PML (progressive multifocal leukoencephalopathy)
Maximilian Reindl studied chemistry and biochemistry at the LMU in Munich and has been a member of the editorial team since December 2020. He will familiarize himself with medical, scientific and health policy topics for you in order to make them understandable and comprehensible.
More posts by Maximilian Reindl All content is checked by medical journalists.Progressive multifocal leukoencephalopathy (PML) is a serious disease of the central nervous system. It is the result of infection with the JC virus. PML usually breaks out in persistently severely immunocompromised patients - for example in the context of AIDS or due to certain medications. The course of the disease is usually critical. Here you can find out what is known about progressive PML and which treatment approaches are available to doctors.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A81

Brief overview
- What is progressive multifocal leukoencephalopathy? Serious central nervous system disease; caused by the John Cunningham virus (JC virus, JCV). PML is difficult in many cases.
- Causes: The JC virus damages certain cells in the white matter of the brain (demyelination). JCV is usually the result of a severely immunocompromising disease (especially HIV / AIDS) or treatment with drugs that slow down the immune system - for example in the case of an organ transplant, multiple sclerosis or the like.
- Frequency: Rare disease, frequency depends on the cause; Risk generally increases with persistently weakened or suppressed immune systems.
- Symptoms: changes in character, visual disturbances, progressive paralysis, visual field deficits, epileptic seizures, incontinence, impaired movement coordination, speech disorder, swallowing disorder, dementia.
- Diagnosis: nuclear spin (MRT), examination of the nerve water, JCV detection (PCR or antibodies)
- Treatment: Currently no causal treatment; AIDS-related PML is treated with antiretroviral drugs (so-called HAART therapy) to stabilize the immune system; if necessary, discontinuation of immunosuppressive therapy, if necessary additional blood washing treatment (immunoadsorption, plasmapheresis); an experimental treatment with virus-specific T cells seems promising (adoptive immunotherapy).
- Prognosis: Depending on the cause; in HIV / AIDS often progressing rapidly and, if left untreated, fatal within about six months; after the illness has been overcome, neurological damage can remain
What is progressive multifocal leukoencephalopathy?
Progressive multifocal leukoencephalopathy, or PML for short, is a serious disease of the central nervous system. PML is caused by the John Cunningham virus (JC virus, JCV), which belongs to the group of the widespread polyomaviruses. While it is generally harmless for healthy people, it can spread in severely weakened people (e.g. in patients with advanced HIV infection).
The JC viruses particularly attack specialized brain cells (oligodendrocytes). As a result, nerve cords lose their “covering”, the so-called myelin sheaths. This significantly affects the transmission of nerve signals. As a result, depending on the affected brain region, nerve functions fail, such as the control of certain muscles.
Frequency of PML
Overall, PML is a rare disease. The frequency within individual patient groups depends on the cause. In AIDS, the result of untreated or undetected HIV infection, around three to seven percent of patients develop PML.
On the basis of immune-suppressing therapy, the risk of PML increases with the duration of the therapy. The multiple sclerosis drug natalizumab should be mentioned in particular. In about 4 out of 1000 treatments, PML develops.
What causes progressive multifocal leukoencephalopathy?
The cause of PML are active JC viruses that multiply in the tissue of the brain and attack certain nerve cells there. This usually only happens in people with a pronounced immune deficiency.
What is the JC virus?
The John Cunningham virus, a polyomavirus, is a so-called opportunistic pathogen: it is generally harmless to healthy people because the immune system can act against it. An initial infection is usually symptom-free.
However, the JC virus then remains in the body. Experts assume that parts of the bone marrow and certain nerve cells, presumably also in the kidneys, are dormant for a long time before the onset of PML. However, JCV can be (re-) activated, multiply and spread through immune-suppressing therapy (immunosuppression) or certain immune deficiencies.
Infection with the JC virus
Experts estimate that around 40-70 percent of the adult population carry the PML-causing JC virus (the information in the literature varies considerably). Infection with JCV probably occurs in childhood and adolescence via droplet infection or smear infection. In rare cases, an organ transplant can transmit the JC virus.
How does the PML arise?
If the JC viruses can spread due to a weakened immune system, they preferentially attack certain cells in the brain, the so-called oligodendrocytes.
These supply, support and protect the actual conduction pathways of the nerve cells, the axons. To do this, they form so-called myelin sheaths (myelin sheaths). These wrap around the axons and act as electrical insulation to enable the nerve signals to be transmitted properly.
If the oligodendrocytes perish as a result of the JCV infection, the nerve impulses consequently no longer reach their destination. As a result, there are severe limitations in motor and cognitive abilities.
