Diaper thrush
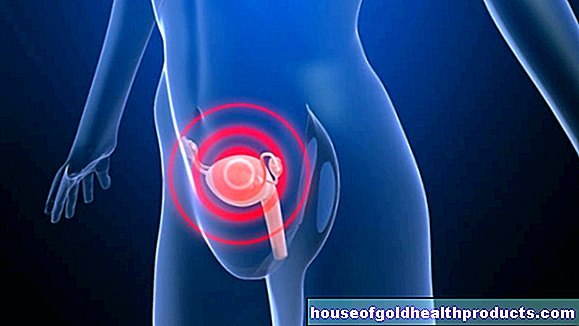
All content is checked by medical journalists.Diaper thrush is an infection with the yeast Candida albicans that is common in babies. The fungus multiplies in the diaper area and causes a red rash that is often associated with pustules and scales. Mostly the baby's bottom and genitals are affected, sometimes the thighs, stomach and back as well. Read here how you can recognize diaper thrush and how you can treat it.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B37
Windelsoor: description
Diaper thrush is a specific form of diaper rash, i.e. an inflammation of the skin in the diaper area of babies. It goes back to an infection with Candida albicans, a common yeast fungus. Therefore, one sometimes speaks of a diaper fungus or - more generally - of a candidiasis.
Candida albicans can infect other areas of the body in babies as in adults, for example the oral mucous membranes, moist skin folds such as groins, anal folds or the armpits, intestines and esophagus, and in individual cases also other internal organs. However, this occurs much less often than diaper bog.
Diaper thrush is widespread in all countries where babies are commonly swaddled. Babies are particularly often affected in the first twelve months of life. Almost every baby has a sore bottom, and it is here that the diaper fungus spreads very quickly. But not only infants can get sick - also in adults who wear a diaper for reasons of incontinence, a diaper fungus can spread. In any case, the most important therapeutic measure is to keep the diaper area as clean and dry as possible.
Diaper thrush: symptoms
With diaper thrush, the baby initially shows typical symptoms of diaper rash. The infection usually begins with a slight reddening in the area of the anus, which later becomes deep red and spreads over the genitals to the entire diaper area. In some cases, the diaper fungus also affects the thighs and the lower back and stomach area.
A characteristic of Windelsoor are red, sometimes white-rimmed blisters and pustules, some of which flow together to form red areas. In addition, the skin often forms a whitish, scaly rim around the edges of the rash. In contrast to a Candida infection of the mucous membranes, there are usually no white deposits to be found in diaper thrush.
For the baby, the diaper fungus causes itching and pain. As a result, the infant may be restless and cry a lot, especially when wetting and cleaning the affected area. The fungus can also be transmitted to other parts of the body via the hands, for example to the mouth. This is why oral thrush and diaper thrush often occur together in infants.
Diaper thrush: causes and risk factors
The cause of diaper thrush is Candida albicans, a yeast that is also known as thrush fungus. This pathogen is widespread: Candida fungi can be detected in most healthy people, especially in the intestines, in the mouth and throat, on the fingers and on the genital organs. This is where the fungi usually settle without causing symptoms. Their increase is kept in check by the body's defense system.
Under certain conditions, however, the Candida fungus can begin to multiply strongly. This is known as an opportunistic infection - the pathogen takes advantage of a chance that presents itself to become infected. In babies with diaper thrush, this happens on the one hand because they do not yet have a fully developed immune system. On the other hand, the skin in the diaper area is often attacked anyway, which makes a fungal infection easier. The warm and humid environment in the diaper, often enriched with stool and urine, softens the skin and makes it more prone to friction and irritation. The pre-damaged skin offers an ideal attack surface for germs such as fungi - and thus also for diaper thrush.
Candida albicans can get to the baby's bottom in various ways - either from the outside through the parents' hands, the changing pad or the diaper itself. In some cases, the fungus settles in the baby's intestines unnoticed and eventually develops into diaper thrush, if it multiplies in the sore anus area.
Diaper thrush: examinations and diagnosis
The diagnosis of diaper thrush is usually made by the pediatrician. He asks the baby's caregivers how long the redness began and how it started. He also wants to know whether the baby is showing any other abnormalities and symptoms, such as whether there are any problems with drinking.
The most important clue to the diagnosis of diaper thrush gives the doctor the characteristic complexion with a red rash, confluent pustules and scaly edges. On the basis of the shape of the rash, the doctor can often distinguish whether it is a pure skin irritation from the diaper (typical W-shape), whether the infection is primarily triggered by bacteria (weeping reddening of the skin and blisters) or whether a diaper fungus is present.
If diaper thrush is suspected, the doctor will also examine other parts of the baby's body (especially the mucous membranes of the mouth) to check whether the fungus has also settled there.
The proof of fungus secures the diagnosis of diaper thrush
However, the diagnosis is often difficult to make with the eye alone, as rashes of various causes often look very similar. In addition, it is not uncommon for bacteria and diaper fungus to be involved in the infection at the same time. A smear from an inflamed area of skin, which is examined in the laboratory for Candida fungi and bacterial pathogens, then provides certainty. Sometimes a stool sample is also useful for diagnosis. If a particularly large number of fungi can be detected in the baby's stool, this is an indication that a strong fungal colonization in the intestine has triggered the diaper thrush.
Diaper thrush: treatment
To treat diaper thrush, the doctor will usually prescribe one or more skin pastes for the baby. A soft zinc paste protects the skin and helps wound healing. Antifungal agents, so-called antimycotics (mostly clotrimazole or miconazole), act directly against the pathogen. In the case of diaper thrush, they are also applied to the affected areas as a paste.
In the case of severe inflammation, the doctor may prescribe a paste containing hydrocortisone for a short time. If there is also thrush in the mouth or bowel area, the baby is also given an antifungal agent (usually nystatin) as a gel or solution to swallow.
What you can do yourself at Windelsoor
The main therapy for diaper thrush is to keep the diaper area as clean and dry as possible so that the inflammation subsides and the skin can heal. The following tips are helpful:
- Change your child's diapers as quickly as possible. It is ideal with diaper thrush if the baby does not wear a diaper at all from time to time.
- Use particularly absorbent and breathable disposable diapers or cotton diapers. You should boil the latter after each use.
- When changing the diaper, wash the baby's skin with lukewarm water and then dry it gently but carefully, e.g. with a cloth or a hair dryer on a lukewarm setting. Then apply the paste before "wrapping up" the baby again.
- Always use a fresh mat on the changing table and wash your hands carefully afterwards.
- Mild and anti-inflammatory baths can be good for the child's skin with diaper thrush, for example oat, wheat bran and oil baths.
Diaper thrush: disease course and prognosis
It is important to treat diaper thrush immediately, otherwise the inflammation can spread further and further. Therapy then becomes increasingly difficult.But if you react quickly and consistently carry out treatment, you can quickly get a grip on diaper thrush.
Diaper thrush: prevention
Safe prevention is not possible with Windelsoor. However, there are various hygiene measures you can take to reduce the likelihood that your child will develop diaper fungus:
- Change your child's diaper frequently - especially if they have diarrhea.
- With every diaper change you should clean the skin in the diaper area thoroughly but gently (do not use harsh soap!).
- Dry the skin well after cleansing - moisture promotes diaper thrush and other infections. By the way, dabbing and blow-drying is more gentle on the skin than rubbing it dry.
- Be careful with baby powder - some infants react with skin irritation.
- Let your baby kick or crawl naked as often as possible. Light and air on the bottom prevents diaper thrush and other infections.