Endometriosis
and Martina Feichter, medical editor and biologistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Endometriosis is when uterine lining-like cells settle outside the uterine cavity (Cavum uteri). Although the condition is benign, many people suffer from severe menstrual cramps, abdominal pain between menstrual periods, painful intercourse, and infertility. Read everything you need to know about the symptoms, causes, diagnosis, treatment and prognosis of endometriosis here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N80D39
Endometriosis: Quick Reference
- What is endometriosis One of the most common abdominal diseases in women. The uterine lining also settles here outside the uterine cavity, for example on the ovaries or between the uterus and rectum. Sexually mature women are usually affected. Endometriosis is rarely noticeable before the first or after the last menstrual period.
- Causes: Unknown, but there are various assumptions, for example that mucous membrane cells with backward flowing menstrual blood reach the abdomen via the fallopian tubes or that a malfunction of the immune system is involved in the development of the disease.
- Symptoms: Some patients have no symptoms whatsoever. Others report severe menstrual pain, abdominal pain regardless of menstruation, pain during sexual intercourse, urination or bowel movements.
- Possible consequences: The illness can be psychologically very stressful and can be associated with infertility.
- Treatment: drugs (pain relievers, hormonal drugs), surgery; supportive often complementary methods (such as relaxation techniques, acupuncture etc.)
- Prognosis: Endometriosis is usually chronic. The course is not predictable. Endometriosis foci can regress spontaneously as well as spread further. Therapy can usually alleviate the symptoms, but relapses often occur afterwards. With the onset of menopause, endometriosis usually comes to rest.
Endometriosis: description
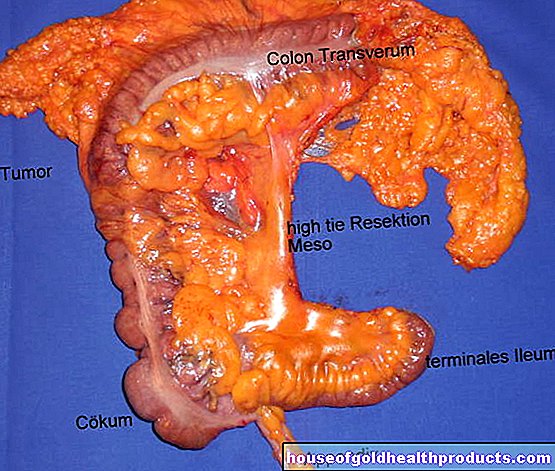
In endometriosis, scattered cell aggregates from the uterine lining (endometrium) occur outside the uterine cavity. These cell islands are called endometriosis foci. Depending on their location, doctors differentiate between three broad groups of endometriosis:
- Internal genital endometriosis: Endometriosis foci within the muscle layer of the uterine wall (myometrium). Doctors speak of adenomyosis (adenomyosis uteri). Endometriosis foci in the fallopian tube also belong to the group Endometriosis genitalis interna.
- External genital endometriosis: the most common form of disease. Endometriosis foci in the genital area (in the small pelvis), but outside the uterus, for example in the ovaries, on the straps of the uterus or in the Douglas space (recess between uterus and rectum).
- Endometriosis extragenitalis: Endometriosis foci outside the small pelvis, for example in the intestine (endometriosis intestine), in the bladder, in the ureters or - very rarely - in the lungs, in the brain, in the spleen or in the skeleton.

The endometriosis foci are estrogen-dependent and behave like the mucous membrane within the uterine cavity: they are built up and shed again alternately as part of the menstrual cycle (with a little bleeding). The cell remains and the blood cannot be excreted through the vagina - as is the case with the regular mucous membrane in the uterine cavity. Sometimes the body can remove them easily and unnoticed (absorb them into the surrounding tissue and break them down).
Often, however, tissue remnants and blood from the endometriosis focus cause inflammation and adhesions or adhesions, which can cause more or less severe pain. In addition, so-called chocolate cysts (endometriomas) can form, for example on the ovaries. Cysts are fluid-filled cavities. In endometriosis patients, these cavities are filled with old, clotted blood and appear brownish as a result. Hence the name chocolate cysts.
