Polymyalgia rheumatica
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Polymyalgia rheumatica is an inflammatory rheumatic disease that mainly affects older women. Common symptoms are pain in the shoulder and / or hip area as well as general complaints such as fatigue and fever. Early treatment with cortisone can help many sufferers. Read more about the causes and symptoms of polymyalgia rheumatica as well as the associated diagnosis, treatment and prognosis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M31M35
Brief overview
- What is Polymyalgia Rheumatica (PMR)? Inflammatory rheumatic autoimmune disease (immune system attacks the body's own tissue); Colloquially called inflammatory soft tissue rheumatism or muscle rheumatism
- Causes: Unknown. Genetic factors and external influences (e.g. infections) may be involved in the outbreak of the disease.
- Symptoms: muscle pain (especially in the shoulder and / or pelvic girdle area), stiff muscles and joints in the morning, general complaints (e.g. fatigue, fever, night sweats, weight loss, depressed mood)
- Diagnosis: doctor-patient consultation, physical examination, blood tests, ultrasound (ACR-EULAR classification of polymyalgia rheumatica)
- Therapy: medication (cortisone, possibly also methotrexate); If necessary, further support measures (e.g. physiotherapy, occupational therapy).
- Prognosis: Polymyalgia rheumatica is usually well treatable if detected early. If the corticosteroid therapy is too short (<1 year), the risk of relapse increases.
Polymyalgia rheumatica: definition
Polymyalgia rheumatica (PMR) is an inflammatory rheumatic disease.The term polymyalgia is also popular. Because the immune system attacks the body's own tissue, it is an autoimmune disease.
The attack of the malfunctioning immune system in PMR triggers inflammatory changes in the shoulder, upper arm, pelvic and thigh muscles, as well as the neighboring soft tissue (such as bursa). That is why the disease is colloquially called inflammatory soft tissue rheumatism or muscle rheumatism.
Soft tissue rheumatism and muscle rheumatism are not official names of diseases! Rather, the terms describe the painful complaints in the respective area.
Some people mean by "soft tissue rheumatism" or "soft tissue rheumatism" the fibromyalgia syndrome! However, this is only a certain form of soft tissue rheumatism (generalized soft tissue rheumatism).
Associated with giant cell arteritis
Polymyalgia rheumatica is closely related to another autoimmune disease - giant cell arteritis, or RZA for short (formerly also called temporal arteritis, cranial artery, capitis or Horton's disease). In both cases, autoimmune inflammation of medium-sized and large arteries (arteries) occurs:
- Polymyalgia rheumatica: The area of the shoulder, neck and upper arms is mainly affected, usually later also the pelvic girdle and thighs. Inflammatory changes occur in the artery under the collarbone (subclavian artery). This inflammation spreads to adjacent joints, bursa, and tendon sheaths. The vascular inflammation itself tends to take a back seat (subclinical vasculitis).
- Giant cell arteritis: The inflammation of the arteries is more prominent and mainly affects arteries of the skull, usually the temporal artery (A. temporalis). Inflammatory cells (leukocytes) migrate into the arterial wall. As a result, giant cells are formed - the wall becomes thicker and firmer, and blood flow is disturbed.
Experts disagree as to whether polymaylgia rheumatica and giant cell arteritis are actually two different diseases or whether PMR is rather a milder form of RZA. In any case, some people with polymyalgia rheumatica also develop giant cell arteritis (around 20 percent). Conversely, 40 to 60 percent of patients with RZA also have PMR. In principle, both diseases can occur simultaneously or follow one another (first PMR, then RZA or vice versa).
Polymyalgia rheumatica: who is affected?
Polymyalgia rheumatica is the second most common inflammatory rheumatic disease in old age (after rheumatoid arthritis). It is most common in people between the ages of 70 and 80. Illness before the age of 50 is very rare.
Most patients are female: Polymyalgia rheumatica is two to three times more common in women than in men.
