Von Willebrand Syndrome
All content is checked by medical journalists.Von Willebrand syndrome (VWS) is a bleeding disorder that is mostly inherited. In rare cases, other diseases or certain medications are the cause. Those affected form too little of the Von Willebrand factor (VWF), which is important for hemostasis, or a defective form of the protein. Typical symptoms are heavy menstrual bleeding, bleeding from the gums and nose, and bleeding after surgery. Read more about diagnosis and treatment here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D68
Brief overview
- Description: Mostly hereditary, rarely acquired bleeding disorder that leads to an increased tendency to bleed
- Prognosis: With appropriate treatment, life expectancy is not affected.
- Treatment: Treatable with medication, not curable in the inherited form
- Symptoms: Bleeding especially of the mucous membranes: heavy menstruation, nosebleeds, bleeding gums, bleeding after operations, iron deficiency
- Prevention: information and clarification of the personal environment; Carrying an emergency ID card; Avoiding certain medications
- Diagnosis: Based on symptoms, family history, blood tests
- Causes: Mostly inherited, rarely caused by other diseases or drugs
What is Von Willebrand Syndrome?
Von Willebrand Syndrome (VWS) is the most common congenital hemostasis disorder worldwide: around one in 1,000 people develop it. An older name of the VWS is "Von Willebrand-Jürgens Syndrome".
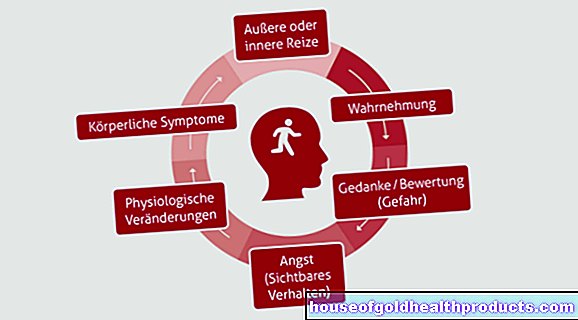
Those affected are more prone to bleeding. The reason is a coagulation disorder. In rare cases, the disease is not inherited but is caused by other underlying diseases (e.g. heart defects, hypothyroidism) or certain medications.
Whether and how much bleeding occurs depends on the type of disease. VWS is weak in some people and hardly any or no symptoms develop. Doctors usually diagnose women earlier than men because of menstrual bleeding or postpartum bleeding. There are three types of VWS:
Types 1 to 3 of Von Willebrand syndrome
Doctors divide Von Willebrand syndrome into three types. Knowing what form of the disease is is important for treatment. In some cases, however, Von Willebrand syndrome cannot be clearly assigned to one type.
Von Willebrand syndrome type 1
Von Willebrand syndrome type 1 has a deficiency of the so-called Von Willebrand factor. Type 1 is the most common form and accounts for about 85 percent of all cases of Von Willebrand syndrome.
The Von Willebrand factor, in conjunction with other substances, ensures that the blood platelets (thrombocytes) stick together, the injury or wound stick together and thus stop the bleeding. Its second task is to protect another important coagulation factor, so-called factor VIII, from being broken down by enzymes. Doctors count type 1 among the quantitative disorders of hemostasis.
Von Willebrand syndrome type 2
In Von Willebrand syndrome type 2, the body produces a defective form of the Von Willebrand factor. As a result, he can only take over his task to a limited extent or not at all. Doctors call this a qualitative hemostasis disorder.
Von Willebrand syndrome type 3
The most severe form of Von Willebrand syndrome is type 3. But it is also the rarest: around one in a million people develop this form. The Von Willebrand factor is completely absent here. Those affected have to replace the Von Willebrand factor with a drug that takes on its function. The symptoms are also most pronounced here. Like type 1, type 3 is one of the quantitative disorders of hemostasis.
Origin of the disease name
The names “Von Willebrand Syndrome” or “Von Willebrand-Jürgens Syndrome” go back to the discoverers of the disease. The Finnish doctor Erik Adolf von Willebrand first described the disease in the 1920s. He realized that, in contrast to hemophilia, Von Willebrand syndrome also affected women. In the 1930s, the German doctor Rudolf Jürgens added further observations to the description of the disease, which is why the bleeding disorder is referred to in parts of the specialist literature as Von Willebrand-Jürgens syndrome.
