Nephropathy
Updated on All content is checked by medical journalists.Nephropathy is the medical umbrella term for non-inflammatory kidney disease. The most common form is diabetic nephropathy - damage to the kidneys in diabetics who have had high blood sugar for many years. However, nephropathy can also occur in connection with other diseases such as high blood pressure. Read here how nephropathy develops and how it is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N12N07N08N11N15I12
Nephropathy: description
The term nephropathy includes various non-inflammatory diseases of the kidneys. These include:
- diabetic nephropathy (kidney disease caused by diabetes)
- Hypertensive nephropathy (kidney disease caused by high blood pressure)
- Nephropathy due to toxins (such as lead ephropathy) or drugs (analgesic nephropathy)
- Hypercalcemic nephropathy (kidney disease due to increased calcium levels)
- HIV-associated nephropathy
- pregnancy-related nephropathy (Nephropathia gravidarum)
Diabetic nephropathy is the most common. It can occur in both type 1 and type 2 diabetics.
Function and structure of the kidneys
The kidneys are part of the body's urinary system and are paired. That means that everyone has two kidneys. They take on important functions:
- They help regulate blood pressure.
- They are involved in the production of red blood cells.
- They filter metabolic waste products from the blood.
- They produce the urine.
- They make different hormones.
- They regulate the fluid and electrolyte balance
- as well as the acid-base balance.
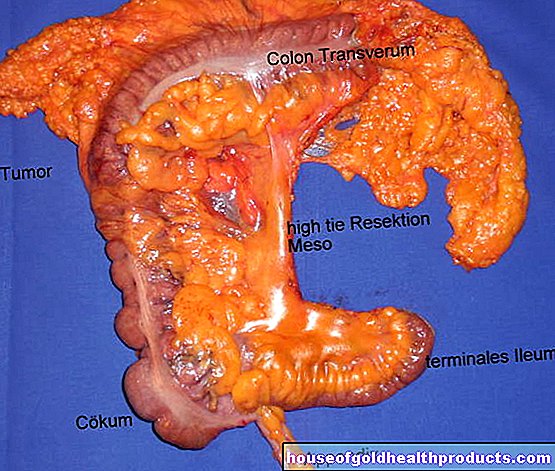
Each kidney consists of around a million small subunits called nephrons. The most important part of a nephron is the kidney corpuscle (glomerulum), a tangle of very fine blood vessels. These have the task of filtering the blood. If they are damaged, the kidney's filtering function suffers. The damage can be caused, for example, by high blood pressure or excessive blood sugar levels for many years.
Nephropathy: symptoms
Diabetic nephropathy: symptoms
Nephropathy often progresses slowly for years without any noticeable symptoms or discomfort. In many cases, it is therefore discovered only by chance, for example in the course of a urine test that is regularly carried out on diabetics. If the protein albumin is increasingly found in the urine, this indicates kidney damage. Healthy kidneys filter out the protein during urine production so that the urine is ultimately free of protein.
Symptoms only become noticeable with advanced diabetic nephropathy. This is the case after several years. The main symptoms of diabetic nephropathy include:
- itching
- Milky coffee-colored skin
- Inefficiency
- exhaustion
- fatigue
- headache
- Anemia
- increased water retention (edema), especially in the legs
- Weight gain
- foamy urine
If nephropathy progresses, patients may need to have blood wash (dialysis) or a kidney transplant.
Other forms of nephropathy: symptoms
With other forms of nephropathy, other signs will occur:
- Nephropathy due to toxins: The toxins cause chronic damage to various functional units of the kidney such as the kidney tubules (tubules) or their vessels (glomeruli). Lead nephropathy damages cells in the kidney tubules, causing the body to break them down - the tubules shrink, which affects their function. In addition, too high a blood pressure develops in the kidneys. There is also an increase in harmful metabolic products in the kidney, which can lead to constipation or loss of appetite and ultimately to kidney failure. Other toxins like mercury or arsenic can also cause kidney failure.
- In analgesic nephropathy, the kidney tubules are damaged by pain relievers. Red blood cells dissolve (hemolysis) and even acute kidney failure occurs.
- With hypertensive nephropathy, symptoms do not appear until the high blood pressure has already caused damage to the kidney. Among other things, nausea, vomiting, headaches and seizures are possible.
- Symptoms of hypercalcemic nephropathy include nausea, vomiting, muscle weakness, high blood pressure, fever and even kidney weakness.
- Pregnancy-related nephropathy is usually preceded by high blood pressure. Here, too, the body loses a lot of protein through the kidneys; water retention (edema) often forms, especially on the arms, legs and face.
Nephropathy: causes
Nephropathies can have very different causes. As mentioned above, diabetic nephropathy is the most common variant.
