Scleroderma
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Scleroderma is a connective tissue disease of unknown origin. Typically there is a thickening and hardening of the skin. Scleroderma occurs in two forms: affecting only the skin (circumscribed scleroderma) or affecting the entire body (systemic scleroderma). Read here what symptoms occur and how the disease progresses!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M34

Brief overview
- What is scleroderma ?: Connective tissue disease, two forms: localized and systemic scleroderma
- Symptoms: thickening of the skin, Raynaud's syndrome, masked face, joint and muscle pain
- Course and prognosis: Depending on which organs are affected
- Treatment: incurable, depending on the organ affected
- Causes and risk factors: autoimmune disease of unknown cause, genetic predisposition
- Examination and diagnostics: examination of skin and nail folds, blood tests, ultrasound, x-rays, computed tomography, magnetic resonance tomography, electrocardiogram
- Prevention: No known preventive measures
What is Scleroderma?
Scleroderma is a group of diseases in which the skin and connective tissue thicken and harden. If the symptoms are limited to the skin, one speaks of circumscribed scleroderma. If internal organs such as the lungs, intestines, heart or kidneys are also affected, it is known as systemic scleroderma (also: progressive systemic sclerosis).
Forms of scleroderma
Scleroderma is a combination of the Greek words "sclero" (hard) and "derma" (skin). This name describes the main symptom of the disease: a thickened and hardened skin.
Scleroderma is triggered by a disease of the connective tissue. Because this tissue is found almost everywhere in the body, scleroderma usually not only affects the skin, but spreads throughout the body. Depending on which organs are affected, there are two types of scleroderma.
Systemic sclerodomy
In systemic scleroderma (also known as progressive systemic sclerosis), the disease is not limited to the skin, but also affects other organs.
Diffuse form: the changes affect all parts of the body, including the internal organs.
Limited form: The skin changes are only found from the fingers to the elbow or from the toes to the knee. Other parts of the body such as the chest, abdomen and back remain exposed, and the head is rarely affected. Systemic scleroderma may extend to the internal organs.
Systemic sclerosis sine scleroderma: It is a special form of sclerosis, because the changes are found in the organs, but not on the skin.
Overlap syndrome: Doctors speak of overlap syndrome if another (autoimmune) disease such as lupus erythematosus or rheumatoid arthritis occurs in addition to one of the forms mentioned.
Circumscribed sclerodomy
The circumscribed scleroderma is also called morphea. It is characteristic of this form that the changes only affect the skin. Internal organs are not involved.
Depending on the extent and depth of the skin changes (plaques), circumscribed scleroderma is divided into four forms:
- Limited form
- Generalized form
- Linear shape
- Deep circumscribed scleroderma (Deep morphea)
Incidence of scleroderma
Scleroderma is a rare disease: less than 50 people per 100,000 people develop it each year.
Around 1,500 people are diagnosed with "systemic sclerosis" each year, and an estimated 25,000 people live in Germany. The first symptoms most often appear between the ages of 50 and 60, and in some cases not until after the age of 65. Women are four times more likely than men to develop scleroderma.
The "circumscribed sclerosis" occurs somewhat more frequently: around 27 per 100,000 inhabitants develop it every year. Women are three times more likely to be affected than men. The first symptoms usually appear between the ages of 20 and 40. If children are affected, the first symptoms appear around the age of eight.
How do I recognize scleroderma?
Symptoms of systemic scleroderma
With systemic scleroderma, symptoms all over the body are possible. The following symptoms typically arise:
- Raynaud's Syndrome:
The first symptom of systemic scleroderma is what is known as Raynaud's syndrome in almost all patients (90 percent of all cases). The fingertips (more rarely the toes) turn white, feel cold and numb. Raynaud's syndrome occurs primarily when it is cold, but also when it is stressed: The small blood vessels in the fingertips cramp, which means that the fingers are no longer supplied with sufficient blood. If the cramps resolve again, those affected often feel severe pain.