Endometriosis: incidence
Endometriosis is considered to be widespread. However, there is no reliable information on the exact frequency - especially since the endometriosis foci in many cases do not cause any symptoms and then often go undetected. Doctors estimate, however, that there are around 40,000 new cases per year in Germany.
It usually takes a long time for endometriosis to be recognized: in Germany, it takes an average of ten years between the onset of symptoms and diagnosis.
Endometriosis in men is extremely rare.
Endometriosis: symptoms and consequences
The scattered islands of uterine lining often cause more or less severe symptoms in affected women. However, endometriosis can also remain completely without symptoms. Below are the main symptoms that can occur with endometriosis, as well as possible consequences of the condition:
Severe menstrual pain: With endometriosis, the pain and cramps can be particularly severe shortly before and during menstruation. Doctors then speak of dysmenorrhea. Especially endometriosis in the uterine muscles can cause severe pain. In some women, menstrual pain is so severe that they cannot go about their work and have to take strong pain relievers.
Other abdominal pain: More or less severe pain in different places in the abdomen can occur in endometriosis regardless of the menstrual period. Sometimes this pain radiates to the back or legs. The symptoms can arise from adhesions between different organs in the abdomen, for example between the ovaries, intestines and uterus. Sometimes the solidified and less elastic structures also cause persistent pain. In addition, foci of endometriosis can release inflammatory substances that additionally irritate the tissue and can lead to pain.
Pain during sexual intercourse: Pain during sex (dyspareunia) - sometimes even afterwards - are also common endometriosis symptoms. Affected women often describe them as burning or cramping. The cause is often endometriosis foci on the elastic straps that "anchor" the uterus in the small pelvis: They can cause pain if the pelvic organs move as usual during sexual intercourse. The symptoms can be so severe that affected women do without sex altogether. That can put a heavy strain on a partnership.
Pain when urinating or defecating: Less common endometriosis symptoms include pain when urinating, and bloating and pain when defecating. They are caused by endometriosis foci in the bladder or in the intestine. Sometimes, depending on the cycle, there is also blood in the urine or stool.
Tiredness and exhaustion: Severe and / or frequent endometriosis symptoms can be physically stressful in the long run. General exhaustion and tiredness are possible consequences.
Psychological stress: In addition to physical stress, endometriosis often also means psychological stress. Many affected women suffer emotionally from severe or frequent pain. This is especially true when countless visits to the doctor are necessary before the cause of the symptoms is determined - which unfortunately happens very often.
The extent of the symptoms in endometriosis is not related to the stage of the disease! For example, women with few / small foci of endometriosis may have more pain than patients with larger foci.
Infertility: Many women with endometriosis cannot get pregnant. The exact reason for this is unknown. However, there are indications that egg cell development and early embryonic development may be disturbed in the patients. You can read more about the causes and treatment of unwanted childlessness in endometriosis under Endometriosis & the desire to have children.
Cancer: Endometriosis is a benign disease and is not associated with a generally increased risk of cancer. However, a malignant tumor (usually ovarian cancer) can develop on the basis of endometriosis. But that only happens very rarely.
It has also been observed that endometriosis is sometimes associated with various cancers. These include, for example, renal cell carcinoma (most common type of kidney cancer), brain tumors, black skin cancer (malignant melanoma), non-Hodgkin's lymphoma (forms of lymphatic cancer) and breast cancer (breast cancer). The clinical significance of this observation is not yet known.
Endometriosis: treatment
Endometriosis therapy always depends on the extent of the symptoms. Endometriosis found by chance and causing no problems does not necessarily require treatment. Treatment is advisable for:
- persistent pain,
- unfulfilled desire to have children and / or
- a disorder of an organ function (ovaries, ureters, intestines, etc.) caused by endometriosis foci.
Operative and / or drug therapy measures are used. How this endometriosis treatment looks in each individual case depends on several factors. In addition to the extent of the symptoms, the location of the endometriosis focus and the age of the woman play a role. When planning therapy, the doctor also takes into account whether the patient would like to have children or not.
In addition to surgery and / or medication, psychosomatic therapy methods can be very useful for endometriosis: Emotional problems and psychosocial stress can aggravate the pain in endometriosis or, conversely, arise or at least be favored by the disease. This can lead to a vicious circle that significantly limits the patient's quality of life. Early support and advice (e.g. from a psychologist, pain therapist, sex counselor, etc.) can counteract this.
