Fecal incontinence
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
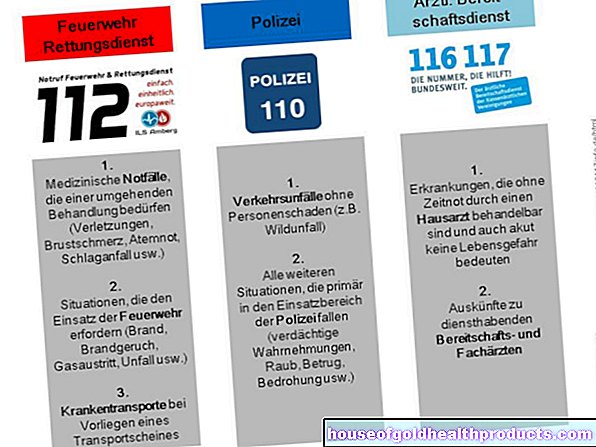
More about the experts All content is checked by medical journalists.Fecal incontinence (also bowel incontinence, anal or anorectal incontinence) is the inability to hold back stool or bowel gases or to consciously empty the bowel. Often the cause is weak sphincter or pelvic floor muscles (e.g. age-related or after childbirth). Therapy can include medication, a change in diet and pelvic floor training, and rarely an operation. Read more about this here!

Brief overview
- Causes: Declining sphincter muscles and pelvic floor muscles, triggered among other things by increasing age, diseases (e.g. stroke) or injuries (e.g. perineal tear after birth)
- Treatment: The doctor treats faecal incontinence depending on the cause. Medicines, biofeedback and physiotherapy, a change in diet or anal tampons can help. In severe cases, surgery is necessary.
- Description: In the case of fecal incontinence, those affected lose the ability to hold back their intestinal contents and intestinal gases.
- Diagnosis: Conversation with the doctor (e.g. about stool behavior), physical examinations of the sphincter muscle and the rectum (e.g. colonoscopy, ultrasound examination, anal sphincter manometry, defecography)
- Course: The prognosis is very different and depends on the cause and the age of the person affected. In many cases, the quality of life can be significantly improved with suitable therapies.
- Prevention: Strengthen the pelvic floor (e.g. through specific exercises, pelvic floor training), move regularly, eat a balanced diet rich in fiber, avoid being overweight.
What are the causes of fecal incontinence?
Defecation is a complex process that involves several areas of the bowel. The so-called continence organ "anorectum" (closing device) closes the anus. It enables the bowel movements and intestinal gases to be retained or stopped in a controlled manner (continence). The continence organ consists of the rectum (= rectum, last section of the intestine), as a reservoir for the stool, and the sphincter (= sphincter), which surrounds the anal canal.
If one or both of the components are damaged by illness, malformations or injuries in the course of life, this can lead to fecal incontinence. Intestinal incontinence, for example due to deformities, is congenital.
The most important causes of fecal incontinence at a glance:
Weak sphincter and pelvic floor muscles in old age
Sphincter weakness and sphincter defects are the most common causes of fecal incontinence and are common in the elderly. The reason for this is that with increasing age, the muscle mass and the supporting connective tissue in the pelvic floor (e.g.when the pelvic floor is lowered) and the anal area decreases (muscular fecal incontinence).
Perineal tear after childbirth
Fecal incontinence is common in women after giving birth vaginally. The sphincter muscle (perineal tear) tears, often unnoticed, during the contractions, which later leads to discomfort. Anal operations that injure the sphincter can also lead to intestinal incontinence.
Rectal prolapse
Rectal prolapse can also cause fecal incontinence. The rectum shifts from its original position and emerges from the anus (often during solid stool). Most advanced hemorrhoids (grade 3 to 4) trigger a rectal prolapse.
Neurological diseases
Regardless of age, neurological diseases such as a stroke, multiple sclerosis, Alzheimer's disease or paraplegia lead to the nerve supply to the pelvic floor muscles being disturbed. As a result, those affected often feel the urge to defecate late or not at all (neurogenic fecal incontinence). Nerve damage that leads to fecal incontinence is also possible in people with diabetes mellitus.
Another possible trigger is discomfort in the spine or when the pelvic nerves are damaged after a vaginal delivery. In some cases, pregnancy also causes the muscles of the pelvic floor to weaken. Especially in the period shortly before giving birth, some women experience an unwanted loss of gas or stool.
