stroke
Updated onMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
A stroke (apoplexy, cerebral stroke) is a sudden circulatory disorder in the brain. She must be treated by a doctor as soon as possible! Otherwise so many brain cells die that the patient suffers permanent damage such as paralysis or speech disorders or even dies. Read everything you need to know about the subject here: What exactly is a stroke and how does it develop? What are the warning signs and what are the possible consequences? How is he treated?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I63I64I61I69
Stroke: quick reference
- What is a stroke A sudden problem with blood flow in the brain
- Important symptoms: acute muscle weakness, paralysis and numbness in one half of the body, sudden visual and speech disorders, acute and very severe headaches, acute dizziness, speech disorders, etc.
- Causes: Reduced blood flow in the brain, usually due to a blood clot (ischemic stroke), more rarely due to cerebral haemorrhage (hemorrhagic stroke)
- Stroke test (FAST test): Ask the patient to smile one after the other (F for face), raise both arms at the same time (A for arms) and repeat a simple sentence (S for speech). If he has problems doing this, there is probably a stroke and you should call the emergency doctor quickly (T as in time).
- First aid: Call an emergency doctor (Tel. 112), calm the patient, loosen tight clothing, raise the upper body (if the patient is conscious), lie on the side in a stable position (if unconscious), resuscitation (if no pulse / no breathing can be determined)
- Treatment: Stabilization and monitoring of vital functions, further measures depending on the cause of the stroke (removal of the blood clot with medication or catheters, surgery for extensive cerebral hemorrhage, etc.), treatment of complications (epileptic seizures, increased intracranial pressure, etc.)
Stroke: description
The stroke is a sudden disturbance of the blood flow in the brain. It is also called apoplexy or apoplexy, stroke, brain insult, apoplectic insult or cerebral insult.
The acute circulatory disorder in the brain means that the brain cells do not receive enough oxygen and nutrients. This is how they die. Failures of brain functions can be the result, such as numbness, paralysis, speech or vision disorders. With rapid treatment, they can sometimes resolve again; in other cases they remain permanent. A severe stroke can also be fatal.
-
Stroke - "Have your carotid artery examined!"
Three questions for
Prof. Dr. med. Christoph Bamberger,
Internist and endocrinologist -
1
Many strokes are considered preventable - how can you take precautions?
Prof. Dr. med. Christoph Bamberger
That depends on your risk factors: In addition to smoking, for example, increased blood pressure, high cholesterol levels or diabetes. A doctor can measure this and decide whether the risk can be reduced through pure lifestyle measures (more conscious diet, weight control, regular exercise), or whether medication is necessary. A special variant of the stroke comes from atrial fibrillation. If you have an irregular pulse, you should also see a doctor!
-
2
Are there any early warning signs to look out for?
Prof. Dr. med. Christoph Bamberger
No, a stroke usually comes out of the blue. Sometimes in a temporary variant, the "TIA" (transitory ischemic attack) with paralysis or speech disorders that completely disappear again. That would be the very last warning. But there is one examination that can tell us a lot about the condition of the blood vessels and thus the risk of stroke: the ultrasound examination of the cervical arteries. Ask your doctor about it.
-
3
Is it bad if a stroke goes unnoticed?
Prof. Dr. med. Christoph Bamberger
Nothing shows the risk of a stroke as clearly as the fact that one has already occurred. The next stroke will not be long in coming, unless you take countermeasures. So yes: you should definitely know if you have ever had a stroke. If in doubt, an MRI scan of the head must be made, which reveals areas of the brain that have died due to a stroke.
-
Prof. Dr. med. Christoph Bamberger,
Internist and endocrinologistIn 2006, the hormone expert founded the Medical Prevention Center Hamburg (MPCH), now Conradia Medical Prevention, of which he is the director to this day.
Stroke: frequency
Every year around 200,000 people in Germany suffer a stroke. Are affected in front of the elderly. As their share in the population is steadily increasing, the number of stroke patients is also likely to rise, experts believe.
Anyone who has ever had a stroke carries an increased risk of another apoplexy. About 40 out of 100 people who have already survived a stroke will get another within ten years. The risk of other cardiovascular diseases (such as heart attacks) is also increased in stroke patients.
Stroke in children
A stroke usually affects older people, but it can also occur at a young age. Even unborn children in the womb can suffer a stroke. Possible causes include, for example, coagulation disorders, heart and vascular diseases. Sometimes an infectious disease also causes a stroke in children.
In Germany around 300 children and adolescents are diagnosed with apoplexy each year. However, experts suspect that the actual number is much higher because the diagnosis of “stroke” is more difficult to make in children. The reason is that brain maturation is not yet complete and a stroke in children therefore often only becomes noticeable months or years later. For example, hemiplegia in newborns only becomes apparent after about six months.