Raynaud's syndrome is often the first symptom of systemic scleroderma. See a doctor as quickly as possible if you experience these symptoms!
- Changes to the skin:
Hardening and scarring are found in almost all patients with systemic scleroderma, in principle on every skin site.
The hands are particularly often affected. There is swelling and redness on the fingers, which sometimes turn bluish in color. The skin thickens, especially around the finger joints, and the fingers can no longer be moved as easily. The skin becomes more and more taut, itches and has a waxy sheen. Skin folds are difficult to lift off. Those affected report the feeling of wearing a glove that is too tight.
The skin changes often also affect the face: if the skin on the face thickens in scleroderma, facial expressions are severely restricted (masked face). Scarring on the face often affects the eyelids as well. In addition, there is a narrowing of the mouth. Gradually, it opens only to a limited extent, and there are also longitudinal folds around the mouth (so-called purse-string folds). The lips become thin, the frenulum becomes shorter due to scarring. In three quarters of all patients, the face and cleavage are noticeably reddened (telangiectasia).
- Involvement of the joints:
Sometimes there are painful calcifications near small joints, which can be felt as hard knots. This is due to the build-up of calcium salts under the skin.
- Involvement of the muscles:
If the muscles are also affected by scleroderma, pain typically occurs when moving. Sufferers report that their muscles tire quickly and that they feel powerless.
- Damage to the internal organs:
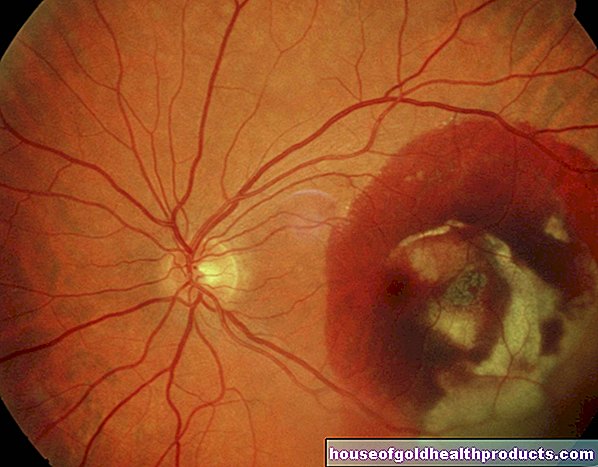
Lungs: After the skin, the lungs are most commonly affected. The build up of connective tissue can damage the lungs. Those affected develop, for example, pulmonary fibrosis or pulmonary hypertension (pulmonary arterial high pressure, PAH). Symptoms of such diseases are shortness of breath and cough.
Heart: Scleroderma damages the heart in 15 percent of all cases. The most common inflammation of the heart muscle or pericardium. If left untreated, this can lead to life-threatening cardiac insufficiency or cardiac arrhythmias.
Typical signs that the heart is also affected are chest pain, strong heart palpitations, fainting spells, or swollen legs.
Kidney: Since the kidneys regulate blood pressure, among other things, high blood pressure is a common side effect of scleroderma. In severe - and very rare - cases, kidney failure occurs.
Digestive tract: Symptoms that occur in the digestive tract with scleroderma include gas or constipation. Dry mouth and heartburn are other possible complaints.
- More symptoms
Systemic scleroderma can affect the entire body. The symptoms are correspondingly diverse and unspecific: They range from tiredness to sleep problems and hoarseness.
Symptoms of circumscribed scleroderma
In circumscribed (demarcated) scleroderma, only the skin is affected. Internal organs are not affected. In contrast to systemic sclerosis, Raynaud's syndrome does not occur either.
- Limited form:
The skin changes are larger than two centimeters and are located in one or two places on the body, usually on the trunk (chest, stomach, back).
- Generalized form:
The lesions appear in at least three places, often on the trunk and thigh, and are often symmetrical.