Diarrheal diseases
In the case of diarrheal diseases, the thin stool, even in otherwise healthy people, can overwhelm the sphincter muscle and mean that those affected cannot hold back the stool. Diarrhea is often caused by infections, food poisoning, food intolerance (e.g. lactose intolerance), and more rarely chronic bowel diseases (e.g. Crohn's disease or ulcerative colitis).
constipation
Constipation and a sluggish bowel can also lead to fecal incontinence in the long run. The stool in the intestine creates a blockage that only allows liquid stool to pass. As a result, the intestine produces more fluid and so-called overflow incontinence occurs.
The watery stool is usually difficult to control and as a result comes out in droplets. In addition, people with constipation often push too hard to empty the bowel. Under certain circumstances, this leads to the sphincter muscle being overstretched or injured, which further promotes fecal incontinence.
Intestinal narrowing due to tumor or surgery
If the bowel is narrowed by a tumor or if the rectum has been surgically reduced in size (e.g. after removal of a tumor or anal fistulas), stool incontinence can subsequently occur.
Obesity
Very overweight (obesity) favors weak pelvic floor muscles and thus, among other things, fecal incontinence.
Medication
Certain medications cause fecal incontinence in some cases. These include laxatives (e.g. paraffin), antidepressants and drugs against Parkinson's disease.
Mental disorders
In rare cases, mental disorders are the cause of fecal incontinence, for example when sufferers relapse into infantile behavior due to trauma and thereby lose the ability to consciously defecate.
What can be done about faecal incontinence?
The doctor treats faecal incontinence depending on the cause. Initially, he usually relies on non-operative (conservative) therapies. For example, medication, pelvic floor training, biofeedback or a change in diet can be considered. In most cases, these measures already bring good results.
If underlying diseases, such as chronic inflammatory bowel disease, are the cause of the symptoms, the doctor first treats them in order to then treat damage to the sphincter muscle.
In severe cases of fecal incontinence or if non-operative measures do not bring the desired result, an operation is necessary.
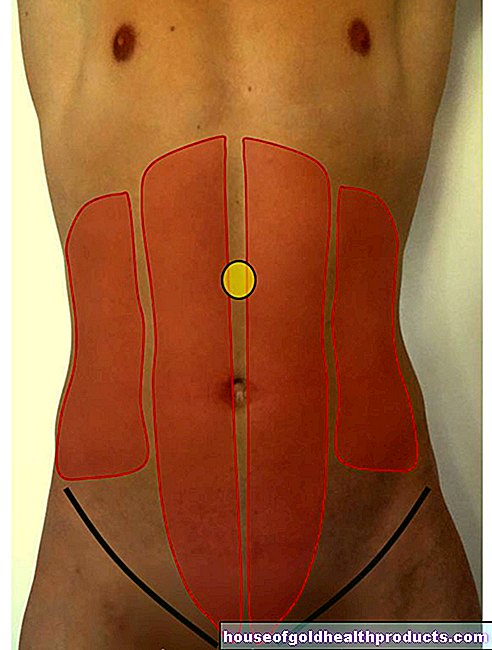
Pelvic floor training
Strengthening the pelvic floor muscles is an essential prerequisite for counteracting faecal incontinence. Pelvic floor exercises (= sphincter training) specifically strengthen the muscles in the anal and pelvic areas. Pelvic floor exercises are particularly effective for people with weak connective tissue and for women who have had multiple births. Doctors recommend doing the training under the guidance of specialized physical therapists.
Exercises for fecal incontinence
Targeted exercises help to strengthen your pelvic floor and sphincter muscles. In this way, you can improve your wind and stool control and prevent fecal incontinence.
Exercise in the supine position
- Lie on your back on a flat surface.
- Extend your legs parallel and tense your buttocks together with your sphincter muscle (pinch!).
- Hold the tension for three seconds as you exhale, then relax as you inhale.
- Repeat the exercise once with your legs stretched out and crossed and once with your legs upright (knees bent, feet on the floor).
Exercise while sitting
- Sit in a chair.
- Tilt your upper body slightly forward.
- Place both legs next to each other and do the first exercise (lying on your back) while sitting.