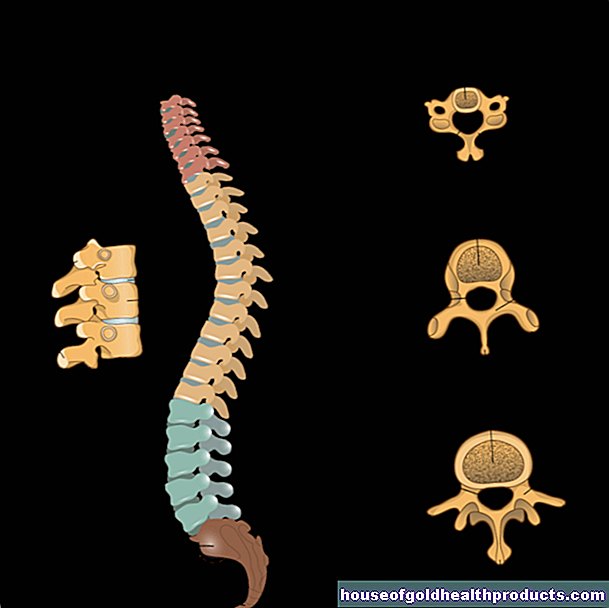
Stroke: symptoms
Stroke symptoms depend on which region of the brain is affected and how severe the stroke is. Acute weakness, numbness and paralysis very often appear in one side of the body. This can be recognized, for example, by the fact that the corner of the mouth and the eyelid are hanging down on one side and / or the patient can no longer move an arm. The left side of the body is affected if the stroke occurs in the right hemisphere, and vice versa. If the patient is completely paralyzed, this indicates a stroke in the brain stem.
Sudden visual disturbances are also common symptoms of stroke: those affected report, for example, that they can only see blurred or that they perceive double vision. Sudden, temporary loss of vision in one eye can also indicate a stroke. The acute visual disturbances can cause the person concerned to fall or - while driving - cause an accident.
An acute speech disorder can also be a sign of a stroke: some patients suddenly speak slurred or slurred, twist letters or can no longer speak at all. Stroke patients can often no longer understand what is being said to them. This is known as a language disorder.
Other possible signs of a stroke may include sudden dizziness and a very severe headache.
You can read more about the signs and symptoms of a stroke in the article Stroke: Symptoms.
Transient ischemic attack (TIA) - the "mini-stroke"
The term "transient ischemic attack" (TIA for short) describes a temporary circulatory disorder in the brain. It is an early warning sign of a stroke and is sometimes called a "mini-stroke".
The TIA is usually caused by tiny blood clots that temporarily impair the blood flow to a brain vessel. The person concerned notices this, for example, from temporary speech or vision disorders. Sometimes weakness, paralysis or numbness occurs in one half of the body for a short time. Temporary confusion or loss of consciousness may also occur.
Such TIA symptoms always appear suddenly and go away after minutes or a few hours. Nevertheless, you should consult a doctor immediately: If the right therapy is initiated quickly, a "real" stroke can often be prevented.
You can read everything you need to know about the "mini-stroke" in the article Transient ischemic attack.
Stroke: causes and risk factors
Doctors differentiate between different causes of strokes: The two most common are reduced blood flow (ischemic stroke) and cerebral haemorrhage (hemorrhagic stroke). In rare cases, other causes of stroke can also be identified.
Stroke cause no. 1: reduced blood flow
Acute under or insufficient blood flow (ischemia) in certain brain regions is the most common of all causes of strokes. It is responsible for about 80 percent of all stroke cases. Doctors speak of an ischemic stroke or cerebral infarction.
There can be different reasons why there is insufficient blood flow in certain areas of the brain. The most important are:
- Blood clots: A blood clot can block a brain vessel and thus cut off the supply of blood and oxygen to a region of the brain. The clot often formed in the heart (for example in the case of atrial fibrillation) or in a "calcified" carotid artery and was washed into the brain with the bloodstream.
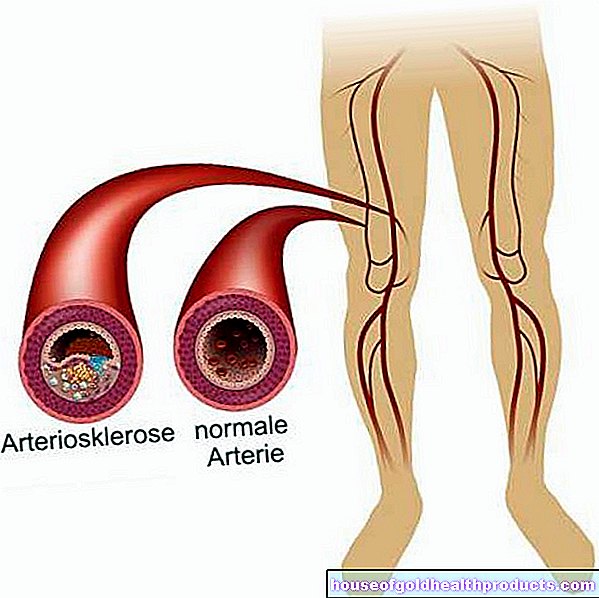
- "Vascular calcification" (arteriosclerosis): cerebral vessels or vessels in the neck supplying the brain (such as the carotid artery) can "calcify": Deposits on the inner wall narrow a vessel more and more or even close it completely. The brain area to be supplied then contains too little blood and oxygen.

