Osler's disease
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.Osler's disease is a rare hereditary disease in which abnormally dilated blood vessels develop in various parts of the body. These vessels are easily vulnerable, which is why bleeding occurs frequently, for example in the form of nosebleeds. A cure is not yet possible. However, various symptomatic treatment options enable most people to lead a largely normal life. Here you can read everything you need to know about Osler's disease.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I78

Osler's disease: description
Osler's disease (Rendu-Osler-Weber syndrome) was named after its discoverer and is also known as hereditary hemorrhagic telangiectasia (HHT). This term already conceals the essential characteristics of this disease:
“Hereditary” means that it is an inherited disease. The term “hemorrhagic” is derived from the Greek “haima” (blood) and “rhegnynai” (flow) and describes the bleeding that occurs in Osler's disease, such as nosebleeds, coughing up blood or gastrointestinal bleeding. The word “telangiectasia” also comes from the Greek: “telos” (wide), “angeion” (vessel) and “ektasis” (expansion). This describes the red, punctiform skin symptoms that are particularly visible on the face. These are pathological enlargements of the smallest blood vessels (capillaries).
There are no reliable data on the incidence of Osler's disease. The Deutsches Ärzteblatt describes that one in 10,000 people is affected by this disease. Overall, this is a rare disease. However, Osler's disease is more common in France, Denmark and Japan.
Osler's disease: symptoms
The symptoms of Osler's disease can be very different. The first symptom is usually heavy and regularly recurring nosebleeds. It usually occurs before the age of 20. Only later do the typical punctiform vasodilatations (telangiectasias) appear on the face, fingers and other parts of the body.
In addition, Osler's disease affects the liver in 80 percent of patients, the gastrointestinal tract in 44 percent, the lungs in 33 percent and the brain in up to 15 percent. In most cases, short-circuit connections develop between arteries and veins. As a result, the blood drains from the arteries (high pressure) into the veins (low pressure), filling the veins excessively with blood. The veins are overloaded by the increased blood flow and blood congestion forms in the veins. Depending on the organ affected, this venous congestion can have different consequences.
Nosebleeds
Epistaxis is the typical symptom of Osler's disease: in up to 90 percent of patients, spontaneous, heavy and often recurring nosebleeds occur in the course of the disease. There is no specific trigger such as an accident or a fall. Most of the time, the nosebleed is one of the first symptoms of the disease, which usually occurs up to the age of 20. In rare cases, it manifests itself afterwards as well.
Telangiectasia
This is understood to mean expanded capillaries. In Osler's disease, telangiectasias appear as small, reddish, point-like spots on the skin. Since Osler's disease is a systemic disease, it can in principle occur anywhere on the body. Particularly common locations are the face area (cheeks, lips, tongue, nose or ears) and the fingers (here especially on the fingertips).
liver
The liver is also affected in about 80 percent of Osler's disease patients. There are short-circuit connections between arteries and veins (shunts). In the vast majority of cases, these vascular changes do not lead to symptoms. In rare cases, however, heart failure, high blood pressure in the hepatic vein or biliary congestion can develop. The blood can back up in the lungs (shortness of breath), liver (with symptoms of hepatic venous hypertension) or the legs (swollen legs, edema).
High pressure in the liver vein in Osler's disease can bypass blood vessels and lead to bleeding (vomiting of blood). In addition, ascites can form and the detoxification function of the liver can be impaired. It is also possible that the coagulation factors formed in the liver are only produced to a limited extent, which means that bleeding can occur more easily. A bile blockage can be noticed when the skin and the whites of the eyes turn yellow. The skin often itches uncomfortably. The stool may be discolored and the urine may appear brownish.
Gastrointestinal tract
Telangiectasias can also be found in the gastrointestinal tract in Osler's disease. They usually develop with age and can cause gastrointestinal bleeding. This can cause black discoloration (tarry stool) or blood on the stool. Repeated heavy bleeding can cause anemia.
lung
Short-circuit connections between the arterial and venous blood vessel systems in the lungs are usually larger and are known as pulmonary arteriovenous malformations (PAVM). They occur in about a third of people with Osler's disease and can lead to coughing up blood.
