Dialysis: nutrition
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Diet plays an important role in dialysis. But there is no single diet that is suitable for all dialysis patients. A dialysis team works out the optimal menu for each patient. If necessary, it is constantly adapted to current changes in the state of health. It is also important that dialysis patients and possibly their relatives receive extensive training from dieticians. Read more about diet during dialysis.

General diet regulations
Even before the start of dialysis, a patient with kidney weakness is often confronted with dietary requirements. In this phase, doctors often recommend drinking a large amount and a low-protein diet. The recommendations for patients on dialysis are often exactly the opposite: a diet high in protein and limited fluid intake are now necessary. Before and during dialysis, patients should eat a diet low in phosphate, low in potassium and low in salt. For this, the patients need the appropriate tools: In addition to a food table, dialysis patients need personal and food scales.
High protein diet
During dialysis, amino acids (building blocks of proteins) are lost. In addition, more proteins are broken down (catabolic metabolism). Dialysis patients should therefore eat a diet rich in protein: A daily intake of 1.2 to 1.5 grams of protein per kilogram of body weight is recommended.
With a sufficient supply of energy (2100 to 2500 kcal per day with a body weight of 75 kg), an increased breakdown of protein can also be counteracted. The proportion of fats as an energy source should be around 35 percent, carbohydrates should make up around 50 percent and proteins around 10 to 15 percent.
Low-phosphate diet
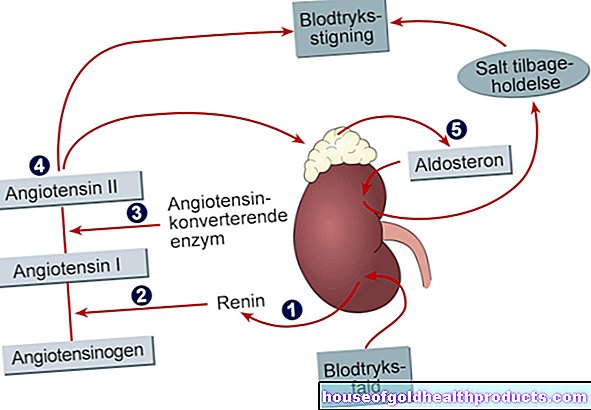
Due to the weak kidneys, the phosphate levels in the blood rise. This hyperphosphataemia leads to bone changes, vascular damage and overactive parathyroid glands in the long term. Therefore, dialysis patients should consume as little phosphate as possible. The problem with this is that the intake of phosphate is closely related to the intake of protein, which means that protein-rich foods often also contain a lot of phosphate. However, since dialysis patients should eat a diet rich in protein, the phosphate intake can only be reduced to a limited extent. In addition, dialysis patients must therefore take phosphate-binding medication (e.g. the active ingredient sevelamer) with meals.
Dialysis patients should avoid foods that are particularly rich in phosphate. These include, for example, nuts, muesli, offal, egg yolks, legumes and whole grain bread. Even foods that contain phosphate for production reasons are rather taboo. Examples are processed cheese, cooked cheese, canned milk and some types of sausage. You may want to ask about the phosphate content when buying sausage products in the butcher's shop.
Drinking milk and condensed milk can be replaced by cream, whereby the cream is diluted with water depending on the purpose.
Low potassium diet
The decrease in urine output as a result of the weak kidneys leads to an increase in the potassium level in the blood. This hyperkalemia can lead to severe cardiac arrhythmias up to and including death from cardiac arrest. Dialysis patients therefore have to keep an eye on their potassium intake: it can be reduced through a targeted selection of foods and the appropriate preparation of the dishes.
Food selection:
The following foods contain a particularly high amount of potassium and should be avoided during dialysis treatment:
- Nuts,
- Muesli, oatmeal,
- Dried fruit,
- Vegetable and fruit juices, bananas, apricots,
- improperly prepared potatoes or vegetables,
- fresh or dried mushrooms,
- Ready-made potato products (mashed potatoes, potato dumplings, potato chips).
Canned fruits and vegetables provide half as much potassium as corresponding fresh produce. Likewise, the potassium content of frozen food is much lower than that of fresh food. However, the water that accumulates when the frozen products are thawed is very rich in potassium and should therefore not be used for cooking.
Dialysis patients should expressly forego diet salts, which often contain very high amounts of potassium.
Preparation of the dishes:
The potassium content of food can be reduced through a suitable preparation, such as "watering". Potatoes or vegetables are cut into small pieces and placed in ten times the amount of water overnight or the (warm) water is changed several times. You should also cook with plenty of water and throw away the cooking water later. In this way, the potassium content in vegetables can be reduced by up to 75 percent.
Low salt diet
In dialysis patients, it is often necessary to limit the salt intake. Table salt is the chemical compound sodium chloride (NaCl). An increased salt content in the blood leads to increased blood pressure, accumulation of excess fluid in tissues and an increased feeling of thirst. If dialysis patients subsequently increase the amount they drink, overhydration can occur.
In terms of a low-salt diet, it is better to use herbs and spices (in moderation) instead of salt when cooking. As a rule, do not add salt to food at the table.
In addition, avoid highly salted foods during dialysis treatment. These include pretzel sticks, pretzels, pickled cucumbers, smoked and cured meat and fish products (raw ham, sausage, anchovies, salted herrings, etc.), ready-made meals, ready-made soups, stock cubes, ready-made sauces and ketchup.
Fluid intake and amount of water to drink during dialysis therapy
Dialysis doctors determine the daily amount of water to drink for dialysis patients on an individual basis. As a rule of thumb: The amount of drink allowed corresponds to the amount of urine plus 500 to 800 milliliters per day. Since the regular determination of the amount of urine is cumbersome, dialysis patients should check their weight gain by weighing them daily. The daily weight gain should not be more than 0.5 to 1 kilogram. Between two dialyses, patients should not gain more than two to three kilograms.
In addition to the amount of water they drink, dialysis patients must also consider the water content in food. Soups, fruit, vegetables, pudding or yoghurt sometimes consist of more than 90 percent water. On average, our dishes contain 60 percent water.
To relieve the feeling of thirst with limited fluid intake, the following tips will help:
- Avoid salty foods! Seasoning instead of salt.
- Avoid sweet drinks.
- Take medication with food (save amount of drink).
- Suck small ice cubes or lemon pieces.
- Chewing gum without sugar or sucking sour drops.
Diet during peritoneal dialysis (peritoneal dialysis)
In contrast to hemodialysis, patients undergoing peritoneal dialysis can be a little more generous with their diet. In particular, the restriction on the consumption of fruit and vegetables is not quite as strict as with hemodialysis. Nevertheless, caution also applies to peritoneal dialysis patients with:
- the amount of drinking,
- the enjoyment of fruit and vegetables and
- the intake of phosphate-containing foods.
A strict reduction in table salt is usually not necessary with peritoneal dialysis. For this, the sugar content (glucose content) of the dialysate must be taken into account in the diet so that the dialysis patients do not put on too much weight. Since peritoneum dialysis also results in a loss of "ready-made" proteins (not just protein building blocks as in hemodialysis), patients must above all ensure that they have a sufficient supply of high-quality proteins.
Tags: Baby Child interview therapies