An ischemic stroke in the brain stem (brain stem infarction) can have particularly serious consequences. There are vital brain centers that are responsible for controlling breathing, circulation and consciousness. An example of a brainstem infarction is the basilar artery thrombosis, i.e. the occlusion of the basilar artery in the brain stem: in severe cases it causes complete paralysis of all extremities (tetraparesis) and coma or leads directly to death.
Stroke cause # 2: cerebral haemorrhage
Bleeding in the head is the cause of around 20 percent of all strokes. Stroke caused by such a cerebral hemorrhage is also called a hemorrhagic stroke. The bleeding can occur in different places:
- Bleeding in the brain: A vessel suddenly bursts directly in the brain and blood leaks into the surrounding brain tissue. The trigger for this so-called intracerebral hemorrhage is usually high blood pressure. Other diseases, substance abuse, and the rupture of a congenital vascular malformation (such as aneurysm) in the brain can also cause bleeding in the brain. Sometimes the cause remains unexplained.
- Bleeding between the meninges: The stroke occurs here as a result of bleeding in the so-called subarachnoid space: This is the gap-shaped space between the middle meninges (arachnoid) and the inner meninges (pia mater) filled with cerebrospinal fluid. The cause of such a subarachnoid hemorrhage is usually a spontaneously ruptured aneurysm (congenital vascular malformation with bulging of the vascular wall).

Rare causes of strokes
Strokes, especially in younger people, can have other causes than insufficient blood flow or cerebral hemorrhage. In some patients, for example, the stroke is due to inflammation of the walls of the blood vessels (vasculitis). Such vascular inflammation occurs in the context of autoimmune diseases such as giant cell arteritis, Takayasu arteritis, Behcet's disease and systemic lupus erythematosus.
Other rare causes of strokes are, for example, fat and air embolisms: Here fat droplets or air that has penetrated clog a cerebral vessel, resulting in a cerebral infarction. A fat embolism can occur in severe bone fractures when fat-rich bone marrow is washed into the blood. Air embolism can be a very rare complication of open heart, chest, or neck surgery.
Congenital coagulation disorders and the formation of blood clots in the veins are also rare causes of strokes.
Stroke: Risk Factors
Stroke doesn't come out of nowhere. Various factors can contribute to its development. Some of these stroke risk factors cannot be influenced. This includes age: the risk of a stroke increases with age. A genetic predisposition for a stroke cannot be influenced either.
There are also many risk factors that can be specifically reduced. This includes, for example, high blood pressure (hypertension): It leads to "vascular calcification" (arteriosclerosis), which means that deposits form on the inner wall of the vessels. As a result, the vessels become increasingly narrow. This makes a stroke more likely. The following applies: the more severe the high blood pressure, the more likely a stroke becomes.
Another avoidable risk factor for a stroke is smoking: the more cigarettes someone smokes per day and the more years their smoking career has lasted, the higher the risk of a stroke. There are several reasons for this:
Among other things, smoking promotes vascular calcification (arteriosclerosis) and lipid metabolism disorders - both of which are further risk factors for a stroke. Smoking also causes the blood vessels to constrict. The resulting rise in blood pressure favors a stroke.
Smoking also reduces the amount of oxygen that red blood cells (erythrocytes) can carry. The tissues and organs get less oxygen as a result, as does the brain. This then signals to the bone marrow to produce more red blood cells for oxygen transport. Due to the increase in erythrocytes, however, the blood is “thickened”. This makes it harder for it to flow through the narrowed vessels.
Last but not least, smoking increases the willingness of the blood to clot - mainly because the platelets become stickier. This makes it easier for blood clots to form, which can clog a vessel. If this happens in the brain, it results in an ischemic stroke.
So it pays to quit smoking. Five years after quitting smoking, someone is at the same risk of stroke again as people who have never smoked.
Other important risk factors for a stroke are:
- Alcohol: Drinking a lot of alcohol - whether regularly or rarely - increases the risk of a stroke. Above all, the risk of cerebral hemorrhage increases. In addition, regular consumption of alcohol harbors other health risks (such as addictive potential, increased risk of cancer).
- Obesity: Obesity increases the risk of many different diseases. In addition to diabetes and high blood pressure, this also includes a stroke.
- Sedentary lifestyle: Possible consequences are obesity and high blood pressure. Both of these promote a stroke.
- Lipid metabolism disorders: LDL cholesterol ("bad" cholesterol) and other blood lipids are part of the deposits that form on the inner walls of blood vessels in arteriosclerosis. High blood lipid levels (such as high cholesterol levels) therefore increase the risk of stroke through arteriosclerosis.