There are also differences in the geographical distribution of the disease: within Europe, polymyalgia rheumatica occurs more frequently in the north than in the south. Overall, the disease is more common in Europeans than in Asians, African-Americans and Latinos.
Polymyalgia rheumatica: cure & prognosis
Polymyalgia rheumatica cannot be overcome quickly. The course generally extends over two to four years. However, some patients suffer from it for ten years or more. It is therefore important to recognize and treat the disease as early as possible.
The right drug treatment (cortisone) can suppress the polymyalgia rheumatica so that the patient no longer has symptoms and the laboratory values are normal. In the best case, it stays that way even after stopping the medication. Doctors then speak of "drug-free remission".
About 50 to 70 percent of all patients with polymyalgia rheumatica are symptom-free after completing cortisone therapy. The following applies: The chances of permanent freedom from symptoms can be increased by long enough cortisone therapy. On the other hand, those who have taken cortisone for less than twelve months are more prone to relapse.
Polymyalgia rheumatica: causes
The cause of polymyalgia rheumatica is not yet known. Experts suggest that there is a genetic predisposition to the disease. Occasionally, the disease occurs more often in families. However, it is not a classic hereditary disease!
In addition to genes, external factors could also be involved in the outbreak of polymyalgia rheumatica. Infections, for example with the parvovirus B19, are discussed. They could trigger the malfunction of the immune system that leads to the inflammatory changes described.
Polymyalgia rheumatica: symptoms
The part of the name "polymyalgia" comes from the Greek and indicates a typical symptom of the disease - a lot of muscle pain:
Those affected develop severe and mostly bilateral (symmetrical) pain in the shoulders, neck and upper arms within a few days to two weeks. The symptoms are mostly based on an inflammation of the bursa, more rarely on an inflammation of the biceps tendon or the joint mucosa (synovitis). The hips, thighs, and lumbar spine areas can also be painful.
The pain is present around the clock - both at rest and during movement and exertion. They often intensify at night in the second half of the night and in the morning. After a while, the pain may ripple and shift.
A pronounced morning stiffness is also typical of polymyalgia rheumatica: joints and muscles feel stiff for more than 45 minutes in the morning. Together with the pain, patients find it difficult to get out of bed and get dressed.
In addition to restricted mobility, some patients also suffer from swollen joints. This can also affect joints that are far from the shoulder or pelvis, usually the hands and knees. If the synovial membrane of the wrists becomes inflamed, some patients also develop carpal tunnel syndrome.
In addition, general symptoms such as:
- Exhaustion, tiredness
- Lack of drive
- fever
- Loss of appetite with weight loss, nausea
- Increased sweating, especially pronounced night sweats
- Depressive mood
If patients have giant cell arteritis in addition to polymyalgia rheumatica, there are other symptoms such as headache (often one-sided and in the temple area), chewing pain and visual disturbances. You can find more symptoms of giant cell arteritis here.
The suspicion of giant cell arteritis is an emergency, especially in the case of visual disturbances! Inflammation of the eye vessels may have developed. Without rapid medical therapy, there is a risk of blindness!
Polymyalgia rheumatica: examinations and diagnosis
In the case of unclear complaints such as severe shoulder and neck pain with exhaustion and fever, the family doctor is usually the first point of contact. If they suspect a rheumatic cause, they will refer you to a specialist. This is usually a specialist in internal medicine and rheumatology, or rheumatologist for short.
There is no single, specific examination for the detection of polymyalgia rheumatica. The doctor makes the diagnosis on the basis of the anamnesis, blood and ultrasound examinations. He excludes other diseases with similar symptoms (such as rheumatoid arthritis, polymyositis).
anamnese
The first step in clarifying your complaints is a detailed discussion about your medical history (anamnesis). The doctor asks you what symptoms you have exactly, how long they have existed and how they are noticeable in everyday life (e.g. stiff joints in the morning, especially severe shoulder and neck pain at night). It is also important for the doctor to know whether there are pre-existing or underlying diseases and whether you are already taking medication.
