Allergic rhinitis
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.Allergic rhinitis is inflammation of the lining of the nose (rhinitis) caused by an allergy. If you have an allergic runny nose, symptoms such as a stuffy nose, constant sneezing and watery eyes occur. Read here how to recognize allergic rhinitis and what helps against it!

Brief overview
- Description: inflammation of the nasal mucosa caused by an allergy
- Symptoms: Typical complaints are an itchy nose, constant sneezing, scratchy throat, feeling of a "stuffy nose", itchy eyes, tiredness.
- Treatment: Avoid contact with allergenic substances; Well treatable with medication (e.g. nasal spray, antihistamines, allergy immunotherapy)
- Causes: Allergic reaction of the body triggered by allergens such as pollen, house dust mites, animal hair and mold spores
- Diagnosis: The doctor makes the diagnosis through a physical examination and a skin and blood test, among other things.
- Course: Usually easy to treat. Depending on the allergen, the symptoms occur all year round (e.g. with house dust mite allergy) or only seasonally (e.g. hay fever).
What is allergic rhinitis?
Allergic rhinitis - also allergic rhinitis or rhinitis allergica - is an inflammatory disease of the nose that is caused by an allergy. The body's defense cells react excessively to harmless particles in the air we breathe, thereby triggering inflammation of the nasal mucous membrane (rhinitis).
Allergic rhinitis is one of the most common allergic diseases. It also often occurs with other respiratory diseases such as sinusitis and allergic asthma. If the conjunctiva is also inflamed, doctors speak of allergic rhinoconjunctivitis.
About ten to 25 percent of the population are affected by allergic rhinitis, and the number is rising.
How does an allergic runny nose develop?
Within a few minutes after the person concerned inhales the triggering substance (inhalation allergen, inhalation allergen or aeroallergen) and it gets into the nose, the body reacts with an inflammation.
The cells that are responsible for the defense (the so-called mast cells) first recognize the allergen. On their surface there are so-called IgE antibodies (immunoglobulin E), which act as "antennas" and connect with the allergen. This causes the mast cell to start releasing histamine and other inflammatory substances. The lining of the nose becomes inflamed.
Since the symptoms of allergic rhinitis develop within a few minutes after contact with the allergen, doctors speak of an allergic reaction of the immediate type (type I).
Runny nose or allergy?
Since the symptoms of allergic rhinitis are very similar to those of a cold from a cold, it is not always easy for those affected to tell the difference. However, this is important in order to effectively manage the symptoms.
Usually it can be determined at the beginning of the symptoms whether the cause of the runny nose is an allergy or a cold (infection with viruses or bacteria). Because while a flu-like infection (cold) usually begins rather slowly with a scratchy throat, a slight headache or a runny nose, the runny nose with an allergy sets in suddenly and very strongly. There are also differences in the symptoms themselves.
For example, allergy sufferers usually have long-lasting, strong sneezing attacks and often sneeze one after the other. Colds, on the other hand, often sneeze sporadically and not as often in a row. Itching in the nose, mouth, roof of the mouth and throat is also more common in allergy sufferers than in people with a cold. In addition, symptoms such as fever or chills are usually associated with a cold.
Last but not least, the period in which the runny nose occurs plays a role. For example, allergic rhinitis occurs at about the same time every year (e.g. in spring) in people who are allergic to pollen. A cold, on the other hand, is more likely to occur in the colder months of the year.
See a doctor if your symptoms persist for more than a week. If in doubt, the doctor can determine whether it is a cold or an allergy.
How do you recognize allergic rhinitis?
An allergic rhinitis manifests itself through the following symptoms, among others:
- The nose itches.
- You have to sneeze all the time.
- The throat is scratching.
- Watery-clear secretion runs out of the nose ("runny nose").
- You feel a 'blocked nose' (impaired nasal breathing).
- The palate, ears or eyes also itch.
In addition, it is possible that those affected have accompanying symptoms such as headaches, head pressure or loss of appetite and feel exhausted or sick. Accordingly, people with allergic rhinitis feel less productive. Sometimes the sense of smell is also temporarily impaired.
Especially when the symptoms persist over a long period of time, many sufferers experience insomnia. For example, those who are allergic to mite droppings suffer from symptoms when they wake up at night and in the morning. As a result, he is often tired and has difficulty concentrating during the day.
Symptoms usually appear within a few minutes of exposure to the allergen.
What are the consequences of allergic rhinitis?
Since, in contrast to other allergic reactions such as food allergies or allergic asthma, there are no threatening symptoms, the allergic runny nose is often played down. Wrongly, because allergic rhinitis often massively affects the physical and mental performance, quality of life, sleep and day-to-day activities of those affected.
