ICD implantation
Dr. med. Philipp Nicol is a freelance writer for the medical editorial team.
More about the experts All content is checked by medical journalists.During an ICD implantation, doctors permanently insert a defibrillator into a patient with a heart condition. This can correct dangerous cardiac arrhythmias and thus protect the wearer from sudden cardiac death. Find out how an implanted defibrillator works, when it is used and what you need to consider after the procedure.

What is an ICD implantation?
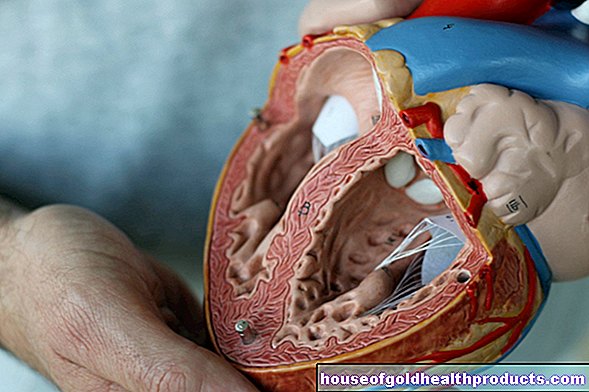
With an ICD implantation, an implantable cardioverter defibrillator (ICD) is inserted into the body. This is a device that detects life-threatening cardiac arrhythmias and terminates them with the help of a strong current surge - this is why it is also called a "shock generator". Its function is comparable to that of a portable defibrillator, which emergency responders use for resuscitation measures.
The ICD looks like a small box the size of a matchbox. This box is implanted by a doctor during the ICD implantation in the body, from where it then works permanently. The battery-operated ICD is usually used in the shoulder area directly under the skin (subcutaneously). Electrode cables go from the device through large veins into the interior of the heart (atria and ventricles). Depending on the number of probes, a distinction is made between the following systems for an ICD implantation:
- Single chamber systems: a probe in the right atrium or in the right ventricle
- Bicameral systems: two probes, one in the right atrium and one in the right ventricle
- Three-chamber systems: an additional third probe in the left chamber
The ICD devices are programmed individually and can thus be adapted to the needs of the respective patient.
How does a defibrillator work?
A normal defibrillator can effectively end so-called tachycardiac arrhythmias (if the heart continues to beat too fast) in an emergency by emitting a high current impulse (shock). These cardiac arrhythmias include, for example, ventricular tachycardias, which can develop into ventricular fibrillation in an emergency. Because the heartbeat is too fast, the blood is no longer pumped properly through the body. Therefore, immediate action must be taken in the case of ventricular fibrillation, i.e. resuscitation measures using chest compressions and defibrillation are necessary.
During defibrillation, the high current impulse brings the asynchronously beating, "flickering" heart to a complete standstill for a few seconds. Then the heart starts beating again by itself and ideally in the right rhythm. It works in a similar way after an ICD implantation. The ICD can detect tachycardia through the electrode cable located in the heart and at the same time terminate it by delivering an immediate shock.
In the case of bradycardia (when the heart continues to beat too slowly), the use of a normal, external defibrillator is unsuitable. An ICD, on the other hand, also has a pacemaker function ("pacing"). This means that bradycardia can also be stopped with light electrical stimulation after an ICD implantation. However, if the heart is completely still (asystole), it can only be restarted by giving heart-stimulating medication immediately.
Differences to the pacemaker
In contrast to the pacemaker, two probes are surrounded by metal spirals in order to be able to deliver a real shock. An ICD can defibrillate ventricular fibrillation, which a pacemaker cannot. An ICD can, however, be combined with a pacemaker.
When is an ICD implantation performed?
There are three main reasons for using an ICD:
ICD implantation for primary prevention
If an ICD is implanted to prevent the occurrence of an illness, it is called "primary prevention". Possible target group here are patients who ...
- ... have an acquired heart condition (heart attack, coronary artery disease, heart failure).
- ... have a significantly reduced cardiac output (heart failure) and thus a high risk of life-threatening cardiac arrhythmias (for example in the case of dilated cardiomyopathy).
Implanting the defibrillator significantly reduces the likelihood of dying from so-called sudden cardiac death.
