Self harm
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.Self-harm - including self-harming behavior (SVV), auto-aggression, auto-aggressive behavior or artifacts - is understood to be behavior in which those affected consciously injure themselves (e.g. by "scratching" or scratching the skin). The behavior mostly occurs in adolescents and often arises from persistent emotional stress. Find out here how to recognize self-harming behavior, what causes it and what you can do about it!

Brief overview
- Description: Self-harming behavior (SVV) in which those affected consciously harm themselves (e.g. by scratching the skin on the arms)
- Causes: Usually long-term psychological stress (e.g. conflicts within the family) or illness (e.g. borderline disorder, depression) is the reason for the behavior.
- Symptoms: For example wounds, stitches, burns on the body (mostly on the arms and legs), bruises, scars, sleep disorders, mood swings
- Treatment: The doctor first treats the wounds, then he investigates the psychological causes and selects a suitable psychotherapy. In some cases, the doctor will prescribe psychotropic drugs.
- Diagnosis: conversation with the doctor, physical examination (e.g. examination of the wounds and scars)
- Prevention: substitute actions such as placing ice cubes on the neck, hitting the bed or pillow, taking a cold shower; In addition: Strengthening self-confidence, developing positive body awareness, learning to use social media critically
What is self-harming behavior?
Self-harm - also self-harming or auto-aggressive behavior or auto-aggression (self-aggression) or artifact action - describes various behaviors and actions in which those affected intentionally repeatedly injure themselves or inflict wounds on themselves.
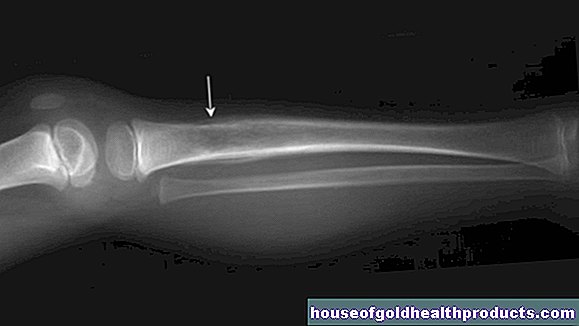
The so-called scratching - the scratching or cutting open of the skin of forearms or legs with sharp objects such as knives, shards or razor blades - is the most common method of self-harm. These are not life-threatening wounds, but small to medium-sized injuries to the skin - or tissue surface of the body.
In the ICD-10, the international classification system for diseases and health problems, self-harm is not classified as a disease in its own right. It is considered "willful self-harm in an unspecified manner".
In the DSM-5, the American guideline for mental disorders, the behavior is defined as "non-suicidal self-harm syndrome" (short: NSVV). It occurs when those affected consciously inflict damage to their own body tissue on five or more days within a year.
Self-injurious behavior can often be traced back to prolonged emotional stress and often occurs in conjunction with other mental illnesses, such as a borderline disorder or depression. According to research, every fourth adolescent is injured at least once by the age of 18.
"Scratching" is often used as a synonym for self-harm, as it is the most common method of self-harm.
What are the causes of self harm?
Self-harming behavior usually occurs due to long-term emotional stress, such as a problematic parent-child relationship or frequent conflicts with people of the same age. This behavior occurs less often in the event of acute emotional stress such as the divorce of the parents, a separation or school problems.
Reasons that people cut themselves also include low self-esteem, despair, hopelessness, sexual abuse, or neglect. In most cases, however, the behavior occurs as a symptom or with other mental illnesses, such as:
- Borderline personality disorder
- depressions
- Eating disorders such as vomiting addiction (bulimia) or anorexia (anorexia)
- Post Traumatic Stress Disorder (PTSD)
- Obsessive-compulsive disorder
- Substance abuse
- Anxiety disorders
- Conduct disorder
Autoaggressive behavior usually begins in youth between the ages of 12 and 15, but in some cases much earlier. Autoaggression is less common in adults. For most people it is a valve to relieve strong internal tension. By hurting themselves, they feel a sense of relief.
Or the self-injuries serve as self-punishment because those affected are angry with themselves. Some people become “addicted” to this condition over time and get hurt again and again.