- Now press both heels together and at the same time push your knees apart.
- Tense your glutes while doing this.
Exercise in the prone position
- Lie on your prone position on a flat surface.
- Press your heels together while pushing your knees apart.
- Tense your glutes while doing this.
Exercise while standing
- Stand up straight.
- Tense your sphincter muscle together with your glutes.
- Hold the tension for three seconds as you exhale, then relax as you inhale.
- Repeat the exercise as you walk.
Exercise in everyday life
- In everyday life (e.g. when waiting at the red light, when brushing your teeth in the morning, when driving a car, in the office), try again and again to tense your buttocks and your sphincter muscles for a few seconds. Keep the tension as long as possible.
It is best to do these exercises regularly (about ten repetitions per exercise twice a day).
nourishment
In order to treat intestinal incontinence, so-called stool regulation is important. This means that, in the best case scenario, the stool should not be too firm or too soft, and that stool should be taken off regularly. Doctors therefore recommend eating a balanced diet rich in fiber (e.g. vegetables, fruit, cereals, legumes) and drinking enough fluids (at least two liters per day).
Swelling foods, such as psyllium soaked in water, also ensure that stool volume increases, which normalizes stool consistency. Rice, a grated apple, or mashed bananas also help the intestines regulate bowel movements.
However, people with fecal incontinence should avoid foods that irritate the intestines, such as coffee, alcohol and flatulent foods (e.g. beans, cabbage, carbonated drinks).
Keeping a stool diary can help you get a better sense of which foods and habits are promoting your continence or making your symptoms worse.
Correct stool behavior
When going to the toilet, it is important to watch out for correct stool behavior. Please note the following:
- Only go to the bathroom if you have an urge to defecate.
- Do not push too hard during bowel movements.
- Do not sit on the toilet for too long (no more than three minutes, no reading the newspaper)
Aids
There is now a large number of products on the market that are available to people with faecal incontinence. Aids such as adult diapers, pads or anal tampons give people with faecal incontinence back some of their quality of life and enable them to lead an almost normal life.
Biofeedback
In order to better perceive the pelvic floor and the sphincter tension itself, the use of biofeedback can also help. To do this, the doctor places a small balloon over a probe in the anal canal, which the patient has to squeeze specifically with his sphincter muscles.
A device uses optical or acoustic signals to indicate when the person concerned squeezes the ball. It also shows how strong the contraction of the anal muscles is. The biofeedback training follows an individually defined exercise plan that the doctor works out. Usually only a few sessions (around six to ten) are necessary to reactivate the pelvic floor, and those affected then continue training (without a device) at home.
Electrical stimulation
Electrostimulation also helps those affected to improve the function of their sphincters. To do this, the doctor supplies the patient with a weak current (stimulation current) via electrodes, which causes the sphincter muscle to contract passively. In order for therapy to be successful, it is necessary to conduct it regularly. The first effects are usually only noticeable after a few weeks.
In the case of inflammation of the rectum, the use of biofeedback and electrical stimulation is not recommended, as this also irritates the intestinal wall.
Medication
Various medications can be used to treat faecal incontinence. Depending on which effect is desired, the doctor can either prescribe laxatives (laxatives) or drugs that inhibit bowel movements (motility inhibitors).
To prevent a sudden loss of stool, he prescribes laxatives that stimulate the colon to pass stool. In addition, mild purgative cones or enemas (enemas) can be used to specifically empty the bowel at a desired time.
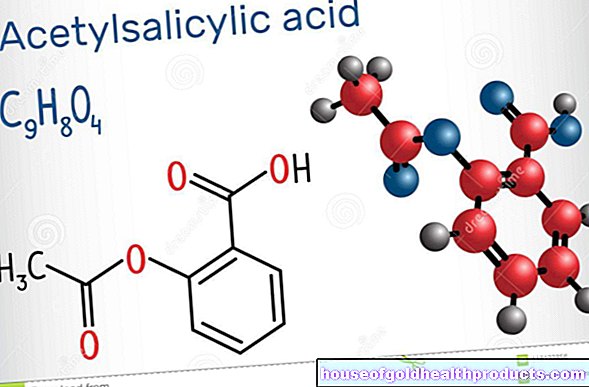
Motility inhibitors such as the active ingredient loperamide slow down the transport of food through the intestines. The stool thickens and the person has to go to the bathroom less often.