- Linear shape:
The skin changes are band-shaped and run in the longitudinal direction of the body. The best-known form is called "En coup de saber": Here the skin thickens from the eyebrows to the hairline. The hair falls out in the affected areas and scars form. Often the brain below is also affected.
- Deep circumscribed scleroderma (Deep morphea):
In this very rare form, the indurations are found in the fatty tissue and in the muscles. It occurs symmetrically on the arms and legs and often begins in childhood. A typical symptom is muscle pain.
How Long Can You Live With Scleroderma? Is Scleroderma Fatal?
Scleroderma affects everyone differently. The disease usually develops slowly over many years, sometimes it starts quickly and violently. It is constant in one patient and in spurts in another. In this case, after years of symptom-free phases, there is always an acute flare-up in which the symptoms worsen. It is difficult to predict how scleroderma will progress individually.
Circumscribed scleroderma
Scleroderma is incurable, but the symptoms can be treated well. In circumscribed scleroderma, the indurations are limited to the skin. Those affected therefore have the same life expectancy as those who do not have the disease. In some cases the disease heals on its own.
Systemic scleroderma
In systemic sclerosis, the prognosis depends on which organs are affected and how severely. The disease is rarely life-threatening. The successes of treatment have made great strides in recent years, so that it is often possible to slow down the course of the disease. In this way, severe flare-ups can often be avoided altogether.
According to statistics, the so-called 10-year survival rate for systemic scleroderma is currently 70 to 80 percent. This means that 70 to 80 percent of patients are still alive ten years after diagnosis.
If the lungs are affected by scleroderma, the prognosis is usually worse. The most common causes of death in scleroderma are pulmonary hypertension and pulmonary fibrosis.
The lungs of patients with scleroderma are thoroughly examined once a year so that countermeasures can be taken as early as possible. In addition, the doctor regularly checks the blood and heart.
What can you do about scleroderma?
According to the current state of knowledge, scleroderma is not curable. Depending on which organ is affected, the doctor uses different treatments. This slows the progression of the disease and alleviates the symptoms.
Treatment of systemic scleroderma
A cure for systemic scleroderma is not yet possible. However, it can alleviate the symptoms of the disease and delay its progression. Doctors therefore also speak of symptomatic treatment (as opposed to causal treatment).
The therapy depends primarily on which organs are affected by the scleroderma and which symptoms are to be alleviated.
If Raynaud's syndrome is present, the hands and feet should be protected from the cold. In addition, the doctor will prescribe vasodilator or blood-thinning medication if necessary. So-called calcium channel blockers such as nifedipine for mild symptoms and iloprost for severe symptoms improve blood circulation. They widen the blood vessels and reduce the severity and frequency of the vascular spasms in Raynaud's syndrome.
If the lungs are affected in scleroderma, the cytostatic agent cyclophosphamide is often used. If the kidneys are involved, ACE inhibitors are used.
Light therapy (PUVA) as well as lymph drainage, physiotherapy and physiotherapy help to counteract stiffness of the fingers in scleroderma.
What can you do yourself?
- Take care of your skin regularly to avoid scarring. Ask your doctor which care products are suitable.
- Avoid nicotine and alcohol.
- Get enough exercise. Regular exercise keeps you fit and contributes to your well-being.
- Eat a healthy diet: Diet also helps relieve the symptoms of scleroderma. Eat little red meat, but a lot of fruit and vegetables and unsaturated omega-3 fatty acids (such as in fish). This is how you will help your body minimize inflammation.
Treatment of circumscribed scleroderma
Ointments containing cortisone have anti-inflammatory effects and are particularly helpful in the active phase of scleroderma. They are prescribed by the doctor and usually applied once a day. For severe forms, the doctor prescribes cortisone tablets.