- Diabetes: Diabetes mellitus damages the blood vessel walls, causing them to thicken. This affects the blood flow. In addition, diabetes aggravates existing arteriosclerosis. Overall, diabetics are two to three times more likely to have a stroke than people who are not diabetic.
- Atrial fibrillation: This arrhythmia increases the risk of stroke because blood clots easily form in the heart. These can - when carried away by the bloodstream - block a vessel in the brain (ischemic stroke). This risk is even greater if there are other heart diseases such as coronary heart disease (CHD) or heart failure.
- Other cardiovascular diseases: Other cardiovascular diseases such as smoker's leg (PAD) and "impotence" (erectile dysfunction) also increase the risk of stroke.
- Narrowed carotid artery (carotid stenosis): It is mostly due to vascular calcification (arteriosclerosis) and often causes no symptoms for a long time. A possible early symptom is a TIA (transient ischemic attack). Asymptomatic or not, carotid stenosis increases the risk of ischemic stroke (cerebral infarction).
- Aura migraines: Strokes caused by reduced blood flow often occur in people who suffer from migraines with aura. The headache is preceded by neurological symptoms such as impaired vision or sensation. The exact relationship between aura migraines and stroke is not yet known. Women are particularly affected.
- Hormone preparations for women: taking the contraceptive pill increases the risk of stroke. This is especially true for women with other risk factors such as high blood pressure, smoking, obesity or aura migraines. Taking hormone preparations during menopause (hormone replacement therapy, HRT) also increases the risk of a stroke.
Child stroke: causes
Stroke in children is rare, but it does happen. While lifestyle factors and lifestyle diseases (smoking, arteriosclerosis, etc.) are the main reasons for a stroke in adults, children have other causes of stroke. These include, for example, an inherited tendency to clot, red blood cell disorders (such as sickle cell anemia) and connective tissue disorders (such as Fabry disease). Autoimmune diseases of the blood vessels and heart diseases are also possible causes of strokes in children.
Stroke: examinations and diagnosis
Whether a severe or mild stroke - every stroke is an emergency! If you even suspect you should call the emergency doctor immediately (Tel. 112)! With the FAST test, you can quickly and easily check a suspected stroke. The stroke test works like this:
- F for "face": Ask the patient to smile. If the face is twisted on one side, this indicates hemiplegia as a result of a stroke.
- A for "arms": Ask the patient to extend their arms forward at the same time while turning their palms upward. If he has problems doing this, it is probably due to incomplete paralysis of one side of the body as a result of a stroke.
- S for "speech": Ask the patient to repeat a simple sentence. If he is unable to do this, or if his voice sounds slurred, there is probably a speech disorder caused by a stroke.
- T for "time": Call the ambulance immediately!

The emergency doctor will check the patient's consciousness, blood pressure and heart rate, among other things. If he is conscious, the doctor can ask about what is happening and any symptoms (such as visual disturbances, numbness or paralysis).
After admission to the hospital, a neurologist is the specialist in charge of suspected stroke. He's doing a neurological exam. For example, he checks the patient's coordination, language, vision, touch and reflexes.
As a rule, a computed tomography of the head (cranial computed tomography, cCT) is done immediately. The examination is often supplemented by a vascular imaging (CT angiography) or a blood flow measurement (CT perfusion). The images from inside the skull show whether a vascular occlusion or cerebral hemorrhage is responsible for the stroke. You can also determine its location and extent.
Sometimes magnetic resonance imaging (MRI, also called magnetic resonance imaging) is used instead of computed tomography. It can also be combined with a vascular display or blood flow measurement.
In some patients, a separate x-ray examination of the vessels (angiography) is carried out. Vascular imaging is important to identify vascular malformations (such as aneurysms) or vascular leaks, for example.
A special ultrasound examination (Doppler and duplex sonography) of the vessels supplying the brain, such as the carotid artery, can also be carried out to clarify a stroke. The doctor can recognize whether there are "calcifications" (arteriosclerotic deposits) on the inner wall of the vessel. They may be the site of a blood clot that was swept away in the bloodstream and caused the stroke.
An ultrasound examination of the heart cavities (echosonography) can reveal heart diseases that favor the formation of blood clots, for example deposits on the heart valves. Sometimes blood clots are found in the heart cavities. You could cause another stroke. Therefore, the patient must be given blood-thinning medication to dissolve the blood clots.
Another important cardiac examination after a stroke is electrocardiography (EKG). This means measuring the electrical currents of the heart. Sometimes it is also carried out as a long-term measurement (24-hour ECG or long-term ECG). The doctor can use the ECG to identify any cardiac arrhythmias. They are also an important risk factor for ischemic insult.
Blood tests are also important when diagnosing a stroke. For example, the blood count, blood clotting, blood sugar, electrolytes and kidney values are determined.
The investigations mentioned serve not only to confirm the suspicion of an apoplexy and to clarify it in more detail. They also help to identify possible complications at an early stage, for example blood pressure crises, heart attacks, pneumonia caused by inhaling food residues (aspiration pneumonia) and kidney failure.
