Varicose veins
and Christiane Fux, medical editorDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.Varicose veins (varices) are extensions of the superficial veins. They are particularly common on the legs. The cause is a weak vein. They usually show up in the form of harmless, bluish curls under the skin. Women are more likely to suffer from varicose veins than men. Only in advanced stages do varicose veins cause symptoms such as water retention in the tissue (edema) and skin ulcers.Read here how varicose veins develop and how to treat them.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I86I83

Varicose veins: brief overview
- Causes: Pressure from blood congestion in the veins, risk factors are genetic predisposition, old age, obesity, smoking, female hormones
- Removal: Sclerotherapy, lasers, variceal surgery (stripping, CHIVA method, external valvuloplasty)
- Non-invasive treatment: compression stockings, alternate showers, exercise, medication / ointments with horse chestnut, butcher's broom or sweet clover
- Diagnosis: physical examination, duplex sonography, angiography
- Symptoms: visibly protruding veins under the skin, swollen, heavy legs, feeling of tension, itching, later "open legs"
- Forms: Truncal and lateral branch varices, perforating varices, reticular varices, spider veins, esophageal varices
Varicose veins: causes and risk factors
Varicose veins occur when blood builds up in the veins. The task of the veins is to transport the blood back to the heart against gravity. This work is done by the muscles surrounding the veins together with the elastic vessel wall. In addition, so-called venous valves in the vessels ensure that the blood does not flow back.
Varicose veins are common: every fifth adult has at least minor changes in the superficial veins. Women are three times as likely to be affected as men.
Congestion of blood in the veins
If the elasticity of the vessel walls decreases or the venous valves are damaged, the venous blood backs up. Then the vessel walls can stretch and sag - varicose veins develop. If there is insufficient movement or after a long day of standing, more blood collects in the leg veins. Then the patients often complain of heavy legs and feelings of tension.
Doctors differentiate between primary and secondary varices:
Primary varicose veins
The primary varices make up 70 percent of all varicose veins. They arise for no known cause. However, there are some risk factors that favor primary varicose veins:
- older age
- Obesity
- smoking
- hereditary factors
- female hormones
Inheritance
Connective tissue weakness can be inherited and increase the risk of varicose veins. However, other risk factors such as obesity, lack of exercise or gender have a greater influence.
Hormones
Women get varicose veins more often than men. The female sex hormones (estrogens) make the connective tissue more flexible. This is necessary during pregnancy. But it also promotes the development of varicose veins.
pregnancy
The risk of varicose veins is particularly high during pregnancy: every third pregnant woman gets varices. In most cases, they resolve on their own after the birth. Nevertheless, the risk of varicosis increases with the number of pregnancies.
Lack of exercise
Movement activates the muscle pumps. This makes it easier for the blood in the veins to flow towards the heart. When standing or sitting for long periods of time, the muscle pump slackens and the blood backs up more easily. If the veins in the hollow of the knee are also kinked while sitting, the venous return flow of the blood is additionally impeded. Sedentary work therefore promotes varicose veins.
Secondary varicose veins
The secondary varicose veins account for around 30 percent of all varicose veins. They arise when a flow obstruction forms in the veins. This usually happens after a blood clot in the deep veins of the leg (leg vein thrombosis).
Remove varicose veins
There are several ways to remove varicose veins. Which treatment path is best suited to the individual depends, among other things, on the type of varicose veins and the stage of the disease. The decision for or against surgical treatment of varicose veins depends on possible comorbidities and personal suffering.
What can be done against varicose veins?
More medical intervention is required to completely remove varicose veins. It is carried out by a doctor specializing in phlebology or vascular surgery. Most of the time, however, varices are harmless and do not need to be removed. However, some patients perceive them as a blemish and therefore decide to have an operation. However, this is only necessary when the affected veins have already sagged and no longer function properly.
The doctor will first examine the veins using an ultrasound scan or vascular x-ray (angiography) and then decide which procedure is most suitable for removing varicose veins in each individual case. For example, it is important to what extent the deep venous system is also affected or whether only the superficial veins are changed.
Remove varicose veins: obliteration (sclerotherapy)
Varicose veins are obliterated by causing an artificial inflammation of the vein walls. To do this, the doctor injects a sclerosing agent (for example Polidocanol) into the vein network, causing the vein walls to stick and scar. The sclerosing agent is administered as a liquid or as a foam, depending on the size and expansion of the vessels. Patients should then usually wear compression stockings for a few days.
Several sessions are usually necessary to successfully obliterate varicose veins. Because the tendency to develop varicose veins is inherited, varices often recur a few years later. The treatment must then be repeated if necessary.