Light treatment (phototherapy) with UVA light is the most effective treatment for circumscribed scleroderma. It should help against the inflammation, hardening and thickening of the skin. Together with an active ingredient from the psoralens group, which makes the skin more sensitive to light, this treatment is called PUVA. The PUVA can be used as a cream (cream PUVA), bath (bath PUVA) or tablet (systemic PUVA). The hardened areas of the skin usually become significantly softer.
Physiotherapy is also an important part of treatment. It prevents stiff joints and maintains muscle strength. Lymphatic drainage or connective tissue massages can also be helpful.
Causes and Risk Factors
causes
Scleroderma is an autoimmune disease of unknown origin. In the case of an autoimmune disease, the immune system works incorrectly: It incorrectly identifies its own tissue as foreign and attacks it. The defensive substances (antibodies) formed in the process get into the entire body with the blood and cause inflammation in various organs. Too many connective tissue cells are produced in response to scleroderma. These are deposited in the skin and in the organs and cause the tissue to harden. In addition, the inner layer of the blood vessels is damaged.
It is not known why the immune system is not working properly. Medical professionals assume that several factors play a role.
Possible triggers for the autoimmune disease are:
- Genetic disposition
- Hormones (women get sick more often than men)
- Environmental factors such as infections with viruses and bacteria (Borrelia) or smoking
- Medicines like bleomycin, pentazocine
- Chemicals such as organic solvents, gasoline, formaldehyde
Risk factors
The most important risk factor for the development of scleroderma is a corresponding genetic predisposition: There are usually several cases of scleroderma in affected families. However, a genetic predisposition to scleroderma does not mean that those affected actually get it. It is therefore not recommended that someone's close relatives get tested for antibodies before symptoms appear.
Examinations and diagnosis
The first noticeable are the changes in the skin, which in systemic scleroderma are often associated with Raynaud's syndrome. The first point of contact for suspected scleroderma is the internist or dermatologist. He first inquires about the symptoms, followed by a detailed physical examination.
There are no tests that the doctor can use to clearly diagnose scleroderma. It is therefore a so-called exclusion diagnosis. This means that the doctor will do a lot of tests to rule out other diseases.
Examination of the skin
The doctor pays attention to typical skin changes that indicate scleroderma. Depending on where they occur, he can further narrow the diagnosis down. Raynaud's syndrome, for example, does not occur in circumscribed scleroderma. If it is present, it speaks more for systemic scleroderma.
Examination of the small gnawing vessels
Dilated blood vessels in the nail fold - the small gap between the nail wall and the nail bed - are another indication of scleroderma. The doctor uses a microscope or a small camera (dermatoscope) to check the condition of the small blood vessels on the fingernails.
Blood test
If systemic sclerosis is suspected, the doctor will examine the blood. Almost all scleroderma patients have certain antibodies, so-called antinuclear antibodies (ANA), in the blood. The blood test also gives the first clues as to whether the organs are affected.
roentgen
With the help of an X-ray examination, the doctor can, for example, determine bone changes on the fingertips or calcifications in the tissue. The lungs and heart can also be assessed using a chest X-ray.
Computed tomography (CT)
If the doctor suspects that internal organs such as the lungs, kidneys or heart are affected, he orders a computed tomographic examination.
Magnetic resonance imaging (MRI)
Some changes can be seen better with magnetic resonance imaging (MRI). For example, if the doctor recognizes an “en coup de saber”, he uses an MRI of the head to examine whether the brain is also affected by scleroderma.
Further investigations
In order to determine whether and to what extent internal organs have been damaged by scleroderma, further examinations may be necessary, for example ultrasound, electrocardiogram (EKG), heart echocardiography, lung function test or an esophagus, stomach and colonoscopy.
prevention
Since the exact trigger for scleroderma is not known, there are no concrete measures to prevent the disease. It is all the more important to see a doctor at an early stage at the first signs of scleroderma. In this way, the course of the autoimmune disease can be positively influenced.
Tags: menopause toadstool poison plants fitness




.jpg)