Stroke: treatment
In stroke treatment, every minute counts, because the “time is brain” principle applies: brain cells that - depending on the type of stroke - are not adequately supplied with blood or are squeezed by increased intracranial pressure, die quickly. Stroke patients should therefore get medical help as soon as possible!
Stroke: first aid
If you suspect a stroke you should call the emergency doctor immediately (emergency number 112)! Until this arrives, you should reassure the patient. Raise your upper body a little and open up tight clothing (such as a collar or tie). That makes breathing easier. Do not give him anything to eat or drink!
If the patient is unconscious but breathing, place them in the stable lateral position (on the paralyzed side). Check his breathing and pulse regularly.
If you cannot find any signs of breathing, you should turn the person on their back immediately and begin cardiopulmonary resuscitation (chest compressions and possibly mouth-to-mouth resuscitation).
Acute medical treatment for every stroke includes monitoring vital functions and other important parameters and, if necessary, stabilizing them. These include breathing, blood pressure, heart rate, blood sugar, body temperature, brain and kidney function as well as water and electrolyte balance. Further measures depend on the type of stroke and any complications.
Stroke: treatment for cerebral infarction
Most cerebral infarctions (ischemic strokes) result from a blood clot blocking a vessel in the brain. This has to be eliminated quickly in order to restore the blood circulation in the relevant brain area and to save nerve cells from destruction. The blood clot can either be dissolved with a drug (lysis therapy) or removed mechanically (thrombectomy). Both methods can also be combined with one another.
Lysis therapy
In so-called systemic lysis, the stroke patient is given a drug that can dissolve blood clots (thrombolytic) via an infusion into a vein. The active ingredient rtPA (“recombinant tissue plasminogen activator”) is used. This activates an enzyme in the body that breaks down blood clots. This form of lysis therapy is approved up to 4.5 hours after the cerebral infarction. The earlier the lysis is started within this time window, the higher the chances of success.
If more than 4.5 hours have passed, the clot can hardly be dissolved with medication. Nevertheless, in certain cases a systemic lysis with rtPA can be carried out up to 6 hours after the onset of the stroke symptoms - as an individual healing attempt.
Lysis therapy must not be carried out in the event of a stroke caused by cerebral haemorrhage. That could make the bleeding worse. Lysis therapy is also not recommended in certain other situations, for example in the case of uncontrollable high blood pressure.
In addition to systemic lysis therapy, there is also local lysis (intra-arterial thrombolysis). A catheter is pushed through an artery to the location of the vascular occlusion in the brain and a clot-dissolving drug (such as pro-urokinase) is injected directly. However, local lysis therapy is only suitable in very specific cases (such as brainstem infarction).
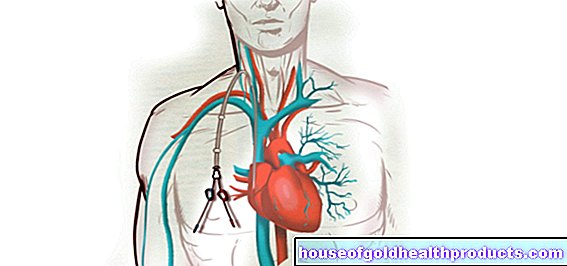
Thrombectomy
Another form of stroke treatment is based on the mechanical removal of the blood clot: In the so-called thrombectomy, a thin catheter is pushed through an artery in the groin to the clot in the brain under X-ray control. This is then removed with suitable fine instruments. The thrombectomy should be performed as soon as possible after the stroke symptoms appear.
Combination of thrombolysis and thrombectomy
It is also possible to combine both procedures - dissolving the blood clot in the brain with a drug (thrombolysis) and removing the clot mechanically using a catheter (thrombectomy).
Stroke: treatment for cerebral haemorrhage
If the stroke is triggered by a minor cerebral hemorrhage, conservative stroke treatment is usually sufficient. Patients must keep bed rest and avoid any activity that increases pressure in the head. This includes, for example, strong pressing when defecating. That is why patients are given laxatives.
It is also very important to monitor blood pressure and treat it if necessary. Too high a pressure increases the bleeding, while too low a pressure could lead to insufficient blood flow in brain tissue.
Surgery is usually necessary for cerebral hemorrhages that are extensive and do not stop on their own. The decision to have an operation depends on various factors such as the location and size of the bleeding, the age and general condition of the patient and any concomitant diseases. During the procedure, the skull is opened in order to clear out the bruise (haematoevacuation) and to close the source of the bleeding as far as possible.
Stroke: treating complications
Stroke treatment includes other measures as needed, especially if complications arise.
Increased intracranial pressure
A very large cerebral infarction can cause the brain to swell (cerebral edema). Because the space in the bony skull is limited, intracranial pressure increases as a result. Nerve tissue can be squeezed and irreversibly damaged as a result.
