Cardiac arrhythmias
Clemens Gödel is a freelancer for the medical team.
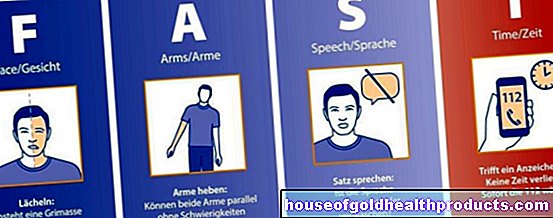
More about the experts All content is checked by medical journalists.With cardiac arrhythmias, the normal heart rate is disturbed by various causes. The heart then either beats too slowly (bradycardia), too fast (tachycardia) or irregularly (arrhythmia). There are disturbances in the formation of electrical impulses that trigger a heartbeat and disturbances in the transmission of these impulses. Read how the arrhythmias differ and how to recognize them.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. R00I48I46I47I49I45I44
Arrhythmias: Where Do They Come From?
Usually the sinus node, a small area in the right atrium, generates electrical impulses for the heart to beat. They first spread over the atria, which then contract. There is a lot of connective tissue of the heart skeleton between the atria and the ventricles. It acts as electrical insulation. The impulses are only conducted into the ventricles at a special connection node, the AV node.
From there, the charges on the bundle of His, the ventricular limbs and the Purkinje fibers run towards and along the apex of the heart. From there, the heart muscle contracts and pumps the blood into the large bloodstream. Cardiac arrhythmias can occur when the sinus node does not generate the electrical impulses properly, the impulses are not transmitted properly, or additional impulses develop in the atrium or ventricle. There are dangerous and harmless cardiac arrhythmias.
How do I recognize an arrhythmia?
Cardiac arrhythmias can cause different symptoms. Palpitations, palpitations, dizziness, chest pain or fainting are some of the typical signs. You can read more about this in the article Cardiac arrhythmias: Symptoms.
What are the causes of cardiac arrhythmias?
You can read everything you need to know about the causes of a cardiac arrhythmia in the article Cardiac arrhythmias: Causes.
Cardiac arrhythmias: what are they?
Arrhythmias can be divided into two main categories. If the heart beats too fast (more than 100 beats per minute), doctors call it tachycardia. A heartbeat that is too slow (less than 60 times per minute), on the other hand, is called bradycardia. Doctors only see relevant bradycardia when the heart beats even more slowly (at least less than 50 beats per minute. It should not be forgotten that some well-trained hearts (athletes) can beat so slowly without being sick.
Another important term is "arrhythmia". Doctors mean cardiac arrhythmias with an irregular heartbeat. If the heart beats too fast, it is called tachyarrhythmia. If the heartbeat is very slow, it is called bradyarrhythmia.
Ventricular arrhythmias
Cardiac arrhythmias are usually classified according to where they occur first. Doctors refer to changes in the heartbeat originating in the chambers of the heart (ventricles) as ventricular arrhythmias. If the excitations arise about it, one speaks of supraventricular cardiac arrhythmias.
Typical ventricular arrhythmias are:
- Extra beats (ventricular extrasystoles)
- Ventricular flutter
- Ventricular fibrillation
- Ventricular tachycardia (e.g. torsade de pointes tachycardia)
Supraventricular arrhythmias
Above all, supraventricular cardiac arrhythmias are further subdivided in some places; namely according to where pathological processes take place in the conduction system:
Normo- or orthotopic irritation disorders are cardiac arrhythmias that originate from the sinus node. The formation of the electrical impulses is changed, for example in:
- Sinus arrhythmia (e.g. sick sinus syndrome)
- Sinus bradycardia (less than 60 beats per minute, sometimes less than 50 beats)
- Sinus tachycardia
Heterotopic irritation disorders originate outside the sinus node. Then the impulses arise either in the atrial muscle itself, in the AV node or in the bundle of His. These include, for example:
- Extra beats (extrasystoles)
- Atrial tachycardias (e.g. in the case of an overactive thyroid)
- Atrial fibrillation / flutter
- AV rhythm / extrasystole (as a secondary pacemaker approx. 40-50 beats per minute)
- His bundle rhythm / extrasystole (as a tertiary pacemaker approx. 30-40 beats per minute)
Conduction disorders exist when the transmission of impulses from the sinus node via the AV node into the heart chamber is disturbed, as in these clinical pictures:
- Sin astrial block (SA block)
- Atrioventricular block (AV block)
- Intraventricular block (e.g. (in) complete right bundle branch block and / or left bundle branch block)
This also includes cardiac arrhythmias that occur like paroxysmal attacks. In this case, some patients have additional "lines" for the electrical impulses.
