Ablation on the heart
Valeria Dahm is a freelance writer in the medical department. She studied medicine at the Technical University of Munich. It is particularly important to her to give the curious reader an insight into the exciting subject area of medicine and at the same time to maintain the content.
More about the experts All content is checked by medical journalists.Ablation on the heart is an operation in which excess or diseased pathways and excitation foci are desolated. As a result, certain types of cardiac arrhythmias can be permanently eliminated, especially if medication does not help (anymore). Read everything about the areas of application, procedure and risks of this therapy!

What is an ablation?
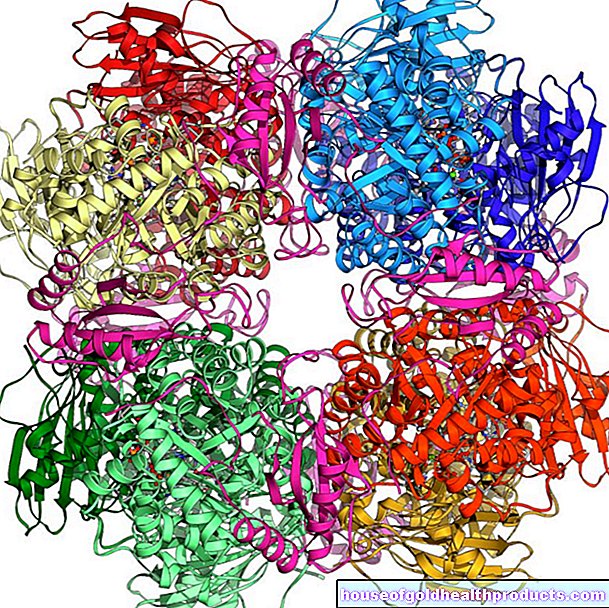
During ablation on the heart, the effects of heat or cold, rarely also ultrasound or laser, are used to cause targeted scars in those cells of the heart muscle that generate or conduct the electrical excitation incorrectly. In this way, muscle excitations can be suppressed that disrupt the normal heart rhythm - the heart beats normally again.
This procedure is almost always performed using a catheter that is advanced to the heart through a blood vessel in the groin. The procedure is therefore also called "catheter ablation". An electrophysiological examination (EPU) usually precedes ablation on the heart. Sometimes doctors combine ablation on the heart with necessary surgery (then called surgical ablation).
The standard procedure is radiofrequency ablation (high frequency ablation), in which the tip of the catheter gives off intense heat generated by electromagnetic waves to the tissue. Another procedure is cryoablation, which uses cold. During the ablation, parts of the excitation conduction system are interrupted. As a result, the heart ideally no longer generates or forwards any pathological impulses and beats regularly again.
Cardiac arrhythmias
The conduction system in the heart determines the heart rhythm. The main impulse comes from the sinus node, which is located in the wall of the right atrium. From there, the electrical excitation travels through the atria, then - as a switching point between the atria and ventricles - via the AV node and the bundle of His into the ventricular limbs (Tawara thighs) and finally into the Purkinje fibers. They excite the heart muscle from the tip and thus trigger its contraction.
If the flow of electrical signals is misdirected or additional impulses arise in the heart wall, the heart rhythm is disturbed. The heart muscle then works uncoordinated and the blood is less effective or - in the worst case - no longer pumped into the bloodstream at all.
When to do a heart ablation?
Catheter ablation is used for certain cardiac arrhythmias, especially when these do not improve significantly despite drug therapy. Major conditions for which doctors perform heart ablation include:
Atrial fibrillation
With atrial fibrillation, the atrium is excited irregularly by circular or disordered impulses. Some of the impulses are passed on to the chambers, which therefore contract irregularly and often in too rapid succession (tachyarrhythmia). This becomes noticeable through complaints such as a drop in performance, palpitations, dizziness, shortness of breath, chest pain or feelings of fear. In addition, the disturbed blood circulation can cause blood clots to form, especially in the atrium, which - if they loosen - can trigger a stroke, for example.
The success of cardiac ablation in atrial fibrillation varies by definition. About 45-65 percent of patients have no recurrence of atrial fibrillation for five years after this treatment. As an alternative to medication, according to currently valid guidelines, ablation on the heart is the therapy of first choice for patients with seizure-like atrial fibrillation and corresponding symptoms - provided the patient does not suffer from any relevant cardiac or serious pre-existing disease.
Atrial flutter
Atrial flutter essentially corresponds to atrial fibrillation. One difference, however, is that the atrium contracts with frequencies of more than 250 to 450 beats per minute, while with atrial fibrillation it can be 350 to 600 beats. In addition, the atrial flutter is regular.
Atrial tachycardia (atrial tachycardia)
The electrical impulses do not come from the sinus node, but from other locations in the wall of the right atrium. In contrast to atrial fibrillation, the atrial actions are regular and typically beat at a rate of 160 to 220 beats per minute. The more places the impulses trigger, the less successful the ablation on the heart is in this disease.
Wolff-Parkinson-White syndrome (WPW syndrome)
The WPW syndrome is one of the AV reentry tachycardias (AVRT). In addition to the normal pathway between atrium and ventricle, there is an additional (accessory) pathway in this disorder, which represents a "short circuit" to the heart muscle. This leads - usually in attacks - to the fact that the impulses reach the heart chambers faster and these then contract faster (heart rate around 150-220 beats per minute). Ablation on the heart is particularly useful if these cardiac arrhythmias occur frequently. The success rate is high (over 90 percent).