Diabetic nephropathy
Diabetic nephropathy is caused by a permanently high blood sugar level. This damages the blood vessels: deposits form in the vessels, which lead to constrictions (arteriosclerosis), so that the blood flow is disturbed.
As an organ with a strong blood supply, the kidney suffers particularly badly from vascular damage caused by diabetes. Especially the small vessels of the kidney corpuscles (glomeruli) are affected in diabetic nephropathy. Damage to the vessels increases blood pressure within the kidney corpuscles. As a result, the kidney function, especially the filter function of the kidney, is restricted. The body now excretes more proteins in the urine, which is normally free of proteins.
People with diabetic kidney disease often have high blood pressure at the same time. Due to arteriosclerosis (hardening of the arteries) of the kidney vessels, the blood pressure continues to rise.
Various risk factors accelerate the development of diabetic nephropathy. This includes:
- high blood pressure (hypertension)
- smoking
- increased protein intake with food
- increased fat levels in the blood
- genetic predisposition
Other forms of nephropathy
- In the case of nephropathies caused by toxins, so-called toxic nepropathies, environmental toxins such as lead, mercury, arsenic or cadmium are the causes. They are deposited in the body, especially in the kidneys, and damage the surrounding tissue.
- In so-called analgesic nephropathy, prolonged abuse of pain relievers (such as paracetamol or acetylsalicylic acid) is the cause of the nephropathy. The combined intake of such painkillers is particularly damaging to the kidneys.
- Hypertensive nephropathy occurs when high blood pressure damages the kidney cells.
- Hypercalcemic nephropathy is caused by an increased level of calcium in the blood (hypercalcemia), which leads to kidney problems.
- In pregnancy-related nephropathy, proteins are deposited in the kidney vessels. This happens, for example, with pregnancy-related high blood pressure diseases such as preeclampsia.
Nephropathy: examinations and diagnosis
If nephropathy is suspected, the doctor will usually do blood and urine tests, as well as sometimes imaging tests such as X-rays.
Protein in the urine
The first thing the doctor does is check the amount of albumin in the urine. Albumin is a protein found in the blood. The urine, on the other hand, is usually free of albumin and other proteins. If, however, more proteins are excreted in the urine (proteinuria), this may be due to nephropathy.
The doctor can use a rapid albumin test to measure this. As a rule, however, the urine is collected over 24 hours (24-hour collection urine) and then examined for protein. Even slightly increased amounts of albumin in the urine indicate kidney damage:
- Albumin values of less than 20 milligrams of albumin per liter of urine (mg / l) within 24 hours are normal.
- Values between 20 and 200 mg / l are known as microalbuminuria and are an indication of the onset of kidney damage.
- Values of more than 200 mg / l albumin in the urine are known as macroalbuminuria and are a sign of advanced nephropathy.
Check-ups are important
Nephropathy is not behind every protein excretion in the urine. Even during physical exertion, urinary tract infections, febrile illnesses or due to short-term elevated blood sugar levels, the body can briefly excrete increased amounts of protein in the urine. A single proof is therefore not sufficient - control examinations must confirm the increased measured value.
Diabetics should have their urine checked for proteins regularly (at least once a year). Anyone who already suffers from nephropathy should be examined two to four times a year, depending on the stage of the disease.
Kidney function values
To further diagnose nephropathy, the doctor determines the kidney function values in the blood and urine. These include creatinine, urea and uric acid, among others. If the kidneys are no longer working properly, they are elevated. Together with the albumin values, they enable the doctor to determine the severity of a nephropathy.
X-ray & Co.
The doctor uses imaging procedures, for example, if analgesic nephropathy or hypercalcemic nephropathy is suspected. These diseases can be diagnosed with x-rays, an ultrasound examination (sonography) or computed tomography (CT).
Nephropathy: treatment
Nephropathy is treated very differently depending on the cause. In most cases, this requires medication to treat the underlying disease. These include antihypertensive agents for hypertensive patients, insulin for diabetics or so-called complexing agents that are used in cases of poisoning - for example with lead.
In addition, possible other factors that influence the course are also taken into account in the treatment.
Diabetic nephropathy: treatment
The longer the blood sugar levels are poorly controlled in diabetes, the higher the risk of developing diabetic nephropathy. The blood sugar levels also influence the further course of the disease.
The blood sugar control can be assessed on the basis of the long-term blood sugar value HbA1c. To prevent the progression of the nephropathy, a value below 7.0 percent is aimed for.
If necessary, the attending physician also adjusts the diabetes therapy as soon as there are signs of diabetic nephropathy. Because some drugs such as metformin put additional strain on the kidneys. The doctor will also explain to patients which active ingredients should still be avoided (e.g. certain painkillers).
Nephropathy and hypertension
Early treatment of high blood pressure is also important in the treatment of nephropathy, as this also damages the kidneys. This is especially true for hypertensive nephropathy, the main cause of which is high blood pressure.