Endometriosis drug treatment
You can take different drugs for endometriosis with different purposes: Painkillers are used to relieve pain and cramps in the abdomen. On the other hand, hormone preparations can slow down the growth of the endometriosis herd.
Painkillers: Many endometriosis patients take so-called nonsteroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid (ASA), ibuprofen or diclofenac. These active ingredients have been shown to help with severe menstrual pain. It has not yet been scientifically proven whether they are also effective for other endometriosis pain. Possible side effects of NSAIDs include stomach upset, nausea, headache and a disorder of blood clotting. The preparations should therefore not be taken frequently or over a long period of time without medical supervision.
For very severe endometriosis pain, the doctor sometimes prescribes so-called opioids. In principle, these are very potent pain relievers. However, their effectiveness in endometriosis pain has not been clearly proven. In addition, opioids can cause side effects such as nausea and vomiting, constipation, and fluctuations in blood pressure. With prolonged use there is also the risk of developing a dependency.
Hormone preparations: Hormonal endometriosis treatment is suitable for patients who do not want to have children. The hormones administered suppress the hormone production in the ovaries and thus also ovulation and menstruation. In particular, the production of estrogens is inhibited. Because the endometriosis herds are dependent on estrogen, they are "immobilized" during hormone therapy. The complaints subside. So far it is unclear whether the hormone treatment can also cause the endometriosis foci to recede and the endometriosis to completely disappear. Various hormone preparations are used:
Sometimes the doctor recommends certain hormonal contraceptives such as the birth control pill or the contraceptive patch for endometriosis patients. Some contraceptive pill preparations can be taken continuously (without a break). This can be an advantage in endometriosis because the withdrawal bleeding (bleeding after the end of a cycle = a pill pack) can be very painful for the patient. This long cycle is not officially approved in Germany, so it takes place "off label".
Other hormone preparations that can be used for endometriosis therapy are so-called GnRH analogues. Like hormonal contraceptives, they can help relieve endometriosis symptoms. However, they have more severe side effects: Symptoms often occur during menopause (mood swings, hot flashes, insomnia, dry vagina). In addition, GnRH analogues can reduce bone density with prolonged use.
Progestin preparations (luteal hormones) such as dienogest or dydrogesterone can also relieve endometriosis pain. They are taken continuously in tablet form. If the pain persists even after an endometriosis operation, a progestin-containing IUD (hormone IUD with levonorgestrel) can be inserted into the uterus. Sometimes this helps better against the symptoms than the operation alone. Possible side effects of progestins include intermenstrual bleeding, headaches, mood swings and decreased sexual interest (loss of libido).
Surgical endometriosis treatment
Surgery may be indicated if the endometriosis is causing severe discomfort and / or infertility. Even with "chocolate cysts" of the ovaries, surgery can usually not be avoided (hormone treatment alone is not sufficient here). The same applies if the endometriosis has affected the intestines or the bladder and disrupts the function of these organs.
If the endometriosis has grown deep into the tissue of other organs (such as the vagina, bladder, intestine), the operation should be performed in clinics where one has a lot of experience with such interventions.
The aim of an operation for endometriosis is to remove the scattered uterine lining islets as completely as possible - using a laser, electric current or scalpel. Sometimes it is also necessary to remove some of the affected organs (fallopian tubes, etc.). The procedure is usually carried out as part of a laparoscopy. A large abdominal incision (laparotomy) is less often necessary.
If the endometriosis is causing very severe symptoms, other treatments do not help and there is no desire to have children, some women opt for a complete removal of the uterus (hysterectomy). Sometimes the symptoms stop, but not always. Then the ovaries may also be removed. This deprives all herds of endometriosis of the estrogens necessary for growth (ovaries are the main production sites for these hormones).
The removal of the ovaries puts the patient suddenly into menopause. Therefore, this radical intervention should be considered very carefully. If very severe menopausal symptoms occur after the operation, the woman can take estrogen preparations against it. However, these can also cause the endometriosis symptoms to return.
-
"Speak actively to your doctor about endometriosis"
Three questions for
Dr. med. Thomas Füger,
Specialist in Obstetrics and Gynecology -
1
Why is endometriosis so difficult to diagnose?