ICD implantation for secondary prevention
If you have already suffered life-threatening cardiac arrhythmias (tachyarrhythmias) and coped with fainting attacks or even survived cardiac arrest, an implantable defibrillator prevents these disorders from recurring. In this case, the doctor speaks of secondary prevention.
ICD implantation for congenital heart diseases
If you suffer from a genetic heart disease that is associated with an increased risk of cardiac arrhythmias, an ICD implantation is also usually carried out. These rare diseases include the long and short QT syndrome, Brugada syndrome and various heart muscle diseases (cardiomyopathy).
ICD implantation for resynchronization therapy
A defibrillator is also often implanted for cardiac resynchronization therapy (ICD-CRT or ICD-C). This therapy is mainly used in the case of severe cardiac insufficiency with significantly reduced ejection power of the heart (ejection fraction). This often leads to a disordered or asynchronous heartbeat: the right ventricle beats first and the left ventricle a few milliseconds later. The heartbeat can be synchronized again through the simultaneous stimulation of both chambers by means of two chamber probes. As a result, the ICD-CRT improves the heart's pumping function and lowers the risk of dying of heart failure.
How is an ICD implantation performed?
The implantation of the ICD often takes less than an hour. With a few exceptional cases, ICD implantation is usually carried out without general anesthesia. Instead, patients are given local anesthesia and, if necessary, a "sleep injection" (light sedation). An external defibrillator must be connected to the patient and usable during the entire implantation. In addition, the patient is continuously monitored on a monitor.
The doctor usually numbs a spot below the collarbone locally and makes a small incision (a few centimeters long). There he looks for a vein (usually the collarbone vein) and pushes the probe (s) into the heart through it. The whole thing takes place under X-ray monitoring. After inserting the defibrillator, the probes are then attached to the chest muscle and then connected to the ICD device. The cardioverter itself is implanted in a small "tissue pocket" under the skin or the pectoral muscle below the collarbone.Finally, the interface is sewn with a few stitches.
To test whether the ICD implantation was successful, the patient is placed under a short anesthetic and ventricular fibrillation is triggered. The defibrillator must detect this and deliver an electric shock. If everything works properly, the anesthesia is terminated and the ICD is ready for use.
What are the risks of an ICD implantation?
ICD implantation is now routine cardiac surgery. Almost 26,000 defibrillator operations were performed in Germany in 2017. Even so, there are some risks associated with it. Overall, however, the number of complications has been falling continuously for years, not least because the surgical technique is constantly being improved and ever smaller devices are being transplanted.
The most common complications include bleeding, infection, perforation of the heart wall, or cable dislocation. In order to reduce the risk of complications, patients are given one-time antibiotics (perioperative antibiotic administration) immediately before cardiovascular surgery. After the defibrillator implantation, the operated person receives anticoagulant medication that prevents blood clots.
Even after the defibrillator has been implanted, complications cannot be ruled out. A frequent problem (up to 40 percent of cases) after ICD implantation is irregular shock delivery: if the ICD mistakenly diagnoses a comparatively harmless atrial fibrillation as life-threatening ventricular tachycardia, it tries to end this by delivering multiple shocks, which is extremely painful for those affected and is traumatizing. If in doubt, the correct programming of the ICD must be checked and possibly changed.
What do I have to consider after an ICD implantation?
In the first few days after the ICD implantation, you should take care of your left arm and not raise it more than 90 degrees so that the ICD device and the probes do not shift but grow in properly.
Before discharge from the clinic (after about a week), the device system is checked again and programmed according to your needs. A second check-up takes place four to six weeks after the ICD implantation.
Follow-up examinations after an ICD implantation are very important. The doctor checks the correct functioning of the ICD and checks, for example, the charge level of the battery.
Contact your cardiologist or a 24-hour emergency center immediately if you suspect problems with the defibrillator, such as:
- Frequent irregular shock delivery
- ICD system infection suspected
- Worsening heart failure
- Irregular heartbeat etc.
After an ICD implantation, you should also carry a corresponding ID document with you that documents the type of system implanted. And: certain medical procedures (MRI examination or various treatments with electrical current) may no longer be used on you, as they can impair the correct functioning of the ICD.
Despite everything, there is usually no alternative to ICD implantation and it is an extremely effective therapy for life-threatening cardiac arrhythmias.
Tags: drugs sex partnership alcohol