Pudendal neuralgia
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Pudendal neuralgia (pudendal neuralgia) is a rare disease that is accompanied by lightning-like pain in the area between the genitalia and anus. It occurs about twice as often in women as in men. In addition to burning pain, disorders of sexual function and urinary and stool continence can also occur. Pudendal neuralgia can have various causes. Read everything you need to know about pudendal neuralgia here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M79

Pudendal neuralgia: description
Pudendal neuralgia is a rare disease. It is described as neuropathic because it affects the peripheral nervous system. Strictly speaking, this is only pain that can be assigned to the so-called pubic nerve (pudendal nerve). In some cases, unexplained chronic pain in the pelvis or genital area is also referred to as pudendal neuralgia. Women get sick about twice as often as men.
Pudendal Neuralgia: Anatomical Fundamentals
The pudendal nerve (pubic nerve) is responsible for the sensitive perception of the anus, perineum and testicles or labia. Doctors refer to the region between the scrotum and anus in men or between the vagina and anus in women as the dam. The pubic nerve also innervates the muscles of the pelvic floor and the external anal sphincter. It is therefore important for urinary and stool continence as well as for sexual function.
The pudendal nerve is made up of various nerves that leave the lower spinal cord and attach to each other. It runs laterally through various structures of the pelvis. In the so-called Alcock Canal, it pulls forward and then divides into various small branches. The Alcock's Canal is an important bottleneck in the course of the pudendal nerve - entrapment of the nerve in this area can lead to pudendal neuralgia.
Pudendal neuralgia: symptoms
Pudendal neuralgia manifests itself as severe pain in the genital and perineum area. Men feel the symptoms mainly in the perineum and rarely in the penis. Women describe discomfort in the area from the lower external vagina to the anus. Most of these are one-sided and may occur alternately. The symptoms of pudendal neuralgia rarely exist on both sides at the same time.
Patients describe the pain as burning, stabbing, shooting, dull, or pressing. Some also speak of a “razor blade feel”. In a few cases, the patients also experience abnormal sensations (paresthesia) or muscle paralysis. Possible numbness can sometimes make urination and bowel movements no longer properly controlled. Pudendal neuralgia can therefore lead to urinary and fecal incontinence. In addition, in rare cases the sexual function can be disturbed.
The symptoms increase when sitting and improve when standing or sitting on the toilet. The reason for this is the pressure relief in the small pelvis. The patient's sleep is usually not disturbed by the symptoms.
Pudendal neuralgia: causes and risk factors
There are many different causes of pudendal neuralgia. Most often there is a mechanical cause behind it. This means that the pubic nerve is irritated or constricted by other structures as it travels through the pelvis. The mechanical damage occurs, for example, when pressure is applied to the dam, such as when riding a bicycle. Operations in which the patient is kept in the same position for a long time can also lead to pressure injuries and thus to pudendal neuralgia.
Other causes of pudendal neuralgia can include:
- Pelvic injuries such as a broken pelvis, gunshot or stab wounds
- gynecological diseases such as endometriosis
- a difficult birth
- Vascular diseases of the pelvis such as thrombosis or varicose veins
- connective tissue narrowing of the Alcock canal
The following diseases are less common causes of pudendal neuralgia:
- Herpes zoster (shingles)
- Cancer diseases in the pelvis
- Diabetes mellitus
Pudendal neuralgia: examinations and diagnosis
If you have pain in the perineum and genital area, your general practitioner will refer you to a urologist, gynecologist or proctologist. The task of these specialists is to first rule out other diseases that can cause symptoms similar to pudendal neuralgia (see below). Once this has happened, the pudendal neuralgia can be diagnosed and treated as a nerve disease by a neurologist.
First, your doctor will ask you in detail about your medical history (anamnesis). He will ask you the following questions, among others:
- Since when are you having those complaints?
- Are the complaints worse on one side than the other?
- How would you describe the pain?
- Do you have diabetes or shingles?
Then the physical exam follows. It is typical of pudendal neuralgia that pressure in the vagina, rectum or perineum causes pain. Magnetic resonance imaging (MRI) is then used to take an image of the pelvis and spinal cord. This can be used to identify structures that may press on the pubic nerve or the lower spinal cord, such as tumors or herniated discs.
Pudendal neuralgia: diagnosis using pudendal block
Often, pudendal neuralgia is diagnosed by attempting therapy. An anesthetic (local anesthetic) is injected along the pubic nerve three times under image control (usually by computer tomography, CT). This process is also known as pudendal blockade. If the anesthesia brings about an improvement in the symptoms, it is assumed that it is pudendal neuralgia. If the pudendal block is carried out soon after the onset of symptoms, it can bring about long-term improvement.