Remove varicose veins: laser therapy
Varicose veins can also be removed with a laser. The procedure is usually carried out on an outpatient basis under local anesthesia. The doctor makes a small incision in the leg and inserts a fine laser probe into the affected varicose vein. This is usually done under ultrasound control so that it hits the right vessel. The laser heats the varicose veins, which then close. They scar and are then broken down by the body.
The removal of varicose veins by laser is particularly suitable for straight, not too pronounced varices. After laser removal, patients usually wear compression stockings for about four weeks to counteract the risk of swelling and the formation of blood clots.
Remove varicose veins: variceal surgery
Varicose vein surgery is a minimally invasive surgical procedure that usually leaves hardly any scars. Talk to the attending physician about the most suitable method for you and the respective surgical risks. Depending on the severity of the illness and the accompanying illnesses, varicose vein surgery is carried out in an inpatient or outpatient setting.
Remove varicose veins: partial stripping
When "pulling varicose veins", the doctor pushes a small probe into the affected vein and pierces the vein wall at the end of the varicose vein again. He then cuts through the vessel and pulls it out. With partial stripping, only the pathologically altered vessel sections are pulled.
Patients should then wear compression stockings for about four weeks to prevent swelling and blood clots from forming.
Remove varicose veins: CHIVA method
CHIVA is a French abbreviation and stands for "the blood flow correcting, vein-preserving, outpatient treatment of varicose veins". For this procedure, the doctor first examines the veins using ultrasound and ties off the pathologically altered vein sections during a minor surgical procedure. Then these usually regress on their own over time.
The patients should then wear compression stockings for four to five weeks in order to accelerate the regression. This method is not recommended for severe varicose veins.
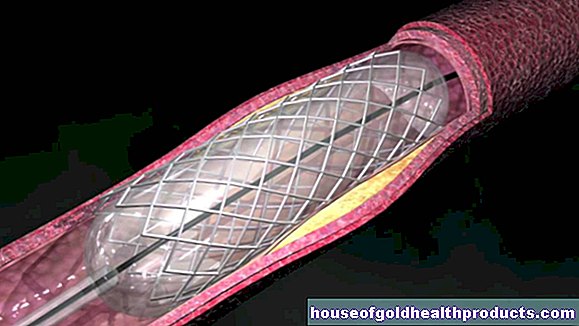
Removing varicose veins: external valvuloplasty (EVP)
External valvuloplasty (EVP) makes the venous valves functional again. The doctor constricts the large vena in the groin (great saphenous vein).
To do this, he makes a small incision in the skin under local anesthesia and sews a small polyester cuff around the large vein. This reduces the size of the vein. The reduced volume makes the venous valves functional again.
The procedure is suitable for very mild varicose veins and has the advantage that the diseased vein is preserved.
Removing varicose veins: surgical risks
Removing a varicose vein is usually just a minor surgical procedure. However, subsequent bleeding can occur. Lymph fluid can also build up and swell up the legs.
Therefore, after removing the varicose veins, the legs are bandaged or relieved with support stockings. In addition, if possible, patients should put their legs up to facilitate blood flow.
There is usually a tendency for varicose veins to persist even after surgical removal. Therefore, patients should consider the recommendations for the prevention of varicose veins.
Remove varicose veins: cost
The cost of removing varicose veins varies greatly depending on the treatment method and the severity of the condition. A spider vein operation is usually a cosmetic procedure that is not paid for by health insurance companies. In the case of larger varicose veins, on the other hand, the statutory and private health insurances usually cover the costs.
Varicose Veins: Non-Invasive Treatment
The aim of treating varicose veins is to improve the blood flow in the veins and thus counteract blood congestion. The surrounding tissue should be supported to prevent water retention in the tissue (edema). The better the venous blood flow, the lower the risk of possible circulatory disorders and ulcers or sore legs.
Compression stockings
The most important measure to support varicose veins are compression stockings. These are very tight, firm support stockings that compress the calf tissue. For varicose veins, they are often the first choice of therapy. The pressure of the stockings on the legs increases the muscle pump in the veins. The venous valves close better. The external pressure also counteracts the leakage of fluid from the veins into the surrounding tissue and prevents edema.
You should put on the stockings when you are lying down, as the blood quickly sinks into your legs when you are standing. Then the stockings no longer have the same effect.
The compression stockings should also fit exactly. Many patients also have them made to measure. They are divided into so-called compression classes (classes I to IV).
Depending on the location and extent of the varicose veins, the compression stockings extend to the calf, over the knee or even to the thigh. The compression stockings are available in different colors and should be replaced after about four to six months.
General measures
There are several ways to improve blood flow to the leg veins. This allows those affected to prevent further varicose veins.