Even with a major cerebral hemorrhage, the escaping blood can increase the pressure in the skull. When blood enters the interior of the brain (ventricle) that is filled with nerve water, the nerve water can also build up - a "water head" (hydrocephalus) develops. This also causes intracranial pressure to rise dangerously.
Whatever the reason for increased intracranial pressure, it is imperative that it be decreased. For this purpose, for example, the patient's head and upper body are raised. It also makes sense to give draining infusions or drain off nerve water via a shunt (e.g. into the abdominal cavity). A part of the skull bone can also be temporarily removed to relieve the strain and reinserted later (relief craniotomy). Removing the bruise from a cerebral hemorrhage also reduces the pressure in the skull.
Vasospasm
In the event of a stroke caused by bleeding between the meninges (subarachnoid haemorrhage), there is a risk that the vessels will narrow in a spasmodic manner. As a result of these vascular spasms (vasospasms), the brain tissue can no longer be adequately supplied with blood. Then an ischemic stroke can also occur. Vascular spasms must therefore be treated with medication.
Epileptic seizures and epilepsy
Stroke is very often the cause of new epilepsy in elderly patients. An epileptic seizure can occur within the first hours after the stroke, but also days or weeks afterwards. Epileptic seizures can be treated with medication (with anti-epileptic drugs).
lung infection
One of the most common complications after a stroke is bacterial pneumonia. The risk is particularly high in patients who suffer from swallowing disorders (dysphagia) as a result of a stroke: If swallowed, food particles can get into the lungs and cause pneumonia (aspiration pneumonia). Antibiotics are given for prevention and treatment. Stroke patients with swallowing disorders can also be fed artificially (through a tube). This lowers the risk of pneumonia.
Urinary tract infections
In the acute phase after a stroke, patients are often unable to urinate (urinary retention or urinary obstruction). Then a urinary catheter has to be inserted repeatedly or permanently. Both urinary obstruction and indwelling catheters promote urinary tract infection after a stroke. They are treated with antibiotics.
Stroke rehab
Medical rehabilitation after a stroke aims to help a patient return to their old social and possibly also professional environment. For this purpose, for example, suitable training methods are used to try to reduce functional restrictions such as paralysis, speech and speech disorders or visual disorders.
In addition, rehabilitation after a stroke should enable a patient to cope with everyday life as independently as possible. This includes washing, getting dressed or preparing a meal by yourself, for example. Sometimes there are physical restrictions (such as a paralyzed hand) that make certain hand grips or movements difficult or impossible. In stroke rehabilitation, those affected then learn solution strategies and how to use suitable aids (such as bath lifts, walking sticks, ankle braces).
Inpatient or outpatient
Neurological rehabilitation can be carried out as an inpatient, especially in the early stages after a stroke, for example in a rehab clinic. The patient receives an individual treatment concept and is cared for by an interdisciplinary team (doctors, nurses, occupational and physiotherapists, etc.).
In semi-inpatient rehabilitation, the stroke patient comes to the rehab station on weekdays for his therapy sessions. But he lives at home.
If interdisciplinary care is no longer necessary, but the patient still has physical functional limitations in certain areas, outpatient rehabilitation can help. The respective therapist (such as occupational therapist, speech therapist) regularly comes to the stroke patient's home to practice with them.
Motor rehabilitation
Sensorimotor disorders are one of the most common impairments after a stroke. This is understood to mean a disturbed interplay of sensory performance (sensory impressions) and motor performance (movements). Usually it is the incomplete paralysis in one half of the body (hemiparesis). Various forms of therapy can help to improve such sensorimotor disorders. Here are some key examples:
In the rehabilitation of hemiplegia, the Bobath concept is very often used: the paralyzed part of the body is persistently promoted and stimulated. For example, the patient is not fed, but the spoon is brought to the mouth together with him and the impaired arm. The Bobath concept must also be implemented in every other activity in everyday life - with the help of doctors, nurses, relatives and all other carers. Over time, the brain can reorganize itself in such a way that healthy parts of the brain gradually take over the tasks of the damaged brain areas.
Another approach is Vojta therapy. It is based on the observation that many human movements are reflexive, such as reflexive grasping, crawling and turning around in babies. This so-called reflex locomotion is still present in adults, but is normally suppressed by conscious movement control.
With the Vojta method, such reflexes are specifically triggered. For example, the therapist stimulates certain pressure points on the patient's trunk, which causes spontaneous muscle reactions (for example, the trunk automatically straightens up against gravity). With regular training, disturbed nerve tracts and certain movement sequences are to be reactivated in this way.
Proprioceptive Neuromuscular Facilitation (PNF) aims to promote the interaction of nerves and muscles via external (exteroceptive) and internal (proprioceptive) stimuli. First, the patient is questioned and examined in detail by the therapist. His movement behavior as well as related restrictions and disorders are precisely analyzed. On this basis, the therapist creates an individual treatment plan, which is repeatedly checked over the course of the therapy and adjusted if necessary.