- AV nodal reentry tachycardia
- AV reentry tachycardia (additional trunk groups as in WPW syndrome)
resuscitation
If the heart stops beating at all, doctors speak of asystole. Sometimes there are also individual electrical discharges, which can also be seen in an EKG, called pulseless electrical activity (PEA). But it is no longer enough for a heartbeat. As with ventricular tachycardias without a pulse or ventricular fibrillation, a PEA or asystole must be resuscitated immediately.
How dangerous are arrhythmias?
Some arrhythmias are harmless, others are life-threatening. If a cardiac arrhythmia persists, it can have several consequences. For example, the heart becomes weaker and weaker (heart failure). The risk of heart attacks also increases. For example, there is a risk of a heart attack because fast-beating hearts consume more oxygen. The heart muscle gets this from the coronary vessels. If the coronary artery or the heart muscle itself are abnormally changed, the oxygen supply is no longer sufficient over time and there is a risk of an undersupply (ischemia).
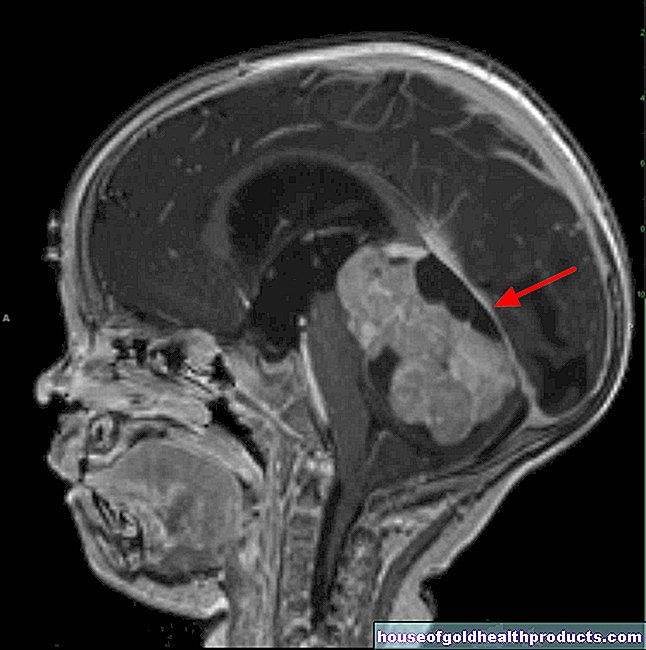
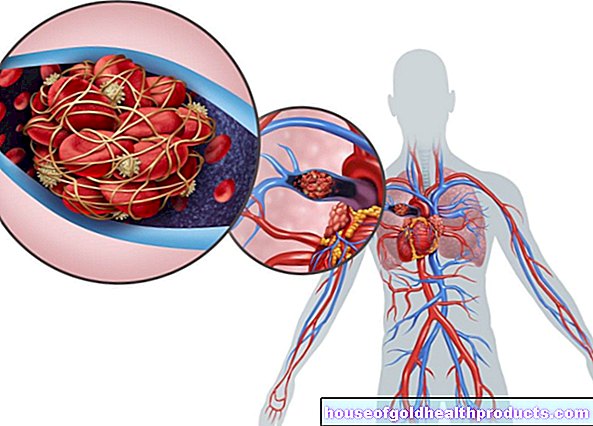
With irregular and rapid cardiac arrhythmias, the blood swirls in some places in the heart. If this condition persists, the blood clumps and a thrombus develops. It can be released from the heart and migrates to other parts of the body via the bloodstream. There the vessels become increasingly narrow, so that the blood clot gets stuck and clogs the vein. As a result, the organ in question or at least parts of it are no longer adequately supplied with oxygen and perish. The consequences are a stroke in the brain, a pulmonary embolism in the lungs or a kidney infarction with subsequent kidney failure.