HIV infection risk factor
The majority of PML patients suffer from an advanced HIV infection. This is usually the case when the infection goes undetected or is not treated.
Since the HIV virus specifically attacks specialized immune cells (T cells / T helper cells / CD4 + cells), the immune system as a whole decreases its ability to defend itself. This also creates a “gap” in the pathogen defense system in the central nervous system.
If the infection progresses, the immune system is so weakened over time that certain diseases - such as PML - can break out. Then doctors speak of an HIV infection in stage 3 or AIDS. The progressive multifocal leukoencephalopathy is thus also one of the AIDS-defining diseases.
Further information on the background, course and treatment of HIV infection and the disease AIDS can be found here.
Risk from further illnesses
Much less often than an advanced HIV infection or AIDS, other diseases can promote PML. The basis is also a pronounced defensive weakness. These include malignant diseases of the hematopoietic and lymphatic system such as blood cancer (leukemia) or lymph gland cancer. The therapy used also plays a role here.
Risk factor medication
There are a number of drugs that influence the immune system and thus impair or suppress specific defense reactions (immunosuppression).
This effect is sometimes desirable - for example in autoimmune diseases in which the immune system is directed against the body's own cells, or after organ transplants. With other preparations, the immune system weakness is a relevant side effect. This is the case with anticancer drugs, for example.
In particular, if this type of immunosuppression persists, the risk of the JC virus spreading and causing PML increases. Drugs that medical professionals point out to be associated with PML include:
- Rituximab: a therapeutic antibody that is used, for example, in rheumatoid arthritis or against malignant lymphoma (lymph gland cancer)
- Brentuximab vedotin: an antibody that doctors use against certain forms of lymphatic cancer, for example
- Mycophenolate mofetil: a drug used to prevent the organ from being rejected after an organ transplant
Above all, however, it includes preparations for the treatment of multiple sclerosis.
Special case of multiple sclerosis therapy
In the clinical picture of multiple sclerosis (MS), the usually useful white blood cells (leukocytes) are destructively directed against one's own healthy body tissue in phases. In doing so, they damage cells of the central nervous system.
To prevent this, the antibody natalizumab was developed, among other things. It is used in highly active relapsing MS and is intended to alleviate the severity of the acute MS relapses and slow down the progression of disease-related disabilities.
Natalizumab prevents immune cells from migrating to the brain
Natalizumab itself is a so-called humanized monoclonal antibody that is directed against certain surface structures (adhesion molecules) of leukocytes.
Specifically, natalizumab blocks the so-called alpha4 integrins (VLA 4). As a result, leukocytes can no longer cross the blood-brain barrier. They are quasi “locked out” of the brain - a misdirected MS-related damage to the brain tissue can be effectively prevented.
Natalizumab has a quick onset of action, is usually administered every four weeks and is very effective and well tolerated. Typical side effects include urinary tract infections, headache and joint pain, nausea or even slight upper respiratory tract infections.
A long-term deficiency of immune cells in the brain promotes PML
Despite the promising properties in MS therapy, treatment with natalizumab also has a downside:
Doctors observe an increased risk of PML, particularly when natalizumab is administered over a longer period of time for more than two years. Experts assume that pathogens located there can no longer be adequately combated due to the long-term blocked path of leukocytes into the brain.
Patients are even more likely to develop PML if they have received immunosuppressants prior to natalizumab. Before starting therapy, doctors therefore pay particular attention to the fact that those affected are not weakened by their immune system.
They also estimate the possible risk of PML prior to natalizumab treatment, usually using a JCV antibody test. If it is positive, the patient is considered to be the carrier of the virus. Doctors then usually switch to another therapy.
Even if the JC virus test is negative, there is still a risk of PML. For example, patients could become infected with the JC virus during treatment.
Other MS drugs are also at risk
Natalizumab is the drug that is currently most commonly associated with PML. But there are other drugs that doctors typically use for MS that carry the risk of PML:
- Dimethyl fumarate: Agent against relapsing MS, among other things it inhibits inflammatory messenger substances, exact mechanism of action still unclear
- Fingolimod: also used in highly active relapsing MS (like natalizumab); prevents immune cells (especially the lymphocytes) from reaching the central nervous system from the lymph nodes, for example
Despite the relationships described, PML is not a common side effect of MS therapy.
You can find more information about common treatments for multiple sclerosis here.
How does progressive multifocal leukoencephalopathy manifest itself?
The symptoms of PML depend on where in the central nervous system the JC viruses attack nerve cells and where the myelin sheaths perish. Since the affected nerves can no longer transmit electrical impulses, their actual function fails (e.g. controlling muscles, language, vision, thinking).
