coma
and Carola Felchner, science journalistChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane FuxCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.
Coma is a prolonged state of deep unconsciousness from which the person concerned cannot be awakened. In the deepest coma, normal reflexes are disabled. The person affected no longer fends off pain stimuli and their pupils do not respond to light. Some coma patients also slide into a so-called waking coma (apallic syndrome) or reach a minimally conscious state (MCS). Others regain full consciousness, but are almost completely paralyzed (locked-in syndrome).

Brief overview
- What is coma? Prolonged deep unconsciousness and the most severe form of impaired consciousness. There are different levels of coma from mild (patient reacts to certain stimuli) to deep (no more reaction).
- Forms: In addition to the classic coma, there is a vegetative state, minimal state of consciousness, artificial coma and the locked-in syndrome.
- Causes: e.g. diseases of the brain (such as stroke, traumatic brain injury), metabolic disorders (such as lack of oxygen, hypoglycaemia / hypoglycaemia), poisoning (e.g. from drugs, poisons, anesthetics)
- When to the doctor Always! Call an ambulance immediately if someone falls into a coma.
- Therapy: Treatment of the cause, intensive medical care, if necessary artificial nutrition / ventilation, stimulation of the brain through massage, light, music, speech, etc.
Coma: description

The term "coma" comes from the Greek. It means something like "deep sleep". A person in a coma can no longer be woken up and only reacts to a very limited extent, if at all, to external stimuli such as light or pain. In a deep coma, the eyes are almost always closed. A coma is the most severe form of impaired consciousness.
Since modern imaging techniques allow insight into brain activity, the understanding of the state of the coma has changed fundamentally. It is becoming increasingly clear that the boundaries between active consciousness and coma are fluid.
Depending on the depth of the coma, there are four levels of coma:
- Slight coma, level I: The patients react to painful stimuli with targeted defensive movements. Your pupils contract when exposed to light.
- Slight coma, stage II: The patients only fend off painful stimuli in an untargeted manner. The pupillary reflex works.
- Deep coma, stage III: The patient no longer shows any pain defense reaction, but only non-targeted movements. The pupillary reaction works only weakly.
- Deep coma, stage IV: The patient no longer shows any pain reaction at all, the pupils are dilated and do not react to light.
A coma can last from a few days to a maximum of several weeks. Then the patient's condition usually either quickly improves or brain death occurs.
Smooth transitions
A coma is increasingly no longer understood as a static state, but as a changeable process. Coma, coma (apallic syndrome) and minimally conscious state (MCS) can flow into one another. Some patients regain full consciousness but are almost completely paralyzed. Experts then speak of the locked-in syndrome (LiS; to German: being trapped / trapped syndrome).
These states differ mainly in the degree of brain activity, the existing reflexes and pain reactions and the ability to react to external stimuli. And the possibility is becoming increasingly clear that islands of consciousness could also be present in a coma.
Coma as a protective reaction
Some neuropsychologists now assume that a coma is not a passive state, but an active protective reaction. It is assumed that those affected have withdrawn to a very deep level of consciousness after brain damage. With the help of therapy, however, they can succeed in regaining access to the world.
Coma: causes and possible diseases
A coma can be caused directly by an injury or disease to the brain. Sometimes, however, severe metabolic imbalances lead to a coma. In addition, intoxication from drugs or other poisons can be the cause of deep unconsciousness.
Brain diseases
- stroke
- traumatic brain injury
- Meningitis
- Inflammation of the brain (encephalitis)
- Cerebral hemorrhage
- Epileptical attack
- Brain tumor
Metabolic disorder (metabolic coma)
- Circulatory failure
- Lack of oxygen
- Low blood sugar (hypoglycaemia)
- Hypoglycemia (hyperglycemia, hyperosmolar coma, diabetic coma)
- Renal failure (uremic coma)
- Hepatic insufficiency (hepatic coma)
Poisoning
- Drugs (e.g. alcohol, intoxicants)
- Poisons
- Anesthetics
Coma: the main forms
In addition to the classic coma, there are forms of coma in which consciousness still seems to be present to a certain extent.
Vegetative state (apallic syndrome)
The vegetative state is a state in the shadow realm between coma and consciousness. The term was coined in the 1970s. It is estimated that up to 5,000 people in Germany live in a vegetative state.
Due to their open eyes and their ability to move, those affected appear awake despite their unconsciousness. However, the gaze is either fixed or wandering around indefinitely. Patients in a vegetative state have to be fed artificially, but they can, for example, grip, smile or cry. However, in a real vegetative state, these movements are unconscious reflexes. The English term "Persistent Vegetative State" (PVS) indicates that the functions of the autonomic nervous system such as breathing, heartbeat and sleep rhythm are still working, while higher cognitive functions are paralyzed.
