Antibiotics
Antibiotics are drugs that fight bacteria. So they help with diseases that arise from infection with these pathogens. They are also effective against some parasitic infectious diseases. Read here which antibiotics are available, how they work and what you should pay attention to when taking them. You can also find out more about resistance and how to avoid it.
What are antibiotics?
An antibiotic, usually antibiotics, is a medicine that works mainly against bacteria. These are tiny organisms that can cause diseases in humans. If the body does not manage to fight off the germs successfully, antibiotics can help it.
These agents kill the bacilli or at least prevent the pathogens from multiplying and spreading. This not only works with bacterial infectious diseases such as streptococci or staphylococci.
Doctors also use antibiotics against parasites. These small, pathogenic parasites include, for example, trichomonads, which inflame the female genitals, or Giardia lamblia, the cause of the diarrheal disease giardiasis.


What antibiotics are there?
There are a number of different antibiotics available. Doctors differentiate between several classes and groups of antibiotics, for example according to their mechanism of action or effectiveness. However, one of the most common classifications is based on the basic chemical structure.
The group of beta-lactam antibiotics is the largest. It includes penicillins, cephalosporins, carbapenems and monobactams. Other well-known groups of antibiotics are, for example, macrolides, fluoroquinolones and tetracyclines.
Penicillins
The active ingredient penicillin is probably the best-known antibiotic and, to a certain extent, the pioneer of all antibiotic agents. There are now numerous variations of it, which together form the group of penicillins. These include, for example, penicillin G and V, ampicillin, amoxicillin and flucloxacillin.
However, some bacteria use an enzyme called beta-lactamase to make the antibiotics ineffective. Therefore, penicillins have also been combined with active ingredients that inhibit this enzyme (e.g. piperacillin + tazobactam, ampicillin + sulbactam or amoxicillin + clavulanic acid).
Penicillins kill the germs, so they have a bactericidal effect. Doctors use the preparations against a wide variety of infections and diseases, including tonsillitis, middle ear, sinus infections and pneumonia. Penicillin is also an effective antibiotic against syphilis.

Cephalosporins
This class of antibiotics comprises five subgroups that contain a total of several active ingredients. You can already tell from the name which one belongs to it: They all start with "Cef-". According to the Paul Ehrlich Society, the cephalosporins are divided as follows:
- Group 1: e.g. Cefaclor, Cefalexin and Cefazolin
- Group 2: cefuroxime
- Group 3: including cefixime, cefpodoxime
- Group 3a: cefotaxime, ceftriaxone
- Group 3b: Ceftazidime
- Group 4: cefepime
- Group 5: Ceftaroline
In the literature, one sometimes speaks of generations instead of groups. Depending on the affiliation, the preparations have certain properties. Those of group 1 are mainly effective against gram-positive bacteria such as staphylococci and streptococci. They are used, for example, for minor wound infections or respiratory diseases.
As part of the further developments, the cephalosporins of higher groups help better and better against gram-negative germs. These include, for example, Klebsiella, Salmonella, Shigella or the intestinal bacterium E. coli, which - when "in the wrong place" - can sometimes inflame the urinary tract.
Doctors also use cephalosporin antibiotics in groups three to five in severe illnesses such as pronounced pneumonia or meningitis and bacterial blood poisoning (sepsis).
How are antibiotics taken?
In order for antibiotics to work fully, it is important to use the preparations correctly. Various forms of administration are generally available for this. There are antibiotic agents, for example, as tablets, capsules or juices.
Antibiotic infusions that are administered through the vein are common in hospitals. Colloquially, one also speaks of antibiosis. There are also antibiotic creams, ointments or drops to only use the active ingredient in a specific area (topical antibiotics).
It is best to stick to the following tips for taking antibiotics:
- Only take antibiotics if your doctor has prescribed them. Careless use can have unnecessary consequences (side effects, resistance).
- Let your doctor know what medications you are taking on a long-term basis. There may be significant interactions (see below)
- Tell your doctor if you have any known allergies.
- Let your doctor explain exactly why and how to use the antibiotic properly.
- Then keep to this agreement. If in doubt, talk to your doctor about it.
- You can also obtain important information about the prescribed product from your pharmacist in the package insert.

Interactions
If you take several drugs at the same time, they can influence each other in terms of their effects. This also applies to antibiotics. A well-known example is the "birth control pill" (contraceptives). Some antibiotics can weaken the effect of the pill. This applies in particular to the active ingredients rifampicin and rifabutin.
Still others increase the effect of anticoagulant drugs (anticoagulants, colloquially "blood thinners"). For example, when taking macrolides (e.g. azithromycin, erythromycin) and the newer anticoagulants such as apixaban or rivaroxaban.
Food also affects some antibiotics. Milk, for example, reduces the effectiveness of tetracyclines (e.g. doxycycline). This also includes dairy products such as butter, yogurt and quark. Another example is grapefruit juice, which can inhibit the breakdown of active antibiotic substances.