Most often, self-harm is used to break very uncomfortable feelings (e.g. despair, self-loathing, depression, anxiety) or memories that overwhelm those affected. After traumatic events such as abuse or mistreatment, there are usually recurring flashbacks - intense, intrusive memories of the trauma - to which those affected are helpless.
Self-harm ("self-mutilation") causes an interruption or alleviation of the intensely uncomfortable emotional state. Self-harming behavior thus serves as a kind of coping strategy for those affected. It is not uncommon for other young people (e.g. friends or classmates) to "learn" and imitate self-harming behavior: the young people take on self-harming actions from others.
The role of the Internet should be noted here. Here, those affected exchange information about self-harming behavior. This can lead to the behavior being socially accepted and “normalized”.
Regardless of the reasons that lead to self-harm, almost all those affected feel a sense of relief afterwards. You will usually feel better for a short time afterwards. That is also the reason why many injure themselves over and over again. Some even become addicted to the feeling that occurs after the injury through the body's own release of endorphins (endogenous morphines, "happiness hormones").
Who is particularly affected?
Adolescents (more rarely also toddlers) with mental health problems are most often affected by autoaggression. In Germany, around 25 percent of young people injure themselves once in their life, around 19 percent of the population in adolescence are affected by self-harming behavior.
Girls and young women between the ages of twelve and 15 in particular have an increased risk of developing self-harming behavior. One of the reasons for this is that girls are more likely to direct negative feelings inwards, i.e. against themselves. They are also more likely to experience depression and anxiety, which increases the risk of self-harm.
Many boys, on the other hand, have a tendency to vent their anger and psychological tension on their surroundings. This is due, among other things, to the higher proportion of testosterone in the body. However, studies from recent years show that more and more male adolescents are affected by autoaggression.
How is self-harming behavior expressed?
Self-injurious behavior and the associated symptoms manifest themselves in many ways. The most common type, however, is “scratching” or “cutting”. This involves repeatedly cutting one's own body with sharp objects such as razor blades, knives, needles or broken glass.
But there are many other types of self-harm, such as putting out a lighted cigarette in your arm, touching a hot stove or pinching off certain parts of the body. It is not uncommon for sufferers to use multiple self-harming methods that change over time.
These include:
- scratch themselves sore or bloody
- scratch or cut themselves with sharp objects
- hit or hit hard objects
- pinch yourself
- bite yourself
- get burned
- burn yourself (e.g. with acids)
- pulling your hair out
- excessive fingernail biting
- the constriction of certain parts of the body
- constant tearing open of healing wounds
- Try to break your bones
- Intentional ingestion of harmful substances (e.g. spoiled food or cleaning agents)
The most common areas of the body injured are:
- Forearms
- Wrists
- Upper arms
- thigh
The chest, abdomen, face or genital area are less likely to be injured. The injuries are usually equally deep, grouped, lined up in parallel or symmetrically recognizable on the surface of the skin (also in the form of letters or words). It is not uncommon for these wounds to result in scars, which are known as self-injury scars or SVV scars.
Often people with SVV have insomnia. They withdraw and neglect contact with friends and hobbies that they used to have. Often, out of shame, those affected try to hide their wounds and injuries on their bodies.
Therefore, even in warm temperatures or when exercising, they often wear long clothes that hide scars from cracks or other fresh wounds. Changes in mood are also often a sign of auto-aggressive behavior. Other warning signs include:
- Frequent locking in the room or bathroom
- Neglecting one's own interests (e.g. meeting friends)
- Storing razor blades, knives or other sharp objects
- Cuts on the body (mostly on the forearm)
- Burn injuries or stitches (e.g. from needles)
- Bruises on the body
- Abrasions (especially on the knees or elbows)
How does the doctor make a diagnosis?
Self-harming behavior is a symptom that can occur in connection with various mental disorders, but also independently of them. If there is any suspicion of self-harm, the family doctor is the first point of contact. If necessary, he will refer you to a specialist.
A specialist in psychiatry or child and adolescent psychiatry assesses whether the behavior is based on a mental illness.
First of all, the doctor has a detailed discussion with the person concerned. Among other things, he asks questions (often using a questionnaire) whether there are other symptoms (e.g. depression, anxiety, hallucinations, social withdrawal, etc.) and whether there are psychosocial stresses (e.g. conflicts within the family, at school or at work). gives. How often the affected person injures himself also plays an important role in the diagnosis.