Typical symptoms of progressive multifocal leukoencephalopathy include:
- Drowsiness, especially in the early stages of the disease
- Change of character and character
- Impaired coordination of movements (ataxia)
- Sensory disturbances (sensory disturbances, paresthesia)
- Progressive symptoms of paralysis
- Half-sided paralysis (hemiparesis)
- Visual disturbances (e.g. unilateral loss of field of vision, called hemianopia)
- Speech disorder (dysarthria)
- Swallowing disorder (dysphagia)
- Loss of speech ability (speech disorders, aphasia)
- headache
- Fits (seizures)
- Incontinence
Especially in the early stages, the symptoms can resemble those of a multiple sclerosis attack (in MS, the nerve medullary sheaths also perish). Therefore, it is easy to confuse the PML signs observed with MS. However, the symptoms of PML usually increase and worsen quickly.
Examinations and diagnosis
The suspicion of progressive multifocal leukoencephalopathy arises on the one hand from the symptoms (rapid progressive loss of motor and cognitive abilities). On the other hand, from an existing, pronounced immune deficiency (e.g. in the case of advanced HIV infection or under immunosuppressive treatment).
The doctor receives the first important information by asking about the patient's medical history. He also recognizes the extent of the symptoms through a physical examination (especially neurological examination).
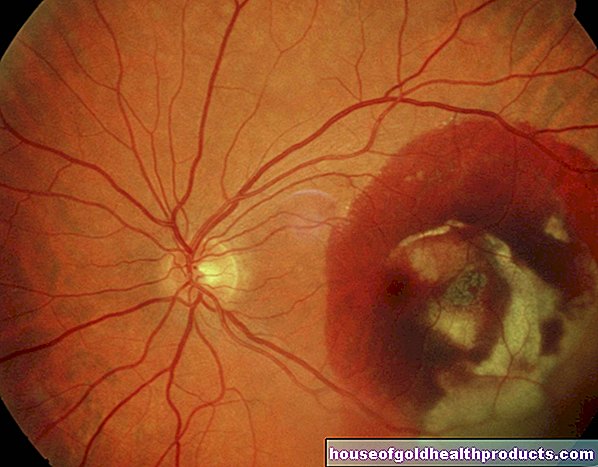
The doctor then arranges for a magnetic resonance tomography with contrast agent (contrast medium MRI, nuclear spin). With the imaging procedure, doctors can visualize possible changes in tissue (lesions, demyelinating / demyelinating foci) in the brain. In PML there are typically several such lesions in different locations (multifocal).
The MRI is followed by a so-called liquor examination. Doctors take a sample of the cerebrospinal fluid ("nerve fluid", liquor) from the area of the lumbar vertebrae using a special needle (lumbar puncture). A polymerase chain reaction (PCR) then clarifies whether the cerebrospinal fluid contains characteristic JC virus DNA traces.
A CSF examination is an essential examination measure to clarify specific infections of the central nervous system (CNS).
If necessary, the amount of virus is determined by qPCR (quantitative polymerase chain reaction) in order to evaluate the progress of the PML. After a positive PCR result with a matching finding in the MRI examination, PML is considered to be diagnostically confirmed.
Doctors then immediately initiate appropriate therapy in order to optimally care for patients and to stabilize their general state of health as well as possible.
Treatment of progressive multifocal leukoencephalopathy
There is currently no standardized causal treatment for progressive multifocal leukoencephalopathy available. This means that there is currently no (tested) treatment with drugs that could prevent the JC virus from multiplying. There is also no vaccination or targeted prophylaxis against the pathogen that causes PML.
Depending on the cause, the therapeutic approaches chosen by the treating physicians therefore differ significantly:
- in HIV patients: aggressive "highly active antiretroviral therapy" (HAART)
- If the immune system is weakened by medication: discontinue immunosuppression as soon as possible, if necessary blood wash.
- experimental treatment approach: adoptive immunotherapy with virus-specific T cells.
Treatment of PML in people with HIV
Doctors rely on "highly active antiretroviral therapy" (HAART, also cART for "combined antiretroviral therapy") for HIV patients. In this case, patients receive three or more HIV drugs at the same time, usually in high doses, in order to suppress the multiplication of the HI virus as best as possible within a short time window.
This is supposed to slow down AIDS and stabilize the number of T-defense cells in order to strengthen the immune system as best as possible, especially in the short term. This can then ideally fight the JC viruses and stop the PML.
The following groups of active ingredients are available for HAART, which complement each other in their mode of action and are used in different combinations:
- Reverse transcriptase inhibitors: disrupt the replication of the HI virus at the molecular level.