Physical examination
The interview is followed by a general physical examination. It gives the doctor information about your general state of health and helps rule out other diseases as the cause of the symptoms.
During the physical exam, the doctor pays particular attention to your joints. If the synovial membrane has become inflamed (synovitis) as a result of the polymyalgia, the joints are slightly swollen (e.g. on the hands or knees). The doctor also tests your mobility: Some PMR patients have difficulty lifting their arms over 90 degrees to the sides.
Blood tests
As with almost all inflammatory diseases, noticeable inflammation values can also be determined in the blood in polymyalgia rheumatica: As a rule, the sedimentation rate and / or the C-reactive protein (CRP) have increased in PMR. The number of white blood cells (leukocytes) may also be increased. In addition, doctors sometimes find an increased number of blood platelets (thrombocytes) and a shift in blood proteins.
Autoantibodies such as rheumatoid factor, which is mostly present in the blood in rheumatoid arthritis and some other rheumatic diseases, cannot typically be detected in polymyalgia rheumatica.
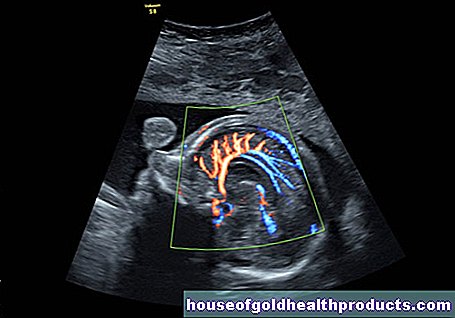
Ultrasonic
In the ultrasound, doctors can detect the inflammatory changes in the shoulder area (e.g. bursitis) that typically occur in polymyalgia rheumatica. X-rays, on the other hand, are inconspicuous. At most they show age-typical changes such as joint wear, but no signs of inflammation.
ACR-EULAR classification of polymyalgia rheumatica
The experts of the European League Against Rheumatism (EULAR) and the American College of Rheumatology developed a point system in 2012 to support the diagnosis of polymyalgia rheumatica. Doctors can apply this score when patients
- are older than 50 years,
- have new shoulder pain on both sides and
- the CRP and / or the blood sedimentation are increased.
The criteria themselves mainly relate to the symptoms of polymyalgia rheumatica, various blood values and an ultrasound examination. Depending on the results of the examination, the person concerned collects points, which speaks for the presence of polymyalgia rheumatica from a corresponding number of points.
Further examinations if necessary
If the doctor suspects, in addition or as an alternative, a giant cell arteritis, a tissue sample (biopsy) of arteries can be informative: Usually a piece is removed from the temporal artery and examined microscopically for inflammatory changes. In the case of polymyalgia rheumatica, on the other hand, the vascular biopsy provides an inconspicuous result.
Sometimes further tests are needed to rule out other diseases. An example: If the cause of the symptoms is polymyalgia rheumatica as well as polymyositis (an autoimmune disease of the muscles), a tissue sample of the painful muscles can help. Such a muscle biopsy is normal in PMR. In the case of polymyositis, on the other hand, typical changes are found in the muscle sample.
In contrast to polymyositis, electromyography (EMG), which measures muscle activity, and the blood value creatine kinase are usually normal.
Once the diagnosis of polymyalgia rheumatica has been made, further examinations for therapy planning can be useful. This can be a bone density measurement, for example. The cortisone therapy necessary for polymyalgia rheumatica can promote or intensify bone loss (osteoporosis).
Polymyalgia rheumatica: therapy
Doctors treat polymyalgia rheumatica with medication. In addition, further therapeutic measures can be useful as support in individual cases.
Medication
The basis of the treatment of polymyalgia rheumatica is always the administration of glucocorticoids ("cortisone") such as prednisone. It should be started immediately after the diagnosis and in sufficient dosage to get the disease and symptoms under control as quickly as possible.
cortisone
Glucocorticoids such as prednisone inhibit the immune system and thereby counteract inflammation. Patients with polymyalgia rheumatica take one cortisone tablet once a day, in the morning. The dosage should be as high as necessary, but as low as possible:
The doctor usually starts therapy with 15 to 25 milligrams of prednisone per day (the exact dose is adjusted individually). He then regularly checks the effect of the treatment and the disease activity. After a few weeks, the cortisone dose can usually be reduced gradually. If there is a relapse (relapse) of the polymyalgia rheumatica, the doctor increases the dosage again.