Thus, the risk of nephropathy can be reduced if the high blood pressure is set to low values early on. The systolic blood pressure should be below 140 mmHg (preferably 120 mmHG and below) and the diastolic blood pressure below 80 mmHg.
In order to achieve healthier blood pressure values, the following measures are recommended:
- antihypertensive drugs (especially ACE inhibitors and AT1 antagonists)
- Treatment of increased levels of fat in the blood
- Low-protein and low-salt diet
- Reduction of excess weight (with an adapted diet and regular mountain hiking / sport)
- Refrain from nicotine
Further therapeutic measures for a nephropathy
In the case of hypercalcemic nephropathy, it is important to take in as little calcium as possible with food.
If the nephropathy is not treated in time, there is a risk of kidney failure. In the end, only regular blood washing (dialysis) or a kidney transplant will help. In Germany, around a third of all patients who regularly need blood washing are diabetics.
Nephropathy: disease course and prognosis
Depending on their cause, nephropathies can be severe and lead to acute kidney failure.If treatment begins in good time, the course of the disease can be positively influenced and in some cases even stopped.
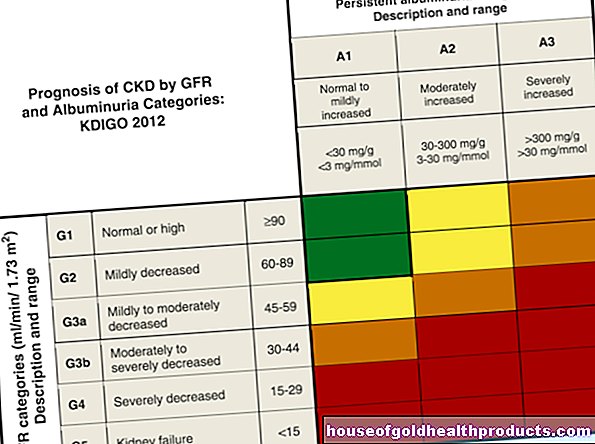
The most common form of nephropathy - diabetic nephropathy - is divided into five stages:
- In the first stage, the body increasingly excretes the protein albumin. The kidneys are damaged, but still function largely normally. A distinction is made between two forms: If the amount of albumin in the urine is low, it is called microalbuminuria, if the amount of albumin is significantly higher, it is called macroabluminuria.
- The other four stages are characterized by kidney damage with varying degrees of kidney weakness (renal insufficiency): mild, moderate and severe kidney weakness. Finally, in the end-stage, there is talk of terminal kidney failure.
If the nephropathy is recognized in good time and the diabetes is then optimally adjusted, the progression of the kidney disease can often be prevented or at least slowed down. In the very early stages, the pathological changes can even be remedied with appropriate measures.
Without treatment, however, kidney function continues to deteriorate - ultimately only blood washing (dialysis) or a kidney transplant will help.
Diabetic nephropathy also increases the risk of heart attack, stroke and diabetic secondary diseases such as diabetic eye disease (diabetic retinopathy).
Regular checks
It is therefore very important to prevent diabetic nephropathy or to recognize it in good time and treat it accordingly. In addition, regular examinations are advisable in order to check the course of the disease and the success of the treatment and, if necessary, to optimize the treatment.
Have your individual risk profile checked regularly so that you can react to critical values as quickly as possible. These include, for example, checking blood pressure and blood lipids (cholesterol). Since patients with diabetic nephropathy also have an increased risk of diseases of the cardiovascular system, special attention should be paid to their cholesterol levels. The decisive factor is the level of LDL cholesterol ("bad cholesterol"). It should be less than 100 micrograms per deciliter (mg / dL).
Nephropathy: prevention
The most common type of kidney disease is diabetic nephropathy. The central adjustment screw here is the blood sugar level: the risk of diabetic nephropathy can be reduced considerably if the blood sugar is optimally adjusted. A well-adjusted blood sugar is also crucial for the further course of the disease.
It is equally important to keep your blood pressure low. This also helps prevent further damage to the kidneys. But there are other factors that can help promote kidney health.
Summary: Tips for a "kidney-healthy" life
Here is an overview of the most important tips for a "kidney-healthy" lifestyle:
- Keep blood sugar and blood pressure in the normal range.
- Eat healthy. In particular, keep an eye on protein and cholesterol intake. A doctor or dietitian can provide more detailed advice on nutrition.
- Drink enough.
- Be cautious about taking pain relievers.
- Only take medication as directed.
- Find out about possible interactions when taking different drugs.
- Avoid pollutants whenever possible.
- Refrain from smoking and drugs.
If you take this advice to heart, you will do a great deal to keep your kidneys healthy and prevent nephropathy from developing.
Tags: sleep medicinal herbal home remedies drugs