In addition, allergic rhinitis often occurs together with concomitant diseases such as sinusitis, nasal polyps, conjunctivitis of the eyes (conjunctivitis) and / or otitis media. It also increases the risk of developing allergic bronchial asthma if the allergy is not treated in time.
What helps against allergic rhinitis?
Treatment for allergic rhinitis includes:
- Avoid the triggering allergen (allergen avoidance)
- Medication (e.g. decongestant nasal sprays, antihistamines)
- Allergy immunotherapy (allergen-specific immunotherapy or desensitization)
Avoid triggering allergen
When treating allergic rhinitis, it is first important that those affected avoid the triggering allergens or at least largely reduce contact. Your allergist will explain and inform you comprehensively about your allergy.
The following measures will help you to largely avoid allergens:
- Animal hair allergy: Avoid contact with animals that you are allergic to (e.g. cats or dogs).
- House dust mite allergy: Cover your bed with suitable mite protection covers (so-called encasing covers) that keep the mattress free from mite excrement. Also ventilate and clean your bedroom more often. This usually helps relieve symptoms.
- Pollen allergy: It is recommended that you change your clothes after being outdoors and wash your hair before entering the bedroom.
- It is also possible to keep pollen and house dust away from your airways by wearing a respirator (dust mask).
Medication
If the symptoms do not decrease to the desired extent by avoiding the allergen, the doctor usually prescribes an antihistamine as basic therapy. In addition, he prescribes medication to treat the nose locally. In addition, nasal sprays or drugs such as Cromone are usually used, which have a decongestant effect and often relieve the symptoms quickly.
An antihistamine nasal spray is the drug of choice for mild symptoms; for moderate or severe symptoms, the doctor will prescribe a cortisone-containing nasal spray or antihistamines in the form of tablets.
Common drugs for allergic rhinitis include:
- Cromone (mast cell stabilizers) as nasal sprays: Weaker effect than antihistamines or cortisone; inhibit inflammatory messenger substances such as histamine; only work after several days of use
- Cortisone (glucocorticoids) in the form of nasal sprays: used locally in the nose; suppresses the symptoms there; has a strong anti-inflammatory effect
- Antihistamines in the form of nasal sprays or oral tablets: inhibit the inflammatory messenger substance histamine
- Decongestants or sympathomimetics as nasal sprays or drops: To decongest the nasal mucosa; should only be used for a short time to prevent inflammation of the nasal mucosa
- Leukotriene receptor antagonists (montelukast) to be taken as tablets: Weaker than cortisone; inhibit inflammatory messenger substances (leukotrienes)
If there are also eye problems (such as burning and itching of the eyes), the doctor will prescribe special eye drops with antiallergic active ingredients (e.g. antihistamines or Cromone).
Allergy immunotherapy
Another option is so-called desensitization or allergen-specific immunotherapy (AIT). It directly fights the cause of allergic rhinitis. This form of therapy aims to gradually get the immune system used to the allergen. The principle is as follows: If you give the body a small dose of the allergen at regular intervals and increase it slowly, the immune system gets used to it and the symptoms decrease.
There are two options for allergen-specific immunotherapy: Either the doctor gives injections under the skin or the patient takes drops or tablets.
The doctor will decide which treatment is suitable for you based on the type, duration and severity of your symptoms as well as individual factors such as your age, possible concomitant diseases and concomitant medication that you are taking.
Which home remedies help with allergic rhinitis?
In some cases, home remedies such as nasal rinses, herbal or homeopathic remedies can be used to support the treatment. However, the effectiveness of homeopathic remedies such as Arundo mauritanica (pile reed) and Adhatoda vasica (Indian lungwort) has not yet been scientifically proven.
Medicinal plants such as astragalus and butterbur in the form of capsules or tablets are also said to help against the symptoms of allergic rhinitis.
You can find out how to do a nasal douche correctly here.
Before taking homeopathic or herbal remedies, especially for more severe illnesses, ask your doctor for advice.
What causes allergic rhinitis?
Allergens are the cause of allergic rhinitis - substances to which the immune system reacts excessively. The main triggers of an allergic runny nose are:
- Pollen (for hay fever)
- House dust mites
- Animal hair
- Mold spores
Air pollutants (e.g. ozone, cigarette smoke, fine dust), histamine-containing foods (e.g. cheese, smoked fish, sausage or alcohol) as well as unspecific stimuli such as smells, vapors, cold or heat, in some cases additionally intensify an existing allergic rhinitis. Doctors then speak of (nasal) hyperreactivity.