- Integrase inhibitors: Inhibit an HIV enzyme that mediates the incorporation of virus DNA into the DNA of human cells.
- Protease inhibitors: disrupt the production of virus proteins. So-called “boosters” can slow down the breakdown of protease inhibitors so that they work longer.
- Entry inhibitors: prevent the HIV virus from entering the human cell (rarely used in the first attempt at HIV therapy).
If PML affects HIV patients who are already receiving combination therapy, doctors review the preparations used. The optimal effectiveness of HAART depends on many factors - including genetic predisposition, the combination of active ingredients and the existence of possible resistance to HIV drugs. A change can improve the immune status and thus possibly push back the PML.
You can read more about the treatment of HIV / AIDS and its side effects in our specialist article "HIV infection and AIDS".
PML with excessive inflammatory response (PML-IRIS)
HAART can cause inflammatory immune reconstitution syndrome (IRIS) in some cases. In the course of its short-term recovery, the immune system generates an intense (systemic) inflammatory reaction against opportunistic pathogens such as the JC virus.
If you have PML, doctors also speak of PML-IRIS or inflammatory PML. The condition of those affected worsens - contrary to actual expectations. Further injuries (lesions) or edema can form in the brain tissue.
Doctors try to counteract the excessive immune reaction with steroids ("cortisone"). However, there is currently no clearly recommended therapy strategy.
Treatment of PML in immunocompromised patients
Doctors immediately stop medication if PML develops as a result of immunodeficiency treatment.If necessary, blood washing treatments are also carried out in order to remove the active ingredient from the body as quickly as possible.
The administration of the active ingredients mefloquine and mirtazapine can be considered as a support. In laboratory tests, both drugs showed a certain antiviral effectiveness against the JC virus - however, the use of this combination of active ingredients is controversial in medical science.
The health status of PML patients is closely monitored by continuous imaging (MRI). Some doctors consider a repeated lumbar puncture with subsequent PCR pathogen detection as an additional follow-up control.
Experimental T cell transplant treatments
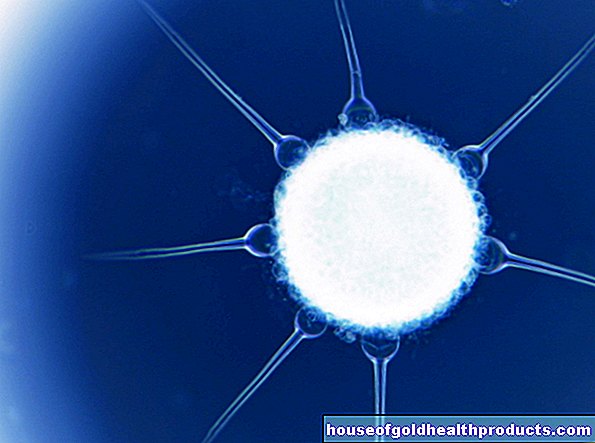
A promising experimental approach to the treatment of progressive multifocal leukoencephalopathy is what is known as adoptive immunotherapy. Alternatively, experts speak of virus-specific T-cell therapy. T cells, also known as T lymphocytes, are a type of natural defense cell in the body.
In adoptive immunotherapy, the deficiency of the body's own immune cells is replaced by the administration of processed T lymphocytes. These mostly come from healthy donors, but depending on the case of illness, they can also be taken from the patient himself.
Before the PML patient receives the T cells, they are specifically exposed to the pathogen in the laboratory. The T cells can “adjust” to the germ. Subsequently, multiplied in cell cultures and administered to the affected person, in the best case scenario, the immune system can fight the JC virus infection in a targeted and long-lasting manner.
This experimental approach can also cause excessive defense reactions against the JC virus.
Chances of recovery in progressive multifocal leukoencephalopathy
Due to the diverse causes of PML, the chance of recovery cannot be estimated across the board. If left untreated, the prognosis is very poor and is fatal within a few weeks to a few months. Untreated patients survive longer than three years only in exceptional cases.
When it comes to treatment, the earlier doctors diagnose PML, the higher the chance of a cure. Estimated chances of survival based on data collected so far add up to
- up to 50 percent of HIV-associated PML treated with HAART
- up to 70-80 percent with natalizumab-associated PML (after discontinuation of natalizumab therapy)
There are some newer therapeutic approaches with individual positive courses. However, these must be examined in more detail in (further) studies. Basically, PML remains an extremely serious disease. Survivors may also suffer persistent neurological damage.
Tags: eyes menshealth home remedies




.jpg)