What is the life expectancy with Von Willebrand Syndrome?
The aim of therapy is to consistently prevent heavy bleeding and to prepare accordingly for risky situations such as surgery or childbirth. Depending on the form and severity of Von Willebrand syndrome, life expectancy is not limited with the right treatment.
If the VWS is pronounced, the quality of life of those affected is often limited. You are at a very high risk of bleeding. For example, affected women can develop very heavy menstrual bleeding. In the rare case of type 3 VWS, those affected have to take medication for life.
How is Von Willebrand Syndrome treated?
Therapy is always necessary if the risk of bleeding increases in certain situations, for example if an operation is imminent. Even if the affected person has the severe but rarely occurring form of Von Willebrand syndrome type 3, lifelong treatment is necessary. The therapy also helps to improve the quality of life.
The doctor uses various drugs for the treatment. The choice of active ingredient depends on the type of VWS. The use of so-called antifibrinolytics is possible with all forms. They strengthen blood clotting and are mainly used for bleeding from the mucous membranes. The replacement of the missing coagulation factor in the form of a drug is also a treatment option. With type 1, it is often sufficient to increase the body's own release of the Von Willebrand factor with a certain active ingredient.
Pregnancy in Von Willebrand Syndrome
In principle, pregnancy is also possible in women who have Von Willebrand syndrome. It is important that if you want to have children, you should talk to your gynecologist and get advice.
If there is a severe form of Von Willebrand syndrome, it is necessary to inform the treating physician (hematologist) about the desire to have children or the pregnancy. The same applies if the child's father is affected by the inherited form of Von Willebrand syndrome, as he may also pass the disease on to his children.
Regular examinations are even more important during pregnancy. The doctor especially conducts informational discussions before examinations that are associated with an increased risk of bleeding, for example in the run-up to an amniotic fluid test. If necessary, a specialist in high-risk pregnancies will be called in.
As a rule, in the third trimester of pregnancy, the doctor examines the blood values of the Von Willebrand factor and the coagulation factor VIII in order to prepare the birth accordingly. Since childbirth is almost always associated with pain, it is also important to clarify in advance which painkillers can be used that do not increase the risk of bleeding.
A natural birth without a caesarean section is more advantageous. But even babies born vaginally have bleeding. If these are too strong, the treating doctors may initiate therapy to stop the bleeding.
Menstruation in Von Willebrand Syndrome
Women are more likely to develop VWS symptoms than men when they have Von Willebrand syndrome. Because menstruation, pregnancy and childbirth are associated with a significantly increased risk of bleeding. Heavy menstrual bleeding is most common in women with Von Willebrand syndrome.
In order to determine how much blood actually escapes during the menstrual period, gynecologists often ask how often hygiene items have to be changed each day and how many days the menstruation lasts. It is also important to inform the doctor about any other bleeding symptoms. These include nosebleeds, bruises or heavy / prolonged bleeding after, for example, dental surgery or childbirth.
If Von Willebrand syndrome is present and the menstrual bleeding increases, the doctor usually first prescribes the pill, i.e. a hormone preparation, to control the bleeding. If that is not enough, other preparations are used as an alternative or in addition to the therapy of Von Willebrand syndrome, which strengthen blood clotting.
Which drugs are prohibited in Von Willebrand syndrome?
Some medications must be avoided at all costs in Von Willebrand syndrome. These include in particular pain relievers with the active ingredient acetylsalicylic acid. Always seek advice from your doctor and pharmacist before taking any medication. It is also advisable to read the package insert carefully before taking it for the first time. There you will find information on active ingredients, contraindications and how to take them, among other things.
Acetylsalicylic acid is also contained in many over-the-counter products! Ask a pharmacist if you are unsure.
Before operations, it is particularly important to discuss the use of painkillers with the attending physician. It has been clarified in advance which pain relievers may and may not take.
