example, bleeding into the joints can be very painful. Then pain relievers like ibuprofen help. In contrast, the pain reliever acetylsalicylic acid (ASA) is unsuitable for haemophilia: it increases the tendency to bleed even further (side effect of ASA).
von Willebrand-Juergens Syndrome (VWS)
In von Willebrand-Jürgens syndrome, a distinction is made between different types, which are treated differently: In the so-called type 1, the active ingredient desmopressin is given when necessary (before an operation or in the event of acute bleeding). It stimulates the release of stored coagulation factors.
Desmopressin is also used in type 2; however, the drug does not always work here. Then the doctor prescribes a factor concentrate (with von Willebrand factor) instead.
Patients with VWS type 3 are always treated with a factor concentrate.
Hemophilia: causes and risk factors
Hemophilia is a congenital genetic disorder that is usually inherited. It occurs more rarely spontaneously (as a result of a spontaneous gene change = spontaneous mutation).
In hemophiliacs, the genetic information required to produce a functional coagulation factor is incorrect: in hemophilia A, it is coagulation factor VIII, in hemophilia B, factor IX. The result of the wrong construction plan is that the relevant coagulation factor cannot be produced in a sufficiently functional quantity. This disrupts blood clotting: wounds do not close as quickly, so bleeding takes an unusually long time. Some patients also have spontaneous bleeding (for no apparent cause).
Hemophilia A and B: inheritance
The blueprints (genes) for all parts of the body are on the chromosomes. In the nucleus of every cell in the body there are 46 chromosomes, including two sex chromosomes, which, among other things, determine gender. Women have two X sex chromosomes (XX): One X chromosome each was inherited from the mother and one from the father. Men, on the other hand, have a Y chromosome inherited from the father and an X chromosome inherited from the mother (XY).
The genes for the coagulation factors are on the X chromosome. In women who have two X chromosomes, if one of them contains a faulty blueprint for a coagulation factor, this can usually be compensated for by the other X chromosome. They are therefore largely symptom-free throughout their life.
If such a woman has a child, she passes one of the two X chromosomes on to the offspring. The probability that this is the copy with the faulty blueprint is 50 percent. By passing on the genetic defect, the mother becomes the carrier (carrier) of the hemophilia. If there is a son, he will be born a hemophiliac. A daughter, on the other hand, usually becomes a potential carrier in turn.
In rare cases, the relevant coagulation factor is not sufficiently formed even in female conductors. Wounds from injuries or operations can then bleed for a long time. It is even more rare for a girl to inherit a defective X chromosome from both parents. This is mostly in connection with the hereditary disease Turner syndrome. The affected girls show the full picture of hemophilia.
Von Willebrand-Juergens Syndrome
In the von Willebrand-Jürgens syndrome, the instructions for the von Willebrand factor (vWF) show a mutation: the coagulation factor is too small or is defective. The gene mutation can occur in both men and women.
Hemophilia: examinations and diagnosis
If someone has frequent spontaneous bleeding (such as nosebleeds) or bruises very easily, this could be an indication of haemophilia. This suspicion is particularly obvious if the family has already known cases of hemophilia. Those affected should have a doctor clarify the increased bleeding tendency. The first point of contact if you suspect haemophilia is your family doctor:
In a conversation with the patient, the doctor will first collect the patient's medical history (anamnesis): He has the symptoms described in detail, asks about any underlying diseases and whether there are any known cases of haemophilia in the family.
Laboratory tests are particularly important for clarifying a possible hemophilia. The doctor takes a blood sample from the patient in order to have it examined in the laboratory for various parameters: In hemophilia, the so-called aPTT (activated partial thromboplastin time) is longer than in healthy people. In contrast, the so-called Quick value (thromboplastin time, TPZ) and the plasma thrombin time (PTZ) are generally normal; they are only prolonged in severe haemophilia. The number of blood platelets (thrombocytes) and the so-called bleeding time are also normal in hemophilia A and B. In the von Willebrand-Jürgens syndrome, on the other hand, the bleeding time is prolonged. Bleeding time is the amount of time it takes for bleeding to stop.
In order to be able to determine unequivocally hemophilia A or B, the activity of the coagulation factors (VIII, IX) must be analyzed. A specialist in hematology or a specialized medical center (haemophilia center) is responsible for this.
Hemophilia: test in newborns and unborn babies
If a family has already developed haemophilia, the coagulation of male newborns is usually checked immediately after birth. In this way, hemophilia can be detected at an early stage. You can also check for haemophilia during pregnancy.
If a woman suspects that she has a genetic predisposition to haemophilia and is therefore a potential carrier, this can be clarified with a genetic test.
Hemophilia: disease course and prognosis
Hemophilia has not yet been cured. Patients have to cope with the lack of clotting factors throughout their lives. With the help of factor concentrates, however, they can usually lead a largely normal life.
If left untreated, moderate and severe hemophilia often lead to serious complications. For example, bleeding into the muscles can cause muscle damage. Hemorrhage in the joints can result in osteoarthritis and joint stiffening. Such complications can be avoided if hemophilia is detected early and treated consistently.
Tags: book tip smoking hair