Move
By doing simple exercises in everyday life you can improve the blood flow to your veins. Try to avoid standing and sitting for long periods of time. If possible, you should walk around regularly to get the blood flowing back into the veins.
Vein gymnastics
With a few simple exercises, you can get the blood flowing in your legs back up and running. Rock up and down on your tiptoes. Lie on your back and cycle in the air. Lie on your stomach, lift one outstretched leg and slowly and forcefully pull the tip of your foot forward several times. Then switch legs.
Elevate your legs
At night, you should raise your legs a little higher. This makes it easier to transport the blood towards the heart. Most patients report that raising the legs particularly improves the feeling of tension in the legs and has a significant relieving effect.
Avoid heat
If the heat is intense in summer, the symptoms of varicose veins increase. The leg veins then widen and can no longer adequately transport the blood to the heart. As a result, patients suffer from thick, swollen legs. You should therefore avoid extreme heat and also going to the sauna.
Alternating showers
Shower your legs alternately cold and hot every 30 seconds. When it is cold, the varicose veins contract, when the water is hot, the blood vessels expand again. This trains the blood vessels and stimulates blood circulation. Alternating showers can be practiced with every shower and often reduces swelling of the legs.
Medicines for varicose veins
So far there are no special drugs against varicose veins. However, numerous preparations are offered that are supposed to have a protective or soothing effect on the symptoms. Various medicinal plants such as horse chestnut, butcher's broom or sweet clover are said to have a vascular sealing effect (edema-protective).
Some sufferers rely on ointments based on plants or with the anticoagulant heparin. However, it is still controversial whether the active ingredients can really penetrate the skin and have an effect on the leg veins. However, many patients find massaging their legs very beneficial, which is why regular use of creams and ointments is recommended.
Varicose veins: examinations and diagnosis
The right contact for suspected varicose veins is a specialist in vascular surgery or phlebology. In an initial consultation, the doctor will ask you about current symptoms and any previous illnesses (anamnesis). He can ask you the following questions, for example:
- How old are they?
- Do you smoke, and if so, how much?
- Do you suffer from a feeling of tension in your legs in the evening?
- Lately, have you felt like your legs are very heavy in the evenings?
- For women: how many pregnancies have you had so far?
- Do other family members have varicose veins?
The doctor will then physically examine you for evidence of varicose veins. He will look at both legs and feet side by side in order to identify any swellings, skin discoloration or ulcers.
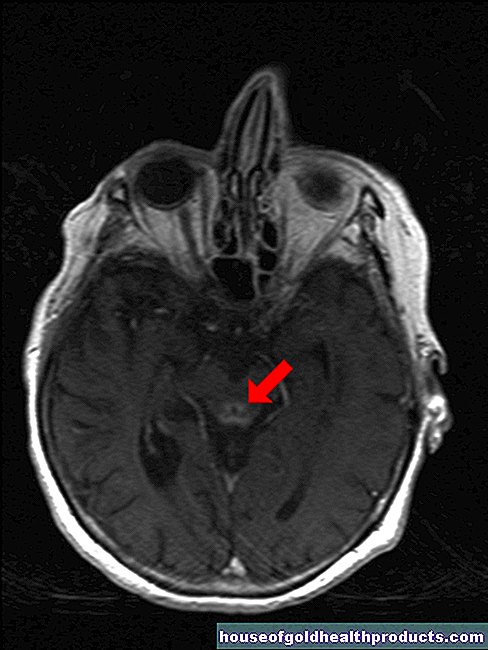
Ultrasound (duplex sonography)
A special ultrasound examination (duplex or Doppler sonography) enables a precise examination of the veins. Duplex sonography can depict the flow of blood and shows in which direction the venous blood is flowing. The doctor can also see how permeable the veins are and whether the venous valves are damaged or intact. Duplex sonography is a simple and inexpensive examination method that is considered the examination method of choice for varicose veins.
Angiography of the veins (venography)
If duplex sonography is insufficient or not available, the veins can also be visualized with a contrast medium (venography). If a thrombosis of the leg veins is suspected, venography can also provide diagnostic information.
To do this, the doctor punctures a vein in the groin or on the foot and introduces contrast medium. The contrast medium makes the veins visible in the X-ray. A break in the course of the contrast medium on the X-ray image thus indicates a vascular occlusion.
Varicose veins: Different shapes
Varicose veins (varices, varicose veins, varicose veins) are cylindrical bulges or widenings of superficial veins. The blood vessels form tangles and coils, which often shimmer bluish through the skin.
Varicose veins: legs
Depending on the location and shape, a distinction is made between different forms of varicose veins on the legs.