When should you not take antibiotics?
There are also reasons that speak against using a certain antibiotic. These can be severe organ diseases such as the liver or kidneys. Known allergies also count among the contraindications (contraindications).
For example, if you are allergic to the penicillin amoxicillin, this will most likely also happen to other penicillins. In addition, caution is advised with other preparations, as so-called cross allergies can occur with cephalosporins, for example.
How do antibiotics work?
Antibiotics generally help against bacteria and some parasites. As bacteriostatics, some preparations inhibit the growth of the pathogen. As a result, these can no longer divide and spread. Classes of antibiotics with a bacteriostatic effect are, for example: macrolides such as azithromycin and erythromycin, tetracyclines such as doxycycline and clindamycin.
There are also bactericidal antibiotics: They kill the germ. This is how penicillins, cephalosporins, fluoroquinolones, carbapenems, aminoglycosides, fosfomycin, rifampicin and metronidazole, among others, work. Few preparations have both bacteriostatic and bactericidal effects, depending on the pathogen. One example is linezolid.
Mechanism of action
Antibiotics intervene in various processes to suppress a bacterial infection. Depending on the site of action, experts sometimes differentiate between:
- Antibiotics that disrupt the formation of the bacterial wall (e.g. vancomycin, fosfomycin and all beta-lactam antibiotics such as penicillins, cephalosporins and carbapenems)
- Active ingredients that inhibit protein metabolism (e.g. macrolides, tetracyclines, genatmicin, streptomycin, clindamycin or linezolid)
- Inhibitors that are directed against the bacterial enzyme gyrase (so-called gyrase inhibitors). This is how fluoroquinolones (e.g. ciprofloxacin, levofloxacin, moxifloxacin) work
Still other antibiotics cause the genetic cord to break (metronidazole) or impair the pathogen's folic acid metabolism (cotrimoxazole).
This is how antibiotics work What tricks antibiotics use to paralyze bacteria and why the miracle weapon sometimes fails. What tricks antibiotics use to paralyze bacteria and why the miracle weapon sometimes fails.What are the side effects of antibiotics?
For all of their benefits, antibiotics can have side effects. This affects around every tenth patient - albeit mostly only slightly. The undesirable side effects that occur sometimes depend on the active ingredient used.
Gastrointestinal complaints such as diarrhea, nausea and abdominal pain are generally typical. One of the reasons for this is that antibiotics cannot differentiate between "good" and "bad" germs. The result: The natural balance of the intestinal flora, which consists mainly of bacteria, is thrown out of joint.
In addition, some people develop an allergy to antibiotics. It can appear immediately and trigger swelling of the mucous membranes, asthma attacks and circulatory problems. Or those affected get an itchy, red-spotted rash (drug eruption) after a few hours to days.
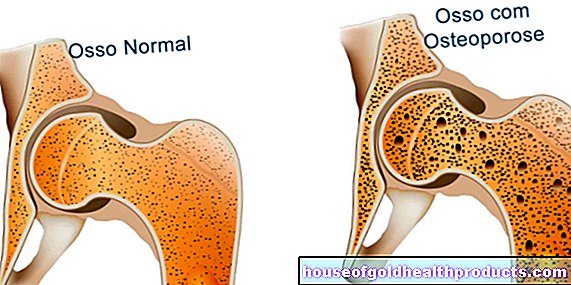
Some antibiotics can also impair organ functions, for example of the liver, kidneys and heart, and cause other side effects, including:
- Headache, dizziness, possibly seizures (sometimes with high doses of penicillins, carbapenems, gentamicin)
- Further infections, especially through fungi (e.g. carbapenems, linezolid)
- Joint, tendon, and cartilage damage from fluoroquinolones (such as ciprofloxacin, moxifloxacin)
- Skin more sensitive to sunlight (also fluoroquinolones, so avoid sunlight and think about UV protection)
- Changes in taste (e.g. metronidazole, linezolid)
- Deafness (especially aminoglycosides such as gentamicin and tobramycin as well as glycopeptides such as vancomycin)
Note:
You can read about typical side effects of your antibiotic in the package insert. In addition, contact your doctor if you have the feeling that you cannot tolerate the preparation.
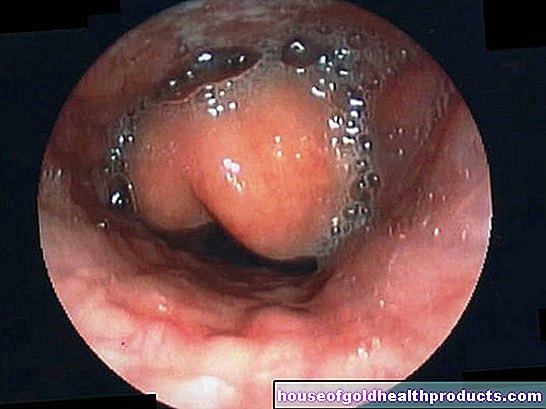
Special case of Clostridioides difficile infection
If antibiotics disturb the intestinal flora, a pathogen can cause particular problems: Clostridioides difficile. If it gains the upper hand, the intestinal wall can become seriously inflamed. Doctors speak of pseudomembranous colitis, which is associated with slimy, foul-smelling diarrhea, abdominal cramps and fever. Treatment is again with antibiotics (especially metronidazole and vancomycin).