AV nodal reentry tachycardia
In the AVNRT, electrical impulses circulate in the AV node (this has two lines here). This leads to a sudden rapid heartbeat that can last for minutes to hours and lead to dizziness and fainting spells. In the case of an EPU, the doctor looks for the slower of the two conduction pathways and obliterates it.
Ablation on the heart is also used for other arrhythmias such as tachycardiac arrhythmias in the ventricles.
What do you do about heart ablation?
Ablation on the heart is a minimally invasive procedure. This means that the therapy only causes the smallest injuries to the skin and soft tissues. As with any surgery, some standard tests, such as an EKG and blood draw, will be done beforehand. In addition, there is in-depth personal advice and information from the attending doctor.
An electrophysiological examination (EPU) is carried out before the actual ablation. It helps the specialist to precisely determine the arrhythmia and its origin.
After a local anesthetic, the doctor usually punctures a vein in the groin and creates a so-called “sluice” there. Like a valve, this prevents blood from escaping from the vessel and at the same time enables the catheter or other instruments to be inserted into the bloodstream.
The doctor then pushes thin electrode catheters through the sluice to the point where the large vena cava flows into the right atrium. This process is hardly noticeable for the patient.
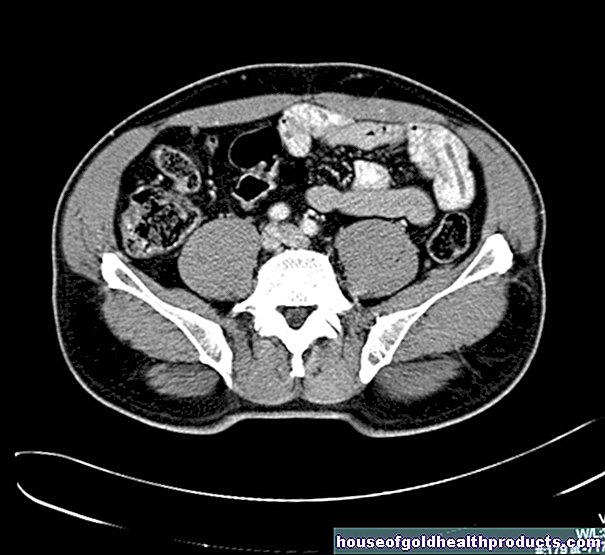
With the help of X-rays and an evaluation of the electrical signals from the catheters, their position is determined. The electrical signals that trigger the cardiac arrhythmia can now be registered at various points in the heart. The doctor may also use electrical impulses to track down the origin of a seizure-like cardiac arrhythmia.
For ablation on the heart, the doctor now inserts an ablation catheter in order to obliterate the source of the interference signals or defective lines. A type of high-frequency current is used in radiofrequency ablation.
To monitor success, the heart is now specifically stimulated, or certain drugs are given that can trigger a cardiac arrhythmia. If no disturbance occurs, the ablation can be terminated. The catheters are removed and the venous puncture site is closed with a pressure bandage.
Ablation in atrial fibrillation is a special case, as there is no clear place of origin for this arrhythmia. One suspects this predominantly at the point where the four pulmonary veins enter the heart. Therefore, with the so-called pulmonary vein isolation, ring-shaped scar areas are created around the entry points, which separate the electrical connection to the left atrium.
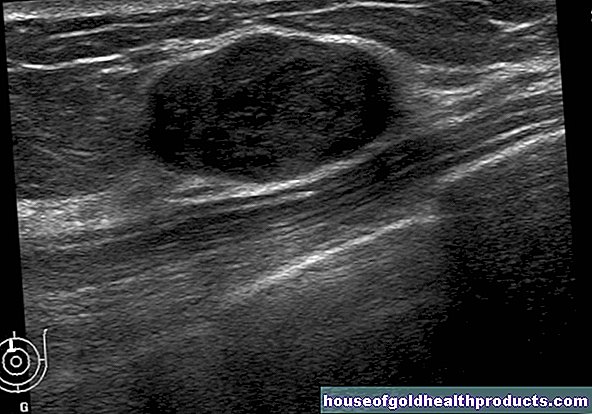
Following the ablation on the heart, the heart's activity is documented by EKG, blood pressure measurements and an ultrasound examination. The patient can leave the hospital after approximately 24 hours.
What are the risks of heart ablation?
In addition to the general risks of any procedure, such as bleeding and infection, specific complications can arise as part of an ablation of the heart. However, these are rare, as catheter ablation is a fundamentally gentle procedure:
- Pericardial effusion (pericardial effusion to pericardial tamponade) - a tear in the muscle causes bleeding into the space between the heart and the pericardium
- Destruction of the excitation conduction system - this must then be treated with a pacemaker
- Blood clot formation (thrombosis)
- Narrowing / occlusion of the pulmonary veins
- Injury to the surrounding structures and organs
- Bruising or bleeding at the puncture site
- Vascular occlusions
What should I watch out for after an ablation?
For about two weeks after the ablation, you should avoid strenuous exercise and exercise to avoid rebleeding. Do not press hard when you have a bowel movement. The arrhythmia treatment drugs that were needed before the operation are usually taken for an additional three months. In addition, therapy to inhibit blood clotting is necessary for at least 8-12 weeks, as otherwise blood clots could form in the scarring areas.
Through intensive observation with resting ECGs, long-term ECGs and ultrasound examinations, the doctor can reliably identify possible complications and the success of the ablation. If the arrhythmia occurs again, another ablation on the heart can be useful.
Tags: dental care nourishment elderly care















.jpg)