Pulmonary fibrosis
All content is checked by medical journalists.Lung fibrosis occurs when the proportion of connective tissue in the lungs increases abnormally. Pulmonary fibrosis is one of a large group of diseases that are summarized under the term interstitial lung diseases. There are a number of different diseases that can cause pulmonary fibrosis. Learn more about it here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J84
Pulmonary fibrosis: description
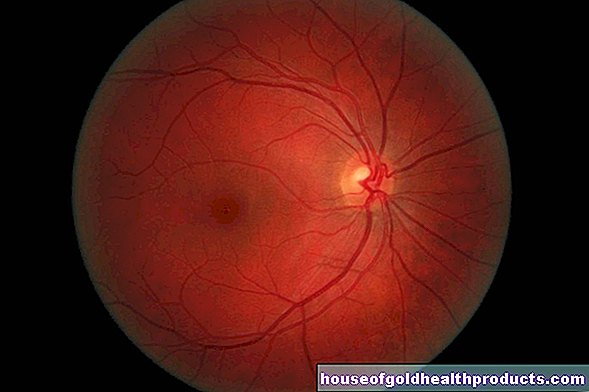
Pulmonary fibrosis can develop as a result of various lung diseases. Some of these have completely different causes, but ultimately lead to similar structural changes in the lungs. The lungs consist, on the one hand, of air-carrying parts and, on the other hand, of a connective tissue support structure. The air-carrying areas include the bronchi, which branch further into the smaller bronchioles and finally open into the smallest functional unit of the lungs - the alveoli. The alveoli are surrounded by a fine network of vessels. The so-called gas exchange takes place via thin membranes that line the alveoli from the inside. The oxygen from the air gets into the blood here, carbon dioxide is released from the blood into the air we breathe.
Connective tissue is located between the air-conveying areas, which supports the lungs and gives them elasticity. The connective tissue of the lungs is also called the interstitium in technical terms. Diseases that take place in this area are accordingly referred to by doctors as interstitial lung diseases. Chronic inflammation in particular can lead to a large increase in the connective tissue of the lungs. This also thickens the wall of the alveoli and increases the distance between the air you breathe and the surrounding blood vessels. As a result, the blood is no longer well oxygenated. The causes of interstitial lung disease are very diverse, in about half of the cases the exact reason for the pulmonary fibrosis is not known.
Pulmonary fibrosis: symptoms
The symptoms of pulmonary fibrosis are often not very specific at first. Over time, the symptoms grow in severity and become more noticeable. Those affected often notice that their physical resilience is decreasing. Everyday activities that they used to be able to do easily get them out of breath faster. In the course of the disease, the shortness of breath eventually occurs without any exertion. As more and more connective tissue forms in the lungs as part of the disease, the membrane between the alveoli and blood vessels also thickens. The oxygen from the air has to overcome a thicker layer in order to get into the blood. As a result, the oxygen level in the blood drops. The body tries to compensate for this by increasing the number of breaths per minute. A dry, dry cough that has persisted for a long time often indicates a disease of the lungs.
In the advanced stages of pulmonary fibrosis, the skin of some affected people turns bluish due to the lack of oxygen (cyanosis). A long-term insufficient supply of oxygen can also lead to changes in the fingers. The bone thickness of the distal phalanges increases, making the fingertips look round and distended. Doctors also refer to them as drumstick fingers because of their appearance. Often the fingernails are noticeably bulging at the same time (glass clock nails). However, these symptoms are not exclusive to pulmonary fibrosis; they can also be an expression of other lung or heart diseases.
Pulmonary fibrosis: causes and risk factors
Doctors basically divide pulmonary fibrosis into two categories: interstitial lung diseases of known cause and so-called idiopathic pulmonary fibrosis, the cause of which is unknown. Both forms are roughly balanced in terms of their frequency.
The following causes of pulmonary fibrosis are known:
- Infections: e.g. by viruses or parasites
- Inhalation of harmful substances: If harmful, inorganic dusts such as quartz dust or asbestos are inhaled, a so-called dust lung can develop. Often this form is an occupational disease, e.g. in miners. Certain gases or vapors as well as cigarette smoke can also cause lasting damage to the lung tissue.
- Medicines: These include certain drugs for cancer therapy such as bleomycin or busulfan, as well as the active ingredient amiodarone against cardiac arrhythmias
- Weed killers: e.g. the herbicide paraquat
- Ionizing radiation: Radiation therapy used to treat cancer, when applied to the chest area, can damage lung tissue.
- Heart diseases: With a so-called left heart failure (left heart failure), the blood builds up in the lungs, which in the long term causes lung damage.
