Cortisol
and Eva Rudolf-Müller, doctorEva Rudolf-Müller is a freelance writer in the medical team. She studied human medicine and newspaper sciences and has repeatedly worked in both areas - as a doctor in the clinic, as a reviewer, and as a medical journalist for various specialist journals. She is currently working in online journalism, where a wide range of medicine is offered to everyone.
More about the experts All content is checked by medical journalists.Cortisol is a hormone made in the adrenal gland and broken down in the liver. It belongs to the group of glucocorticosteroids and has numerous functions in the body. Among other things, it influences the circulation and the excretory function of the kidneys. Here you can read everything you need to know about the formation and function of cortisol, normal values and diseases that affect cortisol levels.
What is cortisol
Cortisol (also called hydrocortisone) is a steroid hormone made in the adrenal cortex. It then enters the bloodstream. The hormone is broken down in the liver and finally excreted in the urine via the kidneys.
How is cortisol made?
The body controls cortisol production with the help of a sensitive control circuit of various hormones. At the top is the corticotropin-releasing hormone CRH from the hypothalamus (part of the diencephalon). This is released in spurts and promotes the formation and release of a hormone of the pituitary gland (pituitary gland) - the ACTH (short for adrenocorticotropic hormone).
The ACTH in turn stimulates the formation and release of cortisol in the cortex of the adrenal gland. Under the influence of ACTH, the cortisol concentration in the blood increases after just a few minutes.
But our body also has a feedback mechanism built into the control loop: The released cortisol inhibits the release of CRH and ACTH, so that there is no continuous production and an excess of cortisol.
What are the tasks of cortisol?
The main task of cortisol is to provide energy from the body's energy stores. At the same time, it reduces the body's energy expenditure. Since this is particularly important in stressful situations (lack of food, physical exertion or psychological stress), cortisol is also known colloquially as the "stress hormone".
In summary, cortisol has the following effects:
- It activates or inhibits the transcription of various genes, so to speak, the reading of the genetic information stored in the genes.
- As an antagonist to insulin, cortisol raises the blood sugar level.
- It promotes the breakdown of the body's own protein stores.
- It supports the dissolution of fat stores, among other things by increasing the effect of adrenaline.
- It increases the strength of the heart muscle, blood pressure and breathing rate.
- It prevents inadequate immune system responses and inhibits inflammation.
- It inhibits the growth in length of bones.
- In the central nervous system, cortisol increases attention and information processing, improves memory and stimulates the appetite.
In addition, cortisol is of great importance for the development of the embryo, more precisely for the development of the lungs, kidneys and heart as well as the development of the immune system.
When is the cortisol level determined?
The cortisol level is particularly important in the diagnosis and control of diseases of the adrenal gland such as:
- Cushing's disease (disorder of the pituitary gland)
- Adenoma of the adrenal cortex (benign growth)
- malignant tumor of the adrenal cortex
- ACTH-producing tumor (for example, small cell lung cancer)
- Dysfunction of the adrenal cortex (Addison's disease)
- Adrenogenital syndrome (metabolic disorder with reduced cortisol production)
The doctor can measure the cortisol in the blood as well as in the urine and saliva.
Cortisol: Function Tests
In order to check the function of the hormonal control circuit around the cortisol, the doctor uses a series of function tests. In these, it stimulates or inhibits individual steps in the control loop and observes the body's reaction. Examples of such functional tests:
In the CRH test, the doctor gives the patient the hormone CRH. In healthy people, there is an increase in the "secondary hormones" ACTH and cortisol.
The ACTH test gives ACTH, which usually increases cortisol levels. If the adrenal cortex is disturbed, this increase in cortisol does not occur or is significantly reduced.
In the metopirone test, the doctor gives the patient metopirone - a substance that inhibits the enzyme 11-beta-hydroxylase. This ensures the conversion of deoxycortisol into cortisol. The enzyme blockade causes the cortisol level to drop, which in healthy people triggers an increase in ACTH. The body wants to increase cortisol production with it, but this only leads to an increase in deoxycortisol due to the enzyme inhibition. If this increase does not occur, there may be an impaired release of ACTH or an enzyme defect in steroid hormone synthesis.
In the dexamethasone inhibition test, the doctor gives the glucocorticoid dexamethasone, which normally interferes with the release of ACTH, causing the cortisol level to drop. If this is not the case, this can be an indication of abnormal hormone production outside the control loop (hypercortisolism).