Treatment according to PNF is based on certain defined movement patterns in the shoulder and hip joint area, which are based on everyday functions. The exercises are repeated continuously so that the movement is increasingly effective and coordinated. Patients are also encouraged to practice regularly at home.
Cognitive therapeutic exercises according to Perfetti are particularly suitable for neurological disorders and hemiplegia. The patient should relearn the movement sequences and regain the lost control of movement. To do this, he first has to feel movements: With his eyes closed or behind a screen, targeted movements are made, for example with the hand or foot, which the patient should consciously feel. Initially, the therapist guides the patient's hand or foot to avoid false patterns. Later, the patient performs the movements himself, but is still supported or corrected by the therapist. After all, the stroke patient learns to perform more difficult movement sequences on their own and to control disorders via the brain.
"Forced-use" therapy is also called "Constrained Induced Movement".It is usually used to exercise a partially paralyzed arm and hand, and sometimes the lower limb as well. In some of those affected, the damaged brain area regenerates over time to such an extent that the diseased part of the body gradually becomes more functional again. The problem: The affected person has completely forgotten how to move the sick limbs and therefore hardly uses them or does not use them at all.
This is where the “forced use” therapy comes in: by forcing the patient to use the affected limb, it should be largely reactivated. This requires strenuous training of the partially paralyzed limb. For example, the participants practice special movements in constant repetition. Frequent use expands the area of the brain that is responsible for that part of the body and creates new nerve connections.
"Forced-use" therapy is more promising than conventional physiotherapy in the treatment of motor failures after a stroke.
Rehabilitation for swallowing disorders
Swallowing disorders (dysphagia) are another common consequence of a stroke. With the right therapy, the sufferer should regain the ability to eat and drink. At the same time, the risk of choking should be reduced. To achieve this, there are three different therapy methods that can also be combined with one another:
- Restorative (restorative) procedures: With the help of stimulation, movement and swallowing exercises, an attempt is made to eliminate the swallowing disorder. This can be achieved, for example, if other brain areas take over the task of the damaged brain area in whole or in part.
- Compensatory procedures: Changes in posture and anti-swallowing techniques are designed to reduce the risk of the patient choking. If food residues or liquids land in the lungs, coughing attacks, attacks of suffocation or pneumonia (aspiration pneumonia) occur.
- Adaptive procedures: The diet is adapted in such a way that it is easier for patients with swallowing disorders to eat and drink. For example, food is pureed and drinks are thickened. Therapy aids such as special drinking cups or special cutlery are used as support.
Cognitive rehabilitation
Cognitive rehab after a stroke tries to improve impaired cognitive functions such as language, attention or memory. As with the treatment of swallowing disorders, rehabilitation can also be aimed at restitution, compensation or adaptation. Very different therapy methods are used.
For example, computer-aided training methods can be helpful in the case of attention, memory and visual disorders. In the case of memory disorders, learning strategies can improve memory performance and aids such as a diary can offer a means of compensation. Medicines are also used in certain cases.
Prevention of another stroke
Whenever possible, existing causes and risk factors for stroke must be eliminated or at least reduced in every patient. This helps prevent another stroke (secondary prophylaxis). For this purpose, medication must often be taken for life. Non-drug measures are also important for secondary prophylaxis.
"Blood thinners" (platelet aggregation inhibitors): After a stroke caused by reduced blood flow or a TIA ("mini-stroke"), most patients receive so-called platelet function inhibitors. These include, for example, acetylsalicylic acid (ASA) and clopidogrel. These "blood thinners" prevent platelets from clumping together into a plug that may then clog a vessel again. If possible, the medication should be taken for life.
By the way: ASA can cause gastric or duodenal ulcers as a side effect. Affected patients therefore often have to take a so-called proton pump inhibitor ("stomach protection") in addition to ASA.
Anticoagulants (anticoagulants): A stroke caused by reduced blood flow (ischemic stroke) or a TIA ("mini stroke") often occurs as a result of atrial fibrillation. With this cardiac arrhythmia, blood clots form very easily in the heart, which are then carried away by the bloodstream and block a vessel in the brain. To prevent this from happening again, stroke patients with atrial fibrillation are given anticoagulant medication in tablet form (oral anticoagulants). These drugs block the complicated process of blood clotting and thus the formation of clots.
Cholesterol lowering drugs: One of the main causes of stroke is calcification of the blood vessels (arteriosclerosis). Part of the calcium deposits on the inner wall of the blood vessels is cholesterol. After a stroke caused by reduced blood flow (ischemic apoplexy) and after a "mini-stroke" (TIA), patients therefore usually receive cholesterol-lowering drugs from the group of statins (CSE inhibitors). These prevent an existing arteriosclerosis from progressing further.
In the event of a stroke caused by cerebral haemorrhage, cholesterol-lowering drugs are only prescribed if necessary and after careful risk-benefit analysis.