Truncal and lateral branch varices,
These are varicose veins of the medium and large veins. This type of varicosis is the most common and mostly occurs on the inside of the thighs and lower legs.
Perforating varices
The superficial veins are connected to the deep leg veins by connecting circuits. When these connecting veins expand and sag, one speaks of perforating varices.
Reticular varices
Very small varicose veins of the legs are called reticular varices. The diameter of these small veins is a maximum of two to four millimeters. Reticular varices are found mainly on the outside of the thighs and lower legs and in the hollow of the knee.
Spider veins
Spider veins are thin, web-like varicose veins. They rarely cause discomfort. However, some sufferers perceive them as annoying blemishes. Spider veins are easy and uncomplicated to desolate. Usually several sessions are necessary. Since it is a cosmetic problem, those affected pay for it themselves.
You can find more information on the subject in the article Spider veins.
Varicose veins: esophagus (esophageal varices)
Varicose veins of the esophagus (esophageal varices) are significantly less common than varicose veins of the legs. The wall of the esophageal veins becomes increasingly thinner over time. The esophageal varices can therefore bleed more easily and cause life-threatening complications.
A varicosis of the esophagus is usually caused by damage to the liver circulation when the liver becomes scarred (cirrhosis of the liver). The blood backs up in the great circulation. The bypass circuits in the esophagus, the abdominal wall or the rectum increasingly fill with blood. The pressure creates bulges in the veins, i.e. varicose veins.
Varicose veins: symptoms
In the early stages, varicose veins usually do not cause any discomfort. The very fine spider vein varices in particular are usually harmless. They usually show up as harmless red, blue or purple veins in the skin of the legs and rarely cause pain.
Stages of varicose veins
Depending on the severity of the symptoms, the varicose veins are divided into different stages:
Initial stage (stage I)
At the beginning of the disease, varicose veins usually do not cause any symptoms and are more of an aesthetic problem. However, many sufferers perceive the spider veins or varicose veins as unsightly and avoid showing them.
Heavy legs (stage II)
In the further course, patients with varicose veins on the legs often suffer from the feeling of heavy legs and feelings of tension. Your legs get tired faster. Calf cramps are more common at night. These symptoms usually improve when lying down and when moving, as the blood flow in the veins is stimulated. Some patients also report pronounced itching or that the symptoms worsen in warm temperatures. When it is warm, the veins widen, the blood can drain even more poorly and the symptoms worsen.
Water retention (edema) in the legs (stage III)
The longer the blood congestion in the veins, the more stressed and permeable the vessel walls become. Fluid, proteins and blood breakdown products (hemosiderin) are then pressed out of the varicose veins into the surrounding tissue.
Initially, patients only suffer from water retention (edema) in their feet and legs in the evening. The chronic congestion of the blood also causes reddish, itchy skin changes (congestive dermatitis, congestive eczema). In older patients in particular, the skin thins out over time ("parchment skin"), and injuries occur more easily, but these can still heal.
Open leg ulcers (stage IV)
If the blood congestion persists, the surrounding tissue is no longer adequately supplied with oxygen. Small injuries can then no longer heal properly. Ulcers form on the skin and the tissue dies. This is how the so-called "open legs" (ulcus cruris) arise.
The reduced blood flow allows only a very slow wound healing. The open ulcers must therefore be treated continuously by a doctor in order to prevent the spread of bacteria.
Inflammation of the veins (phlebitis)
Patients with varicose veins are more likely to suffer from additional inflammation of the superficial veins (phlebitis). The chronic congestion of blood increasingly strains the vessel walls, and they easily become inflamed.
A blood clot easily forms in the affected area, which can block the blood vessel. A thrombosis develops. Such a blood clot can also loosen and be washed into the pulmonary circulation via the large bloodstream. Here it can clog a vessel in the lungs and cause a pulmonary embolism. This is an emergency that requires immediate medical attention to prevent life-threatening complications.
Varicose veins: prevention
Since the genetic predisposition to varicose veins persists for a lifetime, those affected should take appropriate preventive measures. This also applies after the varicose veins have been removed in order to prevent them from re-forming:
- Get regular exercise and exercise. Endurance sports such as cycling, running or swimming are particularly suitable for strengthening the calf muscles and preventing varicose veins.
- Regular alternating showers and Kneipp baths also stimulate blood circulation and can counteract varicose veins.
- Eat a healthy diet and watch your weight. Obesity can impair the venous blood flow and promote varicose veins.
- Put your legs up frequently. The blood then does not have to flow out against gravity, and the feeling of "heavy legs" decreases.
- Avoid intense heat and long periods of standing or sitting, as both encourage and aggravate blood congestion and varicose veins.
- Although these measures cannot remove varicose veins, they can prevent (re) formation.