Antibiotic resistance
Antibiotics can fight bacteria effectively. Under certain circumstances, however, they make the bacilli even more resistant. Above all, the widespread use of antibiotic agents has made bacteria insensitive to various active ingredients.
One big problem: it jeopardizes the successful treatment of infectious diseases. This becomes more difficult, the more resistance the bacteria develop. The so-called multi-resistant germs pose a challenge, especially in hospitals - and endanger the patients who are lying there, who are usually weakened anyway.
In the meantime, programs are increasingly being established around the world to counteract this development. Experts speak of "antibiotic stewardship". The aim is to improve antibiotic therapy in all respects. This includes, for example, the duration of treatment, the dosage and the choice of active ingredient. And that patients really only take antibiotics when there is no alternative.

Antibiogram
If doctors want to find out which germs are behind an infectious disease, they send samples of blood, urine or stool to a laboratory. There one then checks which bacteria can be grown and multiplied from the sample (bacterial culture).
At the same time, the experts can test which antibiotics are effective and which the germs are resistant to. Doctors call this an antibiogram or resistogram. This examination is especially important if the first antibiotic therapy does not work.
The testing takes time anyway: results can only be expected after about two days. At the beginning, doctors therefore often prescribe an antibiotic that is effective against many pathogens (broad-spectrum antibiotic). Depending on the antibiogram, the doctor may then switch to a different active ingredient.
Are antibiotics and alcohol compatible?
It is wrong that you should not drink a drop of alcohol while taking antibiotics. Rather, it depends on which active ingredient you take - and how much alcohol you drink.
Caution should be exercised with some cephalosporins, co-trimoxazole and metronidazole. With these antibiotics one can no longer tolerate alcohol. The consequences are, for example, rapid malaise, headaches, dizziness and nausea.
In general, high amounts of alcohol in particular are stressful for the body. This disrupts the recovery process - and is known not to promote health. Avoid wine, beer and the like as much as possible when you are sick.
Can I exercise while taking antibiotics?
It is less the medication than the underlying infectious disease that makes it better not to exercise. Without physical rest, the germs can attack the heart and inflame the pericardium or heart muscle. This not only applies to bacteria, but also, for example, to cold viruses and other pathogens.
Antibiotics themselves should not be underestimated either. Fluoroquinolones such as ciprofloxacin, for example, affect joints and tendons. In addition, some preparations can interfere with the electrical impulses for the heartbeat.
Sport in this case, but also in general, is an additional burden on the body. It is therefore best to limit yourself to easy walks and only resume training step by step after taking antibiotics. If in doubt, ask your doctor.


As a pregnant / breastfeeding woman, what do I have to consider with regard to antibiotics?
In some cases, pregnant or breastfeeding women also get a bacterial infection. But which active ingredients can you take as a pregnant woman? And what are the risks of antibiotics for the (unborn child)?
Antibiotics in Pregnancy
The last question in particular cannot be answered across the board. In fact, some antibiotics must not be used during pregnancy as they can harm the unborn baby. With some preparations, there is simply not enough experience.
For example, tetracycline and doxycycline and aminoglycosides such as streptomycin and some preparations that are mainly used in hospitals are not suitable. Rifampicin, co-trimoxazole and flurochinolones such as ciprofloxacin or levofloxacin are also unfavorable.
Most cephalosporins (e.g. cefuroxime), penicillins (e.g. amoxicillin) and macrolides (e.g. azithromycin) are the antibiotics of choice for pregnant women. Tried and tested on many patients, doctors prefer to use these substances.
In general, pregnant women should only take antibiotics when really necessary. Doctors make sure that the remedy does more good than it might harm. Always share your concerns and let your doctor explain the need for antibiotic therapy in detail.
Antibiotics while breastfeeding
Here, too, it depends on the particular preparation whether it is suitable for breastfeeding women or not. Basically, it can be said that final weaning is usually not necessary simply because of the intake of antibiotics.
Even a break from breastfeeding is not absolutely necessary with numerous antibiotics. However, due to the infection, for example, it can make sense to stop breastfeeding during the duration of the illness. With some antibiotics, it is also not certain in what quantities they could pass through the breast milk to the child. It is best to ask your doctor.
Tags: elderly care therapies home remedies