Many people with a pollen allergy (hay fever) also react sensitively to other allergens that are similar to the allergen in pollen (e.g. nuts, pome and stone fruit). This is known as a cross allergy.
How does the doctor diagnose allergic rhinitis?
If you suspect an allergic runny nose, your family doctor is your first point of contact. If necessary and for further examinations, he will then refer you to a specialist who specializes in allergies (allergist).
Conversation with the doctor (anamnesis)
The doctor will first ask you carefully about your symptoms and get an idea of your home and work environment. This gives him an impression of which allergy-causing substances you may be exposed to on a daily basis.
With so-called hay fever, the symptoms occur seasonally. This usually gives the doctor a quick first hint. But there are also allergens that are difficult to track down. In this case, it is important that an allergist clarify the symptoms.
Skin test
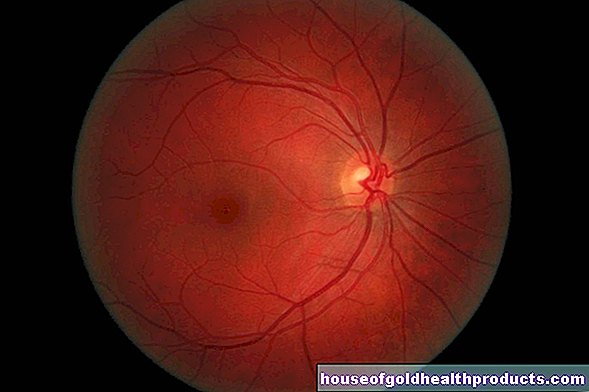
An allergy skin test (usually skin prick test) provides clarity about the triggering allergen. To do this, the doctor drips various allergen solutions onto the inside of the forearm. With the help of a fine lancet or needle, the doctor pricks the affected areas of the skin superficially. If the person concerned reacts to one of the applied allergens after five to 60 minutes with typical symptoms such as redness, itching and wheals, an allergy is present.
Blood test
The determination of the total and allergen-specific IgE antibodies in the blood provides additional information. A simple blood sample is required for this. For example, increased total IgE antibody values indicate an allergy, while the specific IgE antibodies in the blood indicate which allergen the IgE antibodies are specifically directed against.
Provocation test
The doctor can also do a nasal provocation test. He applies the suspected allergen directly to the patient's nasal mucosa under controlled conditions to see whether and what symptoms it is causing.
In so-called local allergic rhinitis, skin and blood tests are typically negative. Information about the triggering allergen is therefore only provided by one's own observation, which the doctor checks with a nasal provocation test.
How does allergic rhinitis work?
Allergic rhinitis usually begins in early childhood. Symptoms are usually most pronounced in adolescents and often decrease in adulthood. For many of those affected, the long-term prognosis is good.
Once those affected know the trigger for their allergic rhinitis and receive the right treatment, most learn to deal with their symptoms fairly quickly.Health consequences and complications, such as inflammation of the paranasal sinuses, narrowed airways or polyps in the nose, are therefore rather rare. It is important that those affected consult a doctor at an early stage if symptoms occur.
For some people (mostly younger ones), however, it is possible that the allergic runny nose worsens and that, over time, they react sensitively to several allergens at the same time. This increases your risk of complications.
However, especially with treatments such as allergy immunotherapy, it is now possible to free those affected from their allergies over a longer period of time or at least to significantly reduce the symptoms.
How long does an allergic runny nose last?
How long the symptoms of allergic rhinitis last depends on the one hand on how sensitive someone is to the triggering substance. On the other hand, it depends on how long the person concerned has been in contact with the allergen.
A distinction is made depending on the duration of the symptoms
- Episodic (intermittent) allergic rhinitis: Symptoms recur for less than four days a week or for less than four weeks (sometimes referred to as "seasonal").
- Persistent (persistent) allergic rhinitis: The symptoms persist for a long time - more than four days a week and longer than four weeks (also referred to as "perennial" or "year-round occurrence").
Flower and grass pollen occur only in certain months, such as in spring (e.g. March to August) or autumn (e.g. end of August to end of September), or in certain areas.
Allergens from house mites, animals (e.g. dogs, cats) or mold can be found in the immediate vicinity all year round (e.g. on the floor or in bed linen). Therefore, it is possible that the symptoms of exposure to the allergen will appear year round.
It is not uncommon for mixed forms to occur when someone is overly sensitive to allergens of various types (e.g. pollen and house dust mites).
Tags: travel medicine skin care hair

















.jpg)