Cardiac arrhythmias: sport
Especially in children and young people, the heart rate rises and falls when inhaling and exhaling. These changes in heart rate are called respiratory sinus arrhythmias. This process is normal and does not require therapy. During sport, but also in everyday life, there are sometimes extra beats of the heart, so-called extrasystoles. They are sometimes uncomfortable, but usually harmless. In addition, a real athlete's heart is sometimes so well trained that it gets the circulation going properly even with fewer beats. This form of sinus bradycardia also has no disease value.
Arrhythmias: diagnosis
The first point of contact is usually the family doctor. He takes the first steps to get to the bottom of cardiac arrhythmias. For more detailed clarification, however, he will refer you to a specialist in heart disease, a cardiologist. At the beginning, the doctor asks the patient about symptoms:
- Do you often get dizzy? Have you already collapsed?
- Do you keep racing your heart? If so, how often and how long does an attack last?
- Does your heart stumble often?
- Do you occasionally experience shortness of breath or chest pain?
The doctor is also interested in the medical history (in summary, the doctor takes a so-called anamnesis):
- What medications are you taking?
- Do you have any known heart disease?
- Have you ever been treated for cardiac arrhythmias?
- Do you suffer from other diseases, such as a thyroid dysfunction?
The doctor will then examine you. He measures blood pressure and feels the pulse. He also listens to the heart.
Apparative investigations
The doctor records the electrical activity of the heart and thus also cardiac arrhythmias with an electrocardiogram (EKG). Sometimes, however, patients suffer from temporary attacks of a cardiac arrhythmia that do not occur when they visit the doctor. Then a long-term ECG examination is advisable, which continuously registers the heart's actions over a period of around 24 hours.
Under certain circumstances, no cardiac arrhythmias will occur during this period either. Then so-called event recorders can help. There are external and implantable recording devices. They automatically save cardiac arrhythmias that correspond to a certain pattern (this is programmed in beforehand). Some external devices also only save the heart's actions at the push of a button, i.e. when the patient notices anomalies.
Doctors use stress tests to test how cardiac arrhythmias behave during physical exertion. A bicycle ergometer is usually used for this. In addition to the stress ECG, this examination also includes measuring blood pressure. In addition, the examinations can be supplemented with a heart ultrasound (echocardiography).
Doctors often use this to identify underlying heart conditions. This may also be seen in a chest x-ray. In some cases, the doctor will perform an electrophysiological test. In this context, he can not only assess the cardiac arrhythmias well, but also treat them immediately if necessary (catheter ablation).
Cardiac arrhythmias: what helps?
If a rapid heartbeat occurs very suddenly, you can first try to see whether certain maneuvers slow the pulse. For example, you can put an ice pack on your face or neck, or press while holding your breath. This irritates special sensors in the vessels. They give feedback to the central nervous system, which throttles cardiac activity via the vagus nerve.
Sometimes doctors also have to prescribe drugs that prevent or at least contain the cardiac arrhythmias. Depending on the type of cardiac arrhythmia, they are taken permanently or only when the abnormal heartbeat occurs. Choosing the right remedy is complex and depends on many factors. Well-known drugs that are used for cardiac arrhythmias are:
- Beta blockers (controls and generally lowers the heart rate)
- Sodium channel blockers (especially flecainide as "pill in the pocket" for attack-like supraventricular tachycardias)
- Potassium channel blockers (e.g. amiodarone for atrial fibrillation)
- Calcium channel blockers (e.g. verapamil)
- Digitalis (lowers atrial tachycardia, especially good when beta blockers are insufficient or low blood pressure does not allow them to be used)
- Parasympatholytics such as atropine or sympathomimetics such as orciprenaline (for bradycardia)
Sometimes, because of their irregular heartbeat, patients need a pacemaker, defibrillator, or a device that includes both. These devices are implanted under the skin. Wires run from there into the heart in order to set electrical impulses permanently or if necessary. Cardiac resynchronization therapy is mainly used for severe cardiac insufficiency and left bundle branch block. With this device, two probes - one per heart chamber - let the ventricles beat again in the same rhythm.
Doctors can obliterate additional conduction pathways, for example in the case of AV node reentry tachycardia, as part of an electrophysiological examination (high-frequency catheter ablation). This method often prevents recurring cardiac arrhythmias in the long term. Treatment and prognosis do not only depend on the type of illness, but also on comorbidities and symptoms. There are also harmless cardiac arrhythmias (e.g. extrasystoles) that do not have to be treated at all.
Tags: eyes organ systems Diseases