- Shock lung: The condition can occur due to a wide variety of damaging factors and is the result of a prolonged lack of blood supply to the lung tissue.
- Chronic kidney failure: Impaired excretion of water can cause fluid to accumulate in the lungs and thereby damage them.
- Certain diseases: These include diseases of the connective tissue, such as sarcoid or collagenosis, as well as rheumatoid arthritis, various vascular and storage diseases.
Of the interstitial lung diseases of unknown cause, interstitial pulmonary fibrosis is the most common form. In addition, other variants are known; they differ from one another considerably in terms of their course and characteristics.
Pulmonary fibrosis: examinations and diagnosis
Symptoms such as shortness of breath and dry coughs usually give rise to a doctor's visit. Such symptoms do not only occur with pulmonary fibrosis, but can also be caused by numerous other diseases. In order to distinguish these from one another, the doctor first conducts a detailed discussion with the patient (anamnesis). For example, he asks how long the symptoms have existed and whether there are known comorbidities. Information about the professional environment - for example whether the person concerned is regularly exposed to harmful gases or dusts - provides the doctor with important information for diagnosing pulmonary fibrosis. During the physical exam, the doctor will listen to the patient's chest with a stethoscope. A crackling rattle or squeaking noise - as if corks are rubbing against each other - are typical signs of pulmonary fibrosis.
A lung function test shows how severely the respiratory function is impaired. For example, the doctor measures the lung volume and checks the maximum amount of air the patient can inhale or exhale. Testing lung function is relatively simple: the patient usually has to inhale and exhale through a mouthpiece into a device. In addition, the measurements are also made in response to certain commands (e.g. sudden strong exhalation as long as the breath lasts). The determination of the so-called diffusion capacity (DCO) also provides an important statement. This measures the ability of the lungs to transport oxygen from the air into the blood.
In order to narrow down the diagnosis further, imaging examinations, such as computed tomography of the chest, usually follow. If the suspicion of pulmonary fibrosis is confirmed, the lungs are finally mirrored (bronchoscopy). As part of this examination, the doctor can also obtain cells by rinsing the bronchi (bronchial lavage) or take a tissue sample (biopsy). The specimens are then examined for their tissue (histopathologically) under the microscope.
Since the diagnosis of the exact form of pulmonary fibrosis and its possible underlying disease is very complex, doctors from various disciplines usually work hand in hand.
Pulmonary fibrosis: treatment
The aim of the treatment of pulmonary fibrosis is to stop the course of the disease or at least to slow down a further increase in connective tissue (fibrosis) as far as possible. If a causative underlying disease (e.g. rheumatoid arthritis) is known, it must be treated accordingly. Other causes, such as harmful substances in the air or smoking, should be avoided as far as possible. A change of occupation may also be necessary for this.
Often an excessive reaction of the immune system and inflammatory processes in the lung tissue contribute to the disease process. Therefore, doctors often use drugs to treat pulmonary fibrosis that have an anti-inflammatory effect and reduce the immune system (immunosuppressants). One of the best-known representatives from this group is, for example, cortisone. The patient can either inhale the active ingredient directly or receive it in the form of tablets or syringes. A newer agent with the active ingredient pirfendione inhibits fibrosis and also counteracts inflammation. If the oxygen level in the blood falls below a certain level, those affected receive additional oxygen via a probe - ideally for many hours a day. If the treatment measures do not work and the pulmonary fibrosis is already very advanced, the last treatment option is a lung transplant.
Pulmonary Fibrosis: Prevention
Lung fibrosis can have many different causes, so there is no specific measure that can be used to prevent the disease. However, to reduce the risk of lung diseases such as pulmonary fibrosis, it is advisable not to smoke or to avoid other pollutants in the air. This includes, for example, appropriate occupational safety (such as breathing filters) for people who are often exposed to polluted or dusty air at work. In the case of idiopathic pulmonary fibrosis, however, no prevention is possible.
Pulmonary fibrosis: disease course and prognosis
The course and prognosis of pulmonary fibrosis depend on many different factors and cannot be generally predicted. The connective tissue remodeling of the lung tissue can no longer be reversed. The extent to which the course of the disease can be slowed down by treatment varies with the individual forms of pulmonary fibrosis. Idiopathic pulmonary fibrosis in particular can be aggressive and can often hardly be influenced by medication. Life expectancy is then significantly shortened in many cases, and a lung transplant can under certain circumstances prolong life.
Forms of pulmonary fibrosis caused by external harmful substances - such as dust or smoking - improve in many cases well if the trigger is avoided. These forms usually respond to anti-inflammatory drugs as well.
Tags: skin foot care skin care

















.jpg)