Do not take medication for faecal incontinence on your own, but only after consulting your doctor! The uncontrolled use of laxatives and motility inhibitors can upset your bowel movements and make the symptoms worse.
surgery
Operations in the pelvic floor area should ideally be carried out by a specialist doctor (proctologist) in a surgical center specializing in this area.
Sphincter surgery
The most common method used for fecal incontinence is surgery, during which the doctor restores the sphincter muscles as well as possible. To do this, the doctor sews the sphincter back together after injuries or tears. He performs the operation through the anus, i.e. without an abdominal incision, and is therefore not very stressful for the patient.
If the sphincter is badly damaged, the doctor often replaces it with an implant made by the body (usually a muscle from the thigh), also known as a gracilis plastic. In some cases, the doctor uses an alien artificial sphincter or a plastic anal strap.
Intestinal pacemaker (sacral nerve stimulation)
A newer therapy for faecal incontinence is the so-called sacral nerve stimulation or neuromodulation (SNM). It follows the principle of the pacemaker. To do this, the doctor implants a thin electrode in the patient's sacrum. A pacemaker, which is also located under the skin, emits light electrical impulses there, which stimulate the nerves in the rectum and increase muscle function.
The method is particularly suitable for people whose faecal incontinence is caused by a neurological disorder. The procedure under anesthesia takes about 40 minutes, usually a short inpatient stay in the hospital is necessary.
Prolapse surgery
In the case of a rectal prolapse, the doctor fixes the rectum to the sacrum in the small pelvis with a plastic net. The doctor usually performs this operation as part of a laparoscopy over the abdominal wall with an endoscope. This is also a small procedure that does not require a large abdominal incision.
The procedure is usually followed by a four to five day hospital stay.
Syringes with "Bulking Agents"
In some cases the doctor injects substances called "bulking agents" under the skin of the anal canal. These are substances such as Teflon particles, collagen, silicone or bioglass. They remain in the tissue and narrow the anal canal. This can usually be done on an outpatient basis and is usually painless for the person concerned.
However, the effect of the bulking agents often only lasts for a short time and has to be repeated. Since allergic reactions to the substances are also possible, this therapy is only carried out in exceptional cases in the case of fecal incontinence.
Artificial anus
If all treatment options fail, the doctor seldom creates an artificial anus (stoma), which he then reoperates if necessary. The doctor connects part of the colon with the abdominal wall. This creates an opening to which a pouch for defecation is attached. However, this procedure should only take place after careful consideration.
For a sustainable treatment, non-surgical support measures are usually necessary after an operation.
What is fecal incontinence?
According to the definition of the World Health Organization (WHO), stool continence is the learned ability to “deliberately stop defecating at the right time and place”. Accordingly, people with fecal incontinence (including bowel incontinence, anal incontinence, anorectal incontinence or fecal incontinence) are no longer able to consciously hold back their bowel movements. Liquid or solid stool as well as intestinal gases (flatulence, winds) escape in an uncontrolled manner, without the person concerned being able to do anything about it.
Faecal incontinence is not an independent disease, but occurs as a symptom of various diseases. Depending on the severity, it can be divided into three degrees of severity:
Grade 1: The underwear is often soiled and intestinal gases escape uncontrollably.
Grade 2: The underwear is often soiled, intestinal gases escape uncontrollably and the person concerned loses liquid stool.
Grade 3: The person concerned no longer has control over when and where he deposits liquid and solid stool and lets intestinal gases escape.
Who is particularly affected?
In general, faecal incontinence can affect people of all ages. Around one to three percent of the population suffer from faecal incontinence worldwide. Around 800,000 people are affected in Germany. The number of people affected is considerably higher in older people than in younger people.
According to the German Continence Society, intestinal incontinence is four to five times more common in women than in men. The reason for this is the different anatomical conditions in the pelvic area of men and women. In addition, pregnancies and childbirths favor the development of faecal incontinence in women.
Mental stress in fecal incontinence
People with fecal incontinence usually have a very high level of psychological distress, as the time at which the stool will be lost cannot be foreseen. This is often associated with shame and great psychological stress for those affected. Because of their fear of getting into an uncomfortable situation in public, people with incontinent stools often withdraw.