Dr. med. Thomas Füger
Diagnosis is actually easy, but many doctors do not think about it even with typical symptoms. Any woman who suffers from severe menstrual pain is suspected of having endometriosis. However, many simply treat this with pain relievers or hormonal contraceptives. On average, it takes 7 to 8 years from the onset of the symptoms to their treatment.Therefore, if in doubt, speak to your gynecologist directly about endometriosis!
-
2
Is it hard to find the root cause?
Dr. med. Thomas Füger
Not for a seasoned endometriosis expert. If the endometriosis is on the ovaries or the uterus, ultrasound is sufficient for diagnosis. For everything else, you have to do a laparoscopy. That scares many at first. But with a laparoscopy, the endometriosis focus is also removed immediately. So it is diagnosis and - the only possible - therapy rolled into one.
-
3
Once the tissue is removed, is one cured?
Dr. med. Thomas Füger
Unfortunately, no. Endometriosis is a chronic condition. That is, as long as the woman has a cycle, endometriosis can come back. The risk after an operation is 30 to 40 percent. I recommend hormone therapy to prevent recurrence after the operation. And: Basically, removing the tissue initially brings great pain relief - and in many cases it is then much easier to have children.
-
Dr. med. Thomas Füger,
Specialist in Obstetrics and GynecologyMedical director of the Center for Minimally Invasive Surgery (MIS) at the Englischer Garten and the Clinical Endometriosis Center of the Dr. Geisenhofer in Munich.
Medication plus surgery
Sometimes drug and surgical endometriosis treatment are combined: the patients receive hormone preparations (mostly GnRH analogues) before and / or after a laparoscopy. Pre-treatment with hormones is intended to reduce the endometriosis focus as much as possible. Hormone treatment after the operation is intended to calm any remaining endometriosis foci and prevent the formation of new foci.
So far, however, studies have not proven that a combination of hormone treatment and laparoscopy is actually more promising than surgery alone - neither in terms of pain nor the chances of pregnancy. In addition, the hormone treatment caused side effects in some patients.
Endometriosis: Complementary Therapies
Some women with endometriosis use alternative / complementary healing methods for their symptoms. The palette ranges from medicinal plants and homeopathy to acupuncture, relaxation and movement techniques (such as yoga or tai chi) and psychological pain management training to chiropractic treatments and TENS (transcutaneous electrical nerve stimulation). A change in lifestyle (more exercise, reducing stress, etc.) should also be helpful.
Such alternative / complementary healing methods can actually improve the symptoms and quality of life of some patients, even if there is no scientific evidence of their effectiveness. Anyone interested in such procedures should discuss their application and possible side effects with an experienced doctor or therapist.
Tip: Endometriosis pain can sometimes be relieved by applying heat, for example in the form of a hot water bottle, a heat pack or a warm bath. Warmth has a calming, relaxing and antispasmodic effect.
Endometriosis: causes and risk factors
Exactly how endometriosis develops is still unclear despite intensive research. But there are different theories about it. One of them is the so-called procrastination or transplant theory:
It assumes that cells in the lining of the uterus are carried from the uterine cavity to other parts of the body. This should happen either via the circulatory system or via a "reverse" (retrograde) menstruation - i.e. via a backflow of menstrual blood via the fallopian tubes into the abdomen. In fact, it is known that retrograde menstruation occurs in nine out of ten women. In theory, it is therefore quite conceivable that mucous membrane cells from the uterus could get into the abdominal cavity in this way.
The metaplasia theory forms a contrast to the transplant theory: According to it, the mucous membrane cells of the endometriosis foci arise directly on the spot (e.g. in the ovaries) and are not carried there from the uterus. Instead, for unknown reasons, they are said to develop from local cells that arose from the same embryonic cell line as the uterine lining cells during development in the womb. This could explain why endometriosis can also occur in men (albeit extremely rarely) - the original embryonic tissue is also found in them.
Other factors could also contribute to the development of endometriosis, for example a disrupted interplay of hormones. A malfunction of the immune system is also discussed: Normally, the immune system ensures that cells from a certain organ cannot settle in other parts of the body. In addition, antibodies against uterine lining can be detected in the blood of some patients. These antibodies trigger inflammation in the area of the endometriosis focus. However, it is not yet known whether these antibodies are the cause or the consequence of endometriosis.