Antihypertensive drugs (antihypertensive drugs): High blood pressure patients must take long-term antihypertensive drugs after an ischemic stroke or TIA. This should prevent another stroke. The attending physician decides on a case-by-case basis which antihypertensive agent is most suitable (ACE inhibitor, beta blocker, etc.) and which target blood pressure value is aimed for.
Non-drug measures: Some risk factors for another stroke can be reduced (supportively) even with non-drug measures. We recommend, for example, reducing excess weight, regular exercise, a balanced diet with little animal fat and abstaining from nicotine and alcohol. Such a lifestyle helps, among other things, to get high blood pressure and cholesterol levels under control. This significantly lowers the risk of another stroke.
Stroke: Stroke Unit
The term "stroke unit" refers to a special department in a hospital whose employees specialize in the diagnosis and acute treatment of people with a stroke. Care on such a "stroke ward" has been shown to improve the patient's chances of survival and reduce the risk of permanent damage.
The patients stay in the stroke unit for an average of three to five days. Then they are transferred to another ward (neurological ward, general ward) or referred directly to a rehabilitation facility as required.
There are now more than 280 "stroke units" in Germany. They are certified by the German Stroke Help.
You can find out more about this in the article Stroke Unit.
Stroke: disease course and prognosis
In general, the following applies: The brain damage caused by a stroke is all the more serious, the larger the affected blood vessel, which has been blocked or has burst. However, even small damage can have devastating effects in particularly sensitive brain regions such as the brain stem.
Around a fifth (20 percent) of all stroke patients die within the first four weeks. More than 37 percent of those affected die in the course of the first year. Overall, after heart attacks and cancer, strokes are the third most common cause of death in Germany.
Of those stroke patients who are still alive after a year, about half suffer permanent damage and are permanently dependent on outside help. In Germany that is almost a million people.
A stroke in children has a very good chance of recovery. There are good treatment options for the little patients so that after a while most of them can return to normal lives. The stroke leaves a major negative impact on only around ten percent of all affected children.
Stroke: consequences
Many patients have permanent impairments after a stroke. These include, for example, movement disorders such as an unsteady gait or hemiplegia. Some patients have difficulty coordinating their movements (such as writing) or performing complex movements (such as opening a letter).
The possible consequences of a stroke also include language and speech disorders: With a language disorder, those affected have problems formulating their thoughts (verbally or in writing) and / or understanding what others are saying to them. In contrast, the motoric articulation of words is impaired in the case of a speech disorder.
Other common consequences of a stroke are, for example, impaired attention and memory, as well as impaired vision and swallowing. You can read more about this in the article Stroke: Consequences.
Living with a Stroke
After a stroke, nothing is often the same as it was before. Consequential damage such as visual and speech disorders as well as hemiplegia can affect the whole of everyday life. For example, after a stroke, the ability to drive can be so severely impaired that it is better for patients not to sit behind the wheel. But even those who are apparently fit should voluntarily inform the driver's license office about the stroke and submit a medical report. The authorities may require additional driving lessons or a conversion of the vehicle.
For younger people, after a stroke, the question arises whether it is possible to return to work or whether retraining is necessary. Even vacation trips often require special compromises and adjustments after a stroke.
Life after a stroke is also a challenge for loved ones. It's about supporting the patient in everyday life as much as possible, but not relieving him of everything.
You can read more about the challenges of everyday life after a stroke in the article Living with a stroke.
Prevent stroke
Various risk factors contribute to the development of a stroke. Many of them can be specifically reduced or even eliminated entirely. This effectively prevents a stroke.
For example, it is important to have a balanced diet with plenty of fruit and vegetables. On the other hand, you should only consume fat and sugar in moderation. With this healthy diet, you prevent vascular calcification (arteriosclerosis) - this is one of the main causes of stroke.
Regular exercise and sport also keep the blood vessels healthy and prevent a stroke. If you are overweight, you should lose weight. Excess pounds increase the risk of high blood pressure and arteriosclerosis. Both of these promote a stroke.
Another great tip to prevent stroke is to avoid nicotine and alcohol.
Read more about how you can reduce the risk of stroke in the article Preventing a stroke.
Additional information
Book recommendations:
- Stroke: Life afterwards: Expert tips for people with a stroke and other damage to the central nervous system (Rainer Schulze-Muhr, CreateSpace Independent Publishing Platform, 2017)
- When the blow hit me: Back to life after a stroke (Gabo, W. Zuckschwerdt Verlag, 2013)
Guidelines:
- S1 guideline "Acute Therapy of Ischemic Stroke" of the German Society for Neurology
- S3 guideline "Secondary prophylaxis of ischemic stroke and transient ischemic attack" of the German Stroke Society and the German Society for Neurology
- S2k guideline "Acute Therapy of Ischemic Stroke - Amendment 2015: Recanalizing Therapy" of the German Society for Neurology
Support groups
German Stroke Foundation
https://www.schlaganfall-hilfe.de//adressen-selbsthilfegruppen









.jpg)