They prefer to stay at home, turn down invitations, do not go to events or restaurants and do not communicate out of shame in those around them (e.g. family, friends). They usually suffer severely from social isolation.
People with faecal incontinence often do not dare to discuss their problem with their doctor. Help from the doctor and various therapies as well as numerous aids are definitely available. In many cases, faecal incontinence is easy to treat, which usually enables those affected to have a normal everyday life despite intestinal incontinence.
If you suspect that you have fecal incontinence yourself or that a relative of yours is affected, do not hesitate to talk to a doctor.
How does the doctor make a diagnosis?
It is important to consult a doctor at an early stage if the first long-lasting difficulties with stool control (e.g. if flatulence escapes unintentionally).
Which doctor is eligible for diagnosis varies depending on the cause. This can either be the family doctor, a gynecologist, a urologist or a rectal specialist (proctologist). The following applies: the sooner you contact a doctor, the faster he can help you and, in the best case, resolve the symptoms.
Talk to the doctor
First, the doctor has a detailed discussion with the person concerned and collects the medical history. To do this, he asks questions about the symptoms and stool behavior.
Doctors recommend keeping a diary of toilet habits about two weeks before the doctor's appointment:
- How many times a day do you have a bowel movement?
- How often do you have to hurry to get to the toilet on time?
- How often do you have uncontrolled defecation because you couldn't postpone it long enough?
- How often does stool pass uncontrollably without you feeling it?
- Do you wear pads / diapers?
- Are your underwear or pads dirty?
- Does your faecal incontinence prevent you from doing normal everyday activities, such as leaving your home or going shopping?
- What is the consistency of your stool? Predominantly firm, soft, liquid?
An open discussion with the doctor is the first step in finding the cause of the symptoms and is an essential part of finding the right treatment.
The way to clarification often takes a long time. Many of those affected refuse to talk about the topic out of shame and fear. But don't be afraid to confide in your doctor. He is there to help you and improve your quality of life with appropriate treatment.
Physical examination
A physical exam will follow. To do this, the doctor uses a stethoscope to listen to the stomach for unusual intestinal noises. He also inspects the anal area to rule out possible skin changes, fissures, scars, hemorrhoids or fistulas.
In order to assess the sphincter muscle and the rectum, the doctor gently palpates them. In doing so, he determines, among other things, how strong the internal tension of the sphincter muscle is at rest and when consciously squeezing together. If necessary, the doctor determines whether polyps or tumors are present by palpation.
Further investigations
The doctor then does a rectoscopy (reflection of the rectum) and colonoscopy (reflection of the large intestine). Among other things, he rules out tumors as a (rare) cause of fecal incontinence.
Further examinations will follow to assess the function of the sphincter muscle. With the so-called sphincter manometry (anorectal manometry), the doctor uses a small probe (measuring catheter) to measure the pressure values in the anal canal. An anal examination with ultrasound (endosonography) also gives the doctor information as to whether there are injuries to the sphincter, such as those that occur after childbirth or surgery.
With the help of a defecography, it is possible to assess the mobility of the pelvic floor and to identify bulges in the rectum. To do this, the doctor gives the patient radiopaque contrast agent through the anus, which makes the functional processes of bowel evacuation visible on a video x-ray film during the next bowel movement.
If necessary, the doctor uses imaging methods such as computed tomography (CT) or magnetic resonance tomography (MRT) to produce sectional images of the sphincter muscle and the pelvic floor.
Is Fecal Incontinence Curable?
The prognosis for faecal incontinence varies from person to person. Both the cause and the age of the person affected influence the course. Appropriate therapies, however, often alleviate the symptoms and significantly improve the quality of life. However, it is not always possible to fully restore stool control.
How do you prevent fecal incontinence?
It is not always possible to specifically prevent fecal incontinence. However, there are a few steps you can take to significantly reduce your risk:
- Exercise regularly.
- Strengthen your pelvic floor muscles (e.g. through pelvic floor training or specific exercises).
- Avoid trans
- Eat a balanced diet rich in fiber (e.g. vegetables, fruits, cereals, legumes).
- Avoid foods that cause gas (e.g. beans, cabbage, carbonated drinks).
- Drink enough (at least two liters of fluids per day).
- Make sure you have regular bowel movements.