Proctitis
Sophie Matzik is a freelance writer for the medical team.
More about the experts All content is checked by medical journalists.Proctitis (inflammation of the rectum) is inflammation of the last section of the rectum and anus. Proctitis causes symptoms such as bloody, purulent stool or discharge, constant or irregular bowel movements, and severe pain. The causes of proctitis are many; most often it is the result of a bacterial infection. Read everything you need to know about proctitis here - further symptoms, causes and treatment options.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K62K51
Proctitis: description
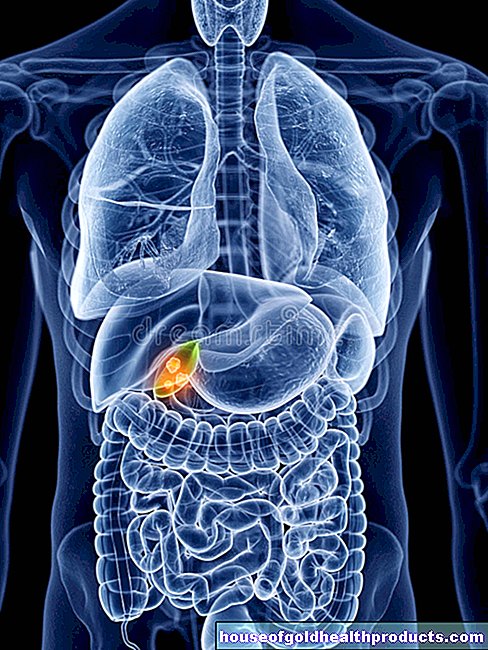
Proctitis (inflammation of the rectum) is inflammation of the last section of the rectum and usually also of the anus. It is accompanied by complaints such as bloody, purulent stool, difficulty with stool and pain in the hip and groin region.
In contrast to other inflammatory bowel diseases, with proctitis the symptoms are limited to the last 15 centimeters of the intestine up to the anus.
The causes of proctitis are many. Bacterial infections (especially during unprotected sexual intercourse), other inflammatory bowel diseases and an allergic reaction to the ingredients of suppositories or condoms are possible. Exact figures on the frequency of proctitis are not yet available.
Proctitis: symptoms
Symptoms rarely occur at the onset of proctitis. At most, those affected notice that the anus is very sensitive or pain occurs when defecating.
After some time while the inflammation spreads in the rectum, the following symptoms may appear:
- bloody purulent discharge
- bloody, purulent stool
- the constant feeling of having to go to the bathroom
- irregular bowel movements
- Fecal incontinence
- Pain and cramps
- Air escapes from the intestines (flatulence)
- Itching of the anus
- reddened, bulging anus
In the further course of proctitis, anal fissures, genital warts or fistulas on the anus, which can also cause severe pain, often occur.
Which complaints occur in individual cases depends to a large extent on which factors caused the proctitis. Proctitis caused by gonorrhea, for example, shows hardly any symptoms.
Proctitis: causes and risk factors
Proctitis can be caused by a variety of factors. Most cases of proctitis are due to unprotected sex, in which the patient contracts an STD. Infections with syphilis, gonorrhea, AIDS, donovanosis (a tropical sexually transmitted disease), genital herpes (genital herpes), chlamydia or the human papilloma virus (HPV) are often associated with proctitis.
People who have frequent anal intercourse or intercourse with different people have a greatly increased risk of developing proctitis. Inserting objects into the anus during sexual intercourse can also tear the intestinal wall. These injuries can also cause proctitis.
In addition, inflammation of the rectum can occur in the context of chronic inflammatory bowel diseases, for example in Crohn's disease or ulcerative colitis. If the inflammation affects only the rectum in ulcerative colitis, doctors speak of ulcerative proctitis.
Proctitis can also result from allergic reactions to the ingredients of suppositories, condoms, or lubricants, or from traumatic events or radiation therapy for cancer.
Proctitis: examinations and diagnosis
To diagnose proctitis, as with other diseases, the doctor will first ask about the medical history (anamnesis). The symptoms described by the patient as well as any existing illnesses can provide initial indications of proctitis. Three examination methods are used for a reliable diagnosis:
Inspection of the anus:
The doctor checks whether there are any inflammatory changes at the anus, such as reddening of the mucous membrane.
Digital rectal exam:
During the digital rectal examination, the doctor feels the anus and the surrounding organs with a finger.
Rectoscopy:
In a rectoscopy, the rectum and anus are examined using a rod-like instrument, the endoscope. With the endoscope, air is introduced into the intestine, which unfolds the folds of the mucous membrane in the rectum. In this way, inflammation can be recognized well. During the examination, smears of the mucous membrane or tissue samples (biopsies) can also be taken. The examination usually takes no longer than five to ten minutes and is at most uncomfortable for those affected, but not painful.
If infection is the cause of proctitis, a reliable diagnosis can only be made in the laboratory. The DNA of the bacteria is detected in the smears obtained from the mucous membrane during rectoscopy.
Proctitis: treatment
The therapy of proctitis depends on the causative factors:
infection
If bacterial infections are the cause of proctitis, attempts are made to fight the pathogens with antibiotics. Alternatively, a cortisone preparation can be applied as a foam. In addition, you should definitely switch to safer sex in order to prevent the infection of other people and future infections of your own.
Inflammatory bowel disease
In the context of a chronic inflammatory bowel disease (ulcerative colitis, Crohn's disease), the anti-inflammatory agent mesalazine is initially administered as a suppository three times a week. If this does not improve, the drug is also given in tablet form. Mesalazine foam or mesalazine enema are also frequently used. In very severe cases of ulcerative proctitis, the inflamed area of the mucous membrane can also be removed.
Drug treatment for inflammatory bowel disease can be lifelong.
allergy
If there is an allergy to latex in condoms or to active ingredients in suppositories, for example, these substances must be avoided in the future. Proctitis caused by an allergy heals itself in most cases. In more severe cases, it can also be treated with mesalazine suppositories.
radiation
Treatment of the proctitis caused by radiation is usually not necessary, as this disease is very mild and in most cases heals on its own.
Symptomatic therapy for proctitis
Suppositories or an intestinal enema (enema) can help against the symptoms of rectal inflammation. With an intestinal enema, water is passed through the anus into the intestine. However, this measure may not be used with certain pre-existing conditions.
process control
In moderate and severe cases of proctitis, control smears of the intestinal mucosa are taken regularly to assess the success of the therapy. This is not necessary for easy gradients.
Proctitis: disease course and prognosis
Out of shame, people with proctitis often wait a long time to see a doctor about their symptoms. The longer the treatment of proctitis is postponed, the higher the risk that the inflammation will develop into a chronic condition and can then only be treated with surgery.
If you see a doctor immediately at the first signs of gastrointestinal discomfort, therapy can begin immediately and the chance of a complete cure is high. In almost all cases of proctitis treated, those affected have a good prognosis and the disease can be completely cured.
In contrast to other inflammatory bowel diseases, the risk of colon cancer is not particularly increased with proctitis.
Can proctitis be prevented?
In general, you cannot prevent proctitis. However, you can reduce the risk of illness by only practicing safe sex. That means: Use a condom and make sure that there are no injuries to the oral mucosa during anal intercourse. Infection-related proctitis can thus be avoided.
Tags: alternative medicine sports fitness healthy workplace