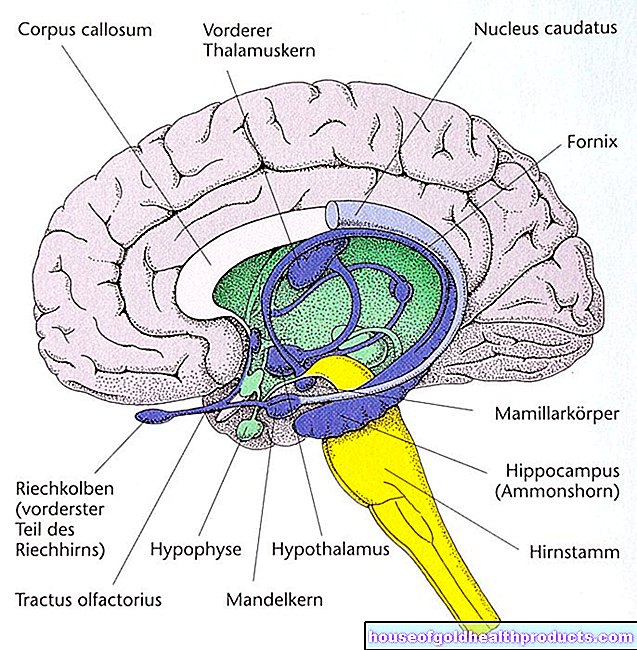
The reason for the state of the coma is damage to the cerebrum, which forms the outer layer of the human organ of thought. It envelops the deeper brain structures like a coat, which is why one speaks of the "apallic syndrome" (Greek for "without a coat"). The cerebrum processes all sensory impressions: seeing, hearing, feeling, tasting and smelling. It stores the memories and is the seat of consciousness. It can almost completely fail due to an injury, illness, or lack of oxygen to the brain.
Patients can survive in a vegetative state for many years. In some cases the brain recovers and functions gradually come back, even if only partially. According to the current state of knowledge, it is difficult to predict which brain will wake up again from the shadowy realm between consciousness and coma.
Minimally Conscious State (MCS)
At first glance, minimal state of consciousness and vegetative state appear to be confusingly similar. The patients have a sleep-wake rhythm controlled by the autonomic nervous system. Due to the open eyes, movements and mine play, they appear temporarily awake.
But while patients in a vegetative state, at least according to the doctrine, are only capable of unconscious reflexes, patients in the minimal state of consciousness occasionally show targeted reactions to external stimuli (such as sounds, touch) or even expressions of feeling in the presence of relatives.
As some patients slide from a vegetative state into the minimal state of consciousness, scientists and doctors see the boundaries between the two states as increasingly fluid.
The likelihood that someone will awaken from the Minimal State of Consciousness is far higher than when they awaken from the vegetative state. If the condition does not improve in the first twelve months, the chance that the patient will recover is significantly reduced. However, even awakened patients usually remain severely disabled due to their severe brain damage.
Artificial coma
A special case is the artificial coma, in which doctors put seriously injured or sick people with the help of anesthetics. Strictly speaking, this is not a coma, but rather a long-term anesthetic. When the medication is stopped, the patient wakes up. Since the patients are only relatively lightly sedated, some can remember events in an artificial coma.
Locked-in syndrome
The so-called locked-in syndrome is actually not a form of coma. Without further investigation, however, it can easily be confused with a vegetative state, which is associated with paraplegia. Locked-in syndrome patients are awake and fully conscious but completely paralyzed. Some at least still have control over their eyes and can communicate by blinking.
Coma: When do you need to see a doctor?
Loss of consciousness is always a medical emergency. Therefore, always call an emergency doctor. Until this arrives, you provide first aid. In particular, make sure that the patient is breathing. If not, start chest compressions immediately.
Coma: The doctor does that
It is often difficult to determine how deep a coma actually is. The fact that the patient does not respond to prompts such as "look at me" or "squeeze my hand" does not necessarily say anything about their level of awareness.
It can also be difficult to distinguish between a vegetative state and a minimal state of consciousness. It has been shown that some of the coma patients still process verbal statements.
Methods that map electrical activity in the brain are an important diagnostic aid. The energy consumption of the brain can be determined with the help of positron emission tomography (PET). Functional magnetic resonance imaging (fMRI) shows whether and which brain regions can be activated by images or sentences.
But even such brain scans are not 100 percent reliable. The diagnosis can be falsified by the fact that a patient with a minimal state of consciousness is stuck in a deeper unconsciousness during the examination. In that case, conscious moments are not captured. Experts therefore call for coma patients to be sent through the brain scan several times before the diagnosis is made.
therapy
Coma therapy initially focuses on treating the disease that triggered the coma. In addition, people in a coma usually need intensive care. Depending on the depth of the coma, they are fed artificially or even ventilated. In addition, there are sometimes physiotherapy and occupational therapy measures.
For people in a vegetative state or with a minimal state of consciousness, coma researchers are increasingly demanding permanent therapy measures that offer the brain sensory stimuli. A brain that is addressed in this way is more likely to go back to work. For example, massages, colored light, movement in the water or music are suitable, but above all loving touch and direct addressing of the patient. Relatives play a central role in activation.
At the very least, a brain scan should be used to regularly check whether the condition of long-term coma patients has improved, even if there are no external signs of this.
Koma: You can do that yourself
A person in a coma needs help. In addition to physical care, this also includes human support. Not only is this a question of ethics, but there is growing evidence that many people in coma are not completely unconscious. Treating the patient in a loving and respectful manner is therefore immensely important.
This has an effect, even if it cannot always be seen from the outside. Coma patients in particular often react to loving stimulation with a change in their heart rate and breathing. Muscle tone and skin resistance also change.
Even if caregivers and relatives cannot know how much the patients really perceive in a coma, they should always behave as if the patient could perceive and understand everything.
Tags: Diagnosis healthy feet drugs