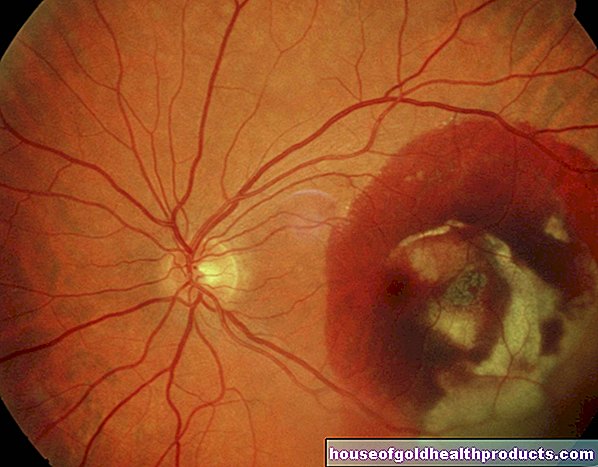
Pudendal neuralgia: measurement of nerve conduction velocity
By measuring the nerve conduction velocity (NLG), damage to the pudendal nerve can be detected, which can lead to pudendal neuralgia: In electroneurography (ENG), electrodes are stuck to the areas of the skin that are innervated by the pudendal nerve. The nerve is stimulated by electricity and the speed at which the nerve transmits the information can be measured. In pudendal neuralgia, the nerve conduction velocity is changed.
Pudendal neuralgia: excluding other diseases
Diagnosing pudendal neuralgia is often difficult, and it often takes a few months to diagnose. The reason for this is that many diseases can trigger similar symptoms. These must first be excluded. Such diseases are, for example:
- Skin inflammation
- Diabetes mellitus
- Tumors of the nerves and spinal cord (neurinoma, ependymoma)
- psychological illnesses
- Nerve damage from radiation therapy
Pudendal neuralgia: treatment
There are many ways to treat pudendal neuralgia. If there is an underlying disease behind it, it should be treated first. This means that, for example, the sugar level in the blood of a patient with diabetes mellitus must be correctly adjusted or a tumor that has grown in the pelvis needs to be treated.
Pudendal neuralgia: pain relievers
Various pain relievers can help to get the acute pain attacks under control. First, try one of the following ingredients:
- Acetylsalicylic acid (ASA)
- Paracetamol
- Diclofenac
- Ibuprofen
- Naproxen
- Metamizole
If these don't help, your doctor may prescribe stronger pain relievers (opioids such as tramadol, dihydrocodeine, or hydromorphone). These are available, for example, as tablets, plasters or suppositories.
In the long term, the pain can be treated with antidepressants or anticonvulsants. Antidepressants (such as amitriptyline or mianserin) are actually used to treat depression, but they also have an analgesic effect.
The group of anticonvulsants (anticonvulsants) is used in a variety of ways. When treating pudendal neuralgia, they slow down the transmission of pain signals in the nerves. The anticonvulsants include, for example, gabapentin, pregabalin, carbamazepine and lamotrigine.
Your doctor can also combine these painkillers.
With pudendal neuralgia therapy - as with any other pain therapy - it can take a while until an improvement is seen and until the individual, suitable combination of active ingredients has been found for each patient.
Pudendal neuralgia: TENS
The so-called TENS (transcutaneous electrical nerve stimulation) is electrical stimulation therapy. Electrodes are attached to the painful areas. The current impulses that are given through them irritate the nerves, but are not perceived as painful for the patient. They should serve to reduce the transmission of pain to the brain.
Pudendal neuralgia: further measures
Psychological accompaniment of pain therapy for pudendal neuralgia can provide further relief. Through patient education and various relaxation methods, it is possible to prevent the pain from becoming chronic and then becoming extremely difficult to treat. Supportive therapeutic measures can be found in alternative medicine, such as homeopathy, acupuncture or osteopathy.
Pudendal neuralgia: operative therapy
There are several so-called invasive procedures that can be used to treat pudendal neuralgia. An intervention is called invasive in which the body is penetrated, for example if the skin as a barrier is damaged. The already mentioned pudendal block is considered a minimally invasive therapy. The pubic nerve is numbed with local anesthetics. Another option is to inject cortisone on the nerves. However, this can only be done a few times, otherwise the nerve will be damaged.
During the operation known as neurolysis, the pudendal nerve is exposed. In this way, any pressure that is on him (for example from scar tissue) is relieved. The nerve is exposed either from behind through the gluteal muscles or through the perineum or vagina.
Pudendal neuralgia: disease course and prognosis
Predicting pudendal neuralgia is difficult because of the many different causes. It is important to treat the pain of pudendal neuralgia as early as possible so that it does not become chronic.
Tags: palliative medicine prevention Baby Child




.jpg)