The doctor then examines the injured parts of the body and examines them for abnormalities (e.g. are the wounds equally deep, grouped, lined up in parallel or symmetrically recognizable on the surface of the skin?).
If you suspect a friend or relative is injuring themselves, contact your general practitioner, a specialist in psychiatry, or a psychotherapist.
What can you do against autoaggression?
Treatment of wounds
First of all, the doctor treats the person's wounds. A cut or burn wound must always be treated immediately. Here the risk is very high that the wound will become infected. The doctor also cleans and treats superficial injuries (e.g. by disinfecting the wound, applying a wound dressing).
If you are affected yourself, do not be afraid to go to the doctor with wounds so that he can take care of them and prevent them from becoming infected.
Psychosocial Treatment
Because self-harming behavior has different causes, it is important to adjust treatment accordingly. It is best to contact a psychologist or child and adolescent psychiatrist. Depending on the underlying disease or disorder, this person has the option of using special therapeutic methods for treatment.
Cognitive behavioral therapy, for example, has proven to be particularly effective. People with autoaggression learn new coping strategies in order to react better to stressful situations and to control their emotions. Those affected learn to analyze possible triggers for self-harming behavior in order to recognize them in good time and to react to them.
Relaxation techniques such as yoga, breathing exercises or progressive muscle relaxation help those affected during therapy to relieve pressure.
If the self-injurious behavior is based on a serious mental illness (e.g. depression, borderline disorder), the doctor may prescribe psychotropic drugs in addition to psychotherapy.Parents and other caregivers should be included in the treatment, especially in the case of adolescents. If they also use behavioral therapy, this usually contributes significantly to a successful treatment.
The person concerned should decide for himself about the treatment. Treatment against his will is not effective.
Scar removal
Depending on how deep or large the wound is, scars remain that are more or less visible. These remind those affected again and again of their previous behavior, for which they are often ashamed. Therefore, many sufferers have their scars removed by a doctor.
Various methods such as dermabrasion (grinding of the upper layer of skin), micro-needling (light needle pricks in the upper layer of skin), serial excision (step-by-step surgical reduction of the scar) or laser treatment are possible.
Special scar ointments or creams from the pharmacy also help to reduce the visibility of scars a little. However, most of these methods do not completely remove the scars.
Some people use home remedies such as compresses or gels with onion extract to apply, olive oil and marigold ointment to apply, or regular massages to improve the elasticity of the scar tissue.
The effects of these home remedies on scars have not been scientifically proven.
How can you prevent it?
As an effective measure, in addition to detailed information for those affected and their parents, “skills training” has proven itself: Here, the affected person exercises strategies that replace self-injurious behavior, for example the use of strong sensory stimuli such as ice cubes in the neck or on Put your wrists, bite into chili peppers, knead a hedgehog ball, drink pure lemon juice, hit the bed or pillow, take a cold shower or the like.
Distraction through intensive concentration on physical or mental activities (e.g. playing football, jogging, writing a diary or solving crossword puzzles) is also used here.
Since emotional problems are often behind auto-aggressive behavior, it is important to take preventive measures in children and adolescents at a young age. For this it is important that children strengthen their self-confidence, develop a positive body image and learn to use social media critically.
What can relatives do?
In any case, self-injurious behavior is to be seen as an emergency signal and should be taken seriously. However, it is often difficult for parents and loved ones to spot signs of self-harm. Young people are often ashamed of their behavior and do not actively seek help.
For friends and siblings of those affected, the following applies: At the first signs, do not hesitate too long, but rather talk to the parents or another adult confidant about it.
Tips for parents and caregivers
- Address the problem calmly and openly.
- Do not criticize or judge the behavior.
- Help affected children or adolescents to understand what triggers the behavior in others (e.g. worry, fear, etc.).
- Take the child's or young person's feelings seriously.
- Don't put pressure on the child if they don't want to talk about it.
- Do not issue ultimatums or prohibitions. Self-harming behavior cannot be suppressed.
- Help the child identify the problem on their own.
- Do not try too long to get the problem under control yourself, but get professional help as early as possible.