In addition, there is an increased risk of so-called paradoxical embolism with Osler's disease. As a rule, thromboses (blood clots) form in the veins. If they loosen and are swept along in the bloodstream as an embolus, they normally only reach the pulmonary vessels via the right heart, where they can block the pulmonary vessels (pulmonary embolism). However, the embolus does not get further into the left heart and thus also not into the arterial vessels. Organs that receive arterial blood from the left heart are therefore usually unaffected by such emboli.
Central nervesystem
Symptoms of the central nervous system in Osler's disease mostly arise from short-circuit connections in the lungs. Material carried away from the pulmonary veins can lead to bacterial accumulations of pus or a stroke. However, in Osler's disease there can also be direct short-circuit connections between arteries and veins in the brain. They mostly lead to headaches, seizures, and bleeding.
Osler's disease: causes and risk factors
Osler's disease is caused by a genetic change that can be inherited regardless of gender. This means: If one parent suffers from Osler's disease, there is a 50 percent chance that the child also has the genetic predisposition for Osler's disease. A gene carrier does not always have all the symptoms of the disease (incomplete penetrance).
Osler's disease: examinations and diagnosis
If a patient suffers from symptoms of Osler's disease, the doctor must check the so-called Curaḉao criteria. There are four typical criteria for Osler's disease. In order for a reliable diagnosis of Osler's disease to be made, at least three of these criteria must be met. If only two of the criteria are positive, this only suggests the suspicion of the disease, so that further investigations are necessary. If only one criterion applies, there is most likely no Osler's disease.
1) nosebleeds
With Osler's disease, those affected suffer from recurrent nosebleeds that occur without a specific trigger (such as a fall).
2) telangiectasia
The doctor checks whether the lips, the oral cavity, the nose and the fingers show red, punctiform vascular enlargements. The characteristic of telangiectasias in Osler's disease is that they disappear when you press on them with a transparent object (e.g. a glass spatula).
3) Involvement of the internal organs
Various tests may be necessary to find out whether internal organs such as the lungs, liver or gastrointestinal tract are also affected: If the doctor reports anemia caused by obvious or unnoticed blood loss (e.g. bleeding from the intestine) suspected of having Osler's disease, he draws blood. This is used to determine the level of hemoglobin (Hb) in the blood, which is too low in anemia. In order to detect vasodilatation in the gastrointestinal tract, a gastric and colonoscopy is necessary. The doctor can determine vascular changes in the liver with an ultrasound (sonography). Changes in the lungs or brain can be shown on a computerized (CT) or magnetic resonance imaging (MRI) scan. In order to be able to see the vessels better, some contrast medium is injected into a vein before the examination.
4) Relationship with Osler's disease
If another first-degree related family member (mother, father, siblings, children) has the disease, this criterion is met.
Although the diagnosis of Osler's disease is mainly made using the Curaḉao criteria, nowadays a genetic diagnosis can also be made from a blood sample. It is mainly carried out in people with a more severe disease with lung involvement or if there is a typical genetic change in affected family members.
Osler's disease: treatment
The two main problems with Osler's disease are, on the one hand, the pathologically enlarged vessels from which it can bleed regularly. On the other hand, short-circuit connections (anastomoses) in internal organs can damage the organ function of the affected organs (especially the lungs and liver) and lead to severe bleeding. The goals of treatment therefore primarily include the obliteration of potential sources of bleeding (especially the nose) and, if necessary, the elimination of vascular short circuits (for example in the lungs) with surgical techniques. Various drugs complement these measures.
Treatment of nosebleeds
Frequent nosebleeds are particularly stressful for those affected. Osler's disease is treated with the following measures:
Nasal ointments and nasal packing
Nasal ointments can be used to prevent the frequent nosebleeds associated with Osler's disease. They moisturize the lining of the nose, reducing the risk of it tearing and bleeding. In the case of acute, heavy bleeding, a nasal packing may be necessary. A tamponade is a filler that is stuffed into the nostril to stop the bleeding. It can be made of different materials, but it should be easy to detach from the nasal mucosa. Tamponades specially developed for nosebleeds are available in pharmacies.
Coagulation
If the nosebleed cannot be adequately treated with ointments and tamponades, dilated blood vessels in the nose can be obliterated with a laser or electrical procedure. However, this can injure the nasal septum, which in turn can lead to heavy bleeding.