Genetic factors could also play a role in the development of endometriosis. Sometimes the disease occurs in several women in the same family. However, there is no evidence that endometriosis is directly hereditary.
Endometriosis & the desire to have children
Many women with endometriosis try unsuccessfully to get pregnant. In such cases, experts generally recommend surgery: surgically removing the dislocated uterine lining can increase the chances of conceiving.
However, this cannot be achieved with endometriosis drug treatment alone. Even hormone treatment with GnRH analogues after an operation cannot improve the fertility of the patient any further.
In some women, new foci of endometriosis form after an operation, so that a pregnancy continues to fail. Then you should not operate again. Instead, experts advise affected women to try artificial insemination.
You can read more about infertility in endometriosis and the various treatment options in the article Endometriosis & the desire to have children.
Endometriosis: examinations and diagnosis
If endometriosis is suspected, women should see a gynecologist. He will first collect the medical history in a detailed conversation (anamnesis): Among other things, he will have the symptoms (severe menstrual pain, pain during sexual intercourse, etc.) described in detail. He also asks how long these have existed and how much they affect everyday life and a possible partnership. In addition, the doctor asks whether endometriosis has already been diagnosed in the family (for example in the mother or sister).
Endometriosis often causes no symptoms at all. It is only discovered by chance (if at all), for example when a woman undergoes a closer examination for involuntary childlessness.
The next step is a pelvic exam. This includes having the doctor palpate the abdominal wall, vagina, cervix, and rectum. This can give him clues about possible pain, hardening or adhesions in these areas.
The doctor can also obtain valuable information from ultrasound examinations of the abdominal wall and the vagina (transvaginal sonography). It can often be used to identify larger foci of endometriosis, as well as cysts and adhesions. Ultrasound through the vagina is particularly suitable for detecting ovarian cysts. Transvaginal ultrasound is also necessary if there is a suspicion of endometriosis in the muscular wall of the uterus (adenomyosis).
If the doctor suspects endometriosis in the urinary tract, he will also examine the kidneys using ultrasound: If the endometriosis foci constrict the ureters, the urine can back up into the kidneys and damage the organ.
If endometriosis is suspected, the doctor often takes a tissue sample from suspicious areas and has it examined in the laboratory for a histological examination. Samples are usually taken via a laparoscopy. The tissue examination can show whether it is actually an endometriosis or perhaps another (possibly malignant) disease.
In individual cases of endometriosis, further examinations can be useful. For example, if the bladder or rectum is suspected to be infested, a cystoscopy or an endoscopy can bring clarity. In addition to ultrasound, other imaging methods (magnetic resonance imaging, computed tomography) are very rarely used.
Endometriosis: course and prognosis
Endometriosis is usually chronic. How it will develop in individual cases cannot be predicted. In some women, the endometriosis foci resolve spontaneously without treatment. In others, the disease progresses: The scattered mucous membrane islands grow steadily, spread and can affect various organs. This can make repeated surgeries necessary.
With the right therapy, the symptoms of endometriosis can be alleviated in most cases. However, the freedom from symptoms is not always permanent: If endometriosis has been successfully treated with hormones, the symptoms often return after stopping the medication. An operation is also no guarantee of lasting freedom from symptoms: in almost four out of five women, new foci of endometriosis form within five years of the operation.
With the onset of menopause, endometriosis subsides in most women.
Additional information
Books:
- Endometriosis: Advice and help for those affected and their relatives (Advice & Help), Ewald Becher and Adolf Schindler, Kohlhammer W., GmbH, 2010
- How we live with endometriosis - everyday life with chronic abdominal disease: companion book for affected women, their families and medical contacts, by Kathrin Steinberger, edition riedenburg, 2013
Guideline:
- S2k guideline for the "Diagnosis and Therapy of Endometriosis" of the German Society for Gynecology and Obstetrics
Self help:
- Endometriose Association Germany e.V.: http://www.endometriose-vereinigung.de/selbsthilfegruppen.html
- Network endometriosis: http://www.netzwerk-endometriose.de/selbsthilfegruppen/