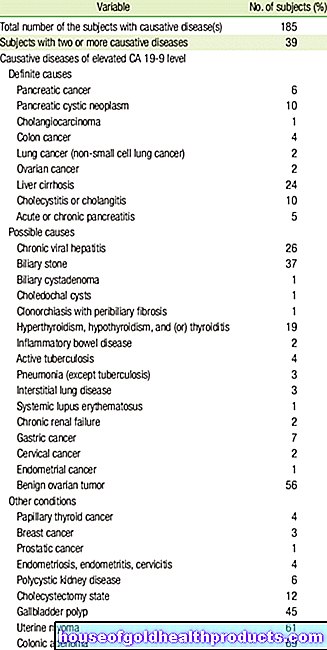
Cortisol values: table with normal values
The cortisol level fluctuates significantly during the day due to the bursts of CRH release. It is therefore important when the blood sample is taken from the patient. Depending on the age group, the following normal values apply for the blood sample at 8 a.m.
|
age |
Normal cortisol values (blood) |
|
up to 1 week |
17 - 550 nmol / l * |
|
2 weeks to 12 months |
66 - 630 nmol / l |
|
1 to 15 years |
69 - 630 nmol / l |
|
16 to 18 years |
66 - 800 nmol / l |
|
from 19 years |
119 - 618 nmol / l |
* Conversion to micrograms per deciliter: nmol / l x 0.0363 = µg / dl
The cortisol level is highest in the morning. During the day it sinks. With a blood sample taken at 11 p.m., the cortisol level is usually below 138 nmol / l in all age groups.
Cortisol in the urine
Cortisol can also be determined in the 24-hour urine collection. The normal range for all age groups is 79 to 590 nmol / 24 h.
When is cortisol low?
A chronically low cortisol concentration is called hypocortisolism. Typical complaints include decreased performance, weakness, nausea and low blood pressure. The cause is a dysfunction of the adrenal cortex (adrenal insufficiency). Depending on the location of the disorder, the doctor differentiates between primary, secondary and tertiary forms of insufficiency:
Primary hypocortisolism (Addison's disease)
In primary hypocortisolism, also called Addison's disease, the disorder is directly in the adrenal cortex. In almost all cases this is due to an autoimmune disease that leads to the destruction of the adrenal cortex. Rarer causes are:
- Bleeding
- Adrenal cortex tumors (also metastases from tumors in other parts of the body)
- Infections such as tuberculosis
- Removal of the adrenal gland during an operation
- Use of certain medications (such as the sleep-inducing anesthetic etomidate)
In addition to the general symptoms of low cortisol levels, unfortunately, patients with Addison's disease suffer from hypoglycaemia, loss of fluid and sodium through the kidneys, over-acidosis (acidosis) and severe skin pigmentation.
Secondary and tertiary hypocortisolism
If the damage is in the brain, i.e. in the pituitary gland or in the thalamus, the doctor speaks of secondary or tertiary hypocortisolism. The most common cause is the abrupt discontinuation of long-term cortisol therapy. Sometimes, however, there is also trauma or large benign growths (adenomas) behind it.
When is cortisol elevated?
If the cortisol is too high, the doctor speaks of hypercortisolism or Cushing's syndrome. The majority of Cushing's syndromes are due to the administration of glucocorticoids, such as in autoimmune diseases. Other reasons for increased cortisol levels are cortisol-producing tumors of the adrenal cortex or ACTH-producing tumors. The latter can arise in the pituitary gland as well as in other regions of the body.
By the way: The term Cushing's syndrome must not be confused with Cushing's disease. While Cushing's syndrome is another word for hypercortisolism, Cushing's disease is a benign tumor of the pituitary gland that produces ACTH independently of the control circuit.
High cortisol levels: consequences
A permanently elevated cortisol level leads to, among other things:
- osteoporosis
- Atrophy of the muscles
- Fat storage on the body trunk (trunk obesity with bull neck and round full moon face)
- high blood pressure
- Connective tissue weakness
- thin skin
- delayed wound healing
- Stomach ulcer
- diabetic metabolism
- Edema (water retention in the tissue)
- depressed mood
If the present disease leads to increased ACTH levels at the same time, the synthesis of male sex hormones is increased in addition to cortisol production. In affected women, the menstrual cycle is disturbed. In addition, a male hair pattern (such as beard growth) can develop.
What to do if the cortisol level changes?
Due to the individual fluctuations in hormone levels, a single cortisol value has little informative value. Repeated measurements or the special stimulation tests mentioned above provide better information.
If the cortisol level is too high because a hormone-producing tumor is present, it is surgically removed and / or treated with medication. In the second case, drugs are administered that inhibit the synthesis of cortisol.
In the case of hypocortisolism, however, the doctor prescribes hormone replacement therapy with drugs that contain precursors of cortisol.
Tags: hospital healthy feet magazine