How long the cortisone has to be taken in total varies from person to person. As a rule, experts recommend taking it for at least a year. Basically, the doctor prescribes the cortisone intake for as long as necessary, but as short as possible. The reason: With prolonged use, cortisone can cause some side effects such as bone loss (osteoporosis). That is why the doctor makes sure that there is an adequate supply of vitamin D and calcium (both important for strong bones) during treatment. If necessary, he prescribes appropriate preparations.
In the case of (additional) giant cell arteritis, cortisone therapy is carried out immediately and in higher doses, as otherwise there is a risk of blindness!
Methotrexate
If a relapse is very likely in patients with polymyalgia rheumatica and / or high-dose and long-term cortisone therapy is necessary, the doctor often also prescribes methotrexate. This can usually reduce the dose of cortisone and thus prevent its side effects.
Combined therapy with cortisone and methotrexate can also be considered if relapses of polymyalgia rheumatica occur repeatedly. The same applies if there are already co-morbidities (e.g. osteoporosis, diabetes) or cortisone does not work sufficiently.
Other drugs for polymyalgia
In order to reduce the dose of cortisone therapy and thus possible side effects, scientists have investigated, among other things, the monoclonal antibody tocilizumab in various studies in polymyalgia rheumatica (and giant cell arteritis). The results so far indicate a benefit in PMR therapy. Tocilizumab could therefore primarily help patients who cannot receive methotrexate or who continue to have symptoms on combination therapy.
Due to the limited number of studies, there is no official recommendation for the use of tocilizumab in the currently valid guidelines!
TNF-alpha blockers, which are used regularly in rheumatoid arthritis, for example, have proven to be ineffective in several studies in polymyalgia rheumatica.
Other measures
Regular check-ups are very important during treatment of polymyalgia rheumatica. In the first year, they are scheduled every four to eight weeks. In the second year they are recommended every eight to twelve weeks. In this way, the attending physician can react quickly to changes.
Contact your doctor as soon as possible if your symptoms worsen or side effects of the treatment occur.
If necessary, patients with polymyalgia rheumatica can receive psychosomatic or psychotherapeutic support - for example if they are very depressed due to the illness.
The attending physician prescribes accompanying physiotherapy and occupational therapy, especially for elderly and frail people. The aim is to prevent the patient from permanently losing mobility in the course of the painful illness.
Because patients are more susceptible to infection, adequate vaccination protection is important. The increased risk of infection results on the one hand from the inflammatory rheumatic disease itself. On the other hand, the cortisone treatment suppresses the immune system. You should therefore make up for any missing vaccinations, preferably before the start of therapy. Some may not be administered during high-dose cortisone treatment (live vaccines such as against measles or rubella). In contrast, the administration of dead vaccines (for example against flu or pneumococci) is not a problem.
Tips for polymyalgia rheumatica
- Join a self-help group - exchanging ideas with other sufferers can help to cope better with the painful illness.
- Avoid overweight or obesity (obesity).
- With polymyalgia rheumatica, make sure you have a varied and balanced diet. We recommend the Mediterranean diet, for example, which is rich in vegetables, fruit and valuable vegetable fats, while meat is only served in moderation.
- Make sure that your body has enough calcium and vitamin D.
- Do not smoke if you have polymyalgia rheumatica and you should consume alcohol in moderation at most.
- Do endurance sports regularly. For example, go running, cycling, or swimming for half an hour three times a week.
- Take the regular check-ups.
With these tips you can improve your quality of life despite polymyalgia rheumatica and support the success of the drug treatment.
Tags: first aid laboratory values parasites



.jpg)