What are the symptoms of Von Willebrand Syndrome?
Those affected by Von Willebrand syndrome develop faster and heavier bleeding, especially bleeding from the mucous membranes. They usually show up as:
- Nosebleeds
- Bleeding gums
- Menstrual bleeding
- Bleeding in the gastrointestinal area: Depending on the location of the bleeding, fresh blood appears in or on the stool and the stool is black (tarry stool).
- Blood in the urine (dark / red color of urine)
In addition, bleeding after surgery - especially in the teeth, tonsils or the nose / sinuses - suggests Von Willebrand syndrome. Spontaneous bleeding into muscles or joints can occur in the rare type 3 of Von Willebrand syndrome.
Because of the more frequent and heavy bleeding, people are often pale and tired. The corners of the mouth are often torn. In addition, those affected usually suffer from difficulty concentrating. Doctors then often use a simple blood test to determine an iron deficiency and anemia.
Precautions for Von Willebrand Syndrome
As soon as you know that Von Willebrand syndrome affects you or your child, there are several recommendations to heed. They can help prevent bleeding and help if it does.
Sports: Is generally allowed, but make sure that these are sports that are associated with a lower risk of injury, such as swimming, gymnastics, hiking.
Basics for an emergency: If you have injured yourself, it is advisable that you:
- immobilize the affected body region,
- cool,
- elevate,
- apply a pressure bandage if you have a bleeding
- and if necessary, consult a doctor.
Informing others: Regardless of whether it is your partner doing sports, your colleague at work or your partner - inform those around you about your illness. If you have any medication that your doctor has prescribed for you in an emergency, you should carry it with you and tell others about it. Help is quickly organized in an emergency and important information is passed on directly.
It is advisable to have an emergency ID card with you with the information about Von Willebrand syndrome. Make sure you have an international emergency ID (also in English) with you when traveling.
How is Von Willebrand Syndrome diagnosed?
It often takes many years for a doctor to diagnose Von Willebrand syndrome. In women, it is an average of 16 years from the onset of the first bleeding symptoms to the diagnosis of VWS. Often it is hematologists, i.e. doctors who specialize in blood disorders, but also internists, general practitioners or gynecologists who diagnose the disease.
A detailed medical history is important for the diagnosis of Von Willebrand syndrome. The doctor will ask for specific symptoms of the disease in order to recognize the disease in you or your child. He will also ask if there are clusters in the family. In addition to the detailed discussion, the doctor checks the blood for its natural clotting function.
To determine the exact type of Von Willebrand syndrome, he will perform special genetic tests.
What causes Von Willebrand Syndrome?
In the vast majority of cases, the cause of Von Willebrand syndrome is congenital. It goes back to a genetic mutation that at least one parent passed on. In rare cases, Von Willebrand syndrome is caused by other diseases or certain medications.
How is Von Willebrand Syndrome inherited?
Types 1, 2A, 2B and 2M are inherited dominantly. This means that it is sufficient if only father OR only mother is affected by Von Willebrand syndrome for the disease to be passed on to the child. Type 3 and type 2N are inherited recessively. Father AND mother both have to carry Von Willebrand syndrome in order for the child to develop it. If only one parent is a carrier of type 3 or type 2N von Willebrand syndrome, the child will not develop it, but it is a carrier and may in turn pass it on to their children.
Non-congenital, acquired Von Willebrand syndrome
In children, acquired Von Willebrand syndrome occurs, for example, with heart defects. In adults, it can develop as part of various diseases, such as:
- Heart disease
- Myeloproliferative neoplasms (MPN), rare, malignant diseases of the bone marrow
- Autoimmune diseases such as underactive thyroid gland (hypothyroidism)
Certain drugs such as the active ingredients valproic acid (e.g. used in epilepsy) and ciprofloxacin (an antibiotic) also cause Von Willebrand syndrome in rare cases.
In the case of acquired VWS, the therapy is based on the underlying cause. If this is treated successfully, the symptoms of Von Willebrand syndrome also subside.
Tags: anatomy diet laboratory values

.jpg)