Skin graft
If the nasal wall is almost completely permeated with the vasodilatations typical of Osler's disease, a skin graft can be carried out. First, the nasal mucosa is removed and then replaced with skin from the thigh or with oral mucosa. With this procedure, the nosebleed disappears relatively reliably. However, a dry nose with crusts and crusts and a loss of smell can occur.
Operative nasal closure
If the symptoms are extremely pronounced, the nose can be completely closed surgically. This prevents nosebleeds from occurring. However, those affected have to breathe through their mouths for the rest of their lives. This procedure is mainly suitable for people with Osler's disease who have to take blood-thinning medication and who can hardly stop a nosebleed.
Medication
If patients with Osler's disease suffer from recurrent nosebleeds, drug therapy can also be useful. For example, the active ingredient tranexamic acid, which is taken orally in the form of tablets, comes into consideration. Tranexamic acid prevents the blood clots that form when the blood clots from being dissolved again.
Treatment of liver symptoms
Liver involvement in Osler's disease should be treated with medication for as long as possible in order to avoid surgical interventions due to the high risk of bleeding. For example, beta blockers can lower an existing high blood pressure in the portal vein. Further therapy options depend on the individual complaints. Endoscopic closure of the altered hepatic vessels or, in extreme cases, a liver transplant are associated with high risks and should therefore not be done in Osler's disease.
Treatment of gastrointestinal tract symptoms
If telangiectasias in the gastrointestinal region lead to anemia (anemia), iron should be replaced with a capsule preparation or an infusion. In rare cases, blood transfusions are necessary to treat anemia. If enlarged or bleeding vessels are found during a colonoscopy, they can be obliterated during the colonoscopy. There is also evidence that therapy with female sex hormones (estrogens and gestagens) improves hemostasis in the gastrointestinal tract. These hormones stimulate the formation of clotting factors in the liver, which are responsible for blood clotting. If more of the coagulation factors circulate in the blood, this improves the body's own hemostasis. However, this therapy option is only possible for Osler's disease patients from the menopause.
Treatment of pulmonary symptoms
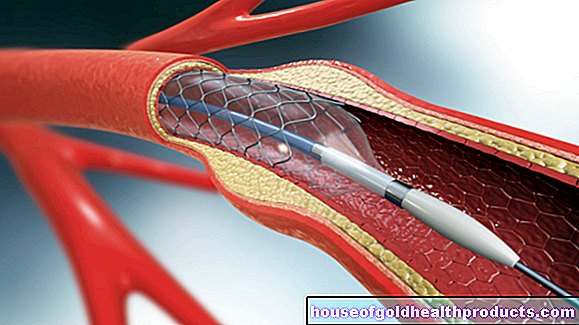
If there are pronounced vascular short-circuits (anastomoses) in the lungs in Osler's disease, these can be closed as part of a catheter examination. To do this, the femoral artery is sought in the groin. With a small tube (catheter), the doctor can then penetrate the vascular system to the corresponding vascular change. This is closed by a small wire spiral or a balloon. This does not affect the blood supply to the lungs.
Treatment of central nervous system symptoms
If blood vessels in the brain are abnormally changed, they can be treated with neurosurgical measures. Possible treatment options should be made together with neurologists (neurologists), neurosurgeons and radiologists and are always individual.
Osler's disease: disease course and prognosis
Since Osler's disease is a genetic disease, a cure in the narrower sense is not possible. However, the symptomatic treatment measures presented enable most people who suffer from Osler's disease to lead a largely normal life. Patients with known short-circuit connections in the lungs should only refrain from diving with compressed air cylinders, as life-threatening air embolisms can occur more frequently.
With regular medical check-ups, possible complications involving the internal organs can usually be quickly identified and treated before they cause symptoms. Pulmonary arterial venous malformations can enlarge with age and during pregnancy and cause serious bleeding problems.
Overall, the course of the disease and prognosis are not the same in all Osler's disease patients. The spectrum of possible complaints ranges from only slight restrictions to life-threatening complications as a result of Osler's disease.
Tags: first aid nourishment medicinal herbal home remedies






.jpg)







.jpg)