syphilis
and Martina Feichter, medical editor and biologistSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Syphilis is an infectious disease. It is triggered by a bacterium and is mainly transmitted during unprotected sexual intercourse. Typical first symptoms are ulcers on the genital organs and lymph node swelling. In the further course the bacteria can cause severe organ damage and even lead to death. Read everything you need to know about symptoms, ways of infection, treatment and chances of a cure for syphilis!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A50A51A52
Brief overview
- What is syphilis Syphilis, also known as syphilis, is an infectious disease caused by the Treponema pallidum bacterium.
- How can you get infected with syphilis? Syphilis is very contagious. The pathogens are mostly spread through unprotected sex, less often through direct contact with infected blood (e.g. via contaminated drug equipment). In addition, infected pregnant women can transmit the pathogen to the unborn child (congenital syphilis).
- How common is syphilis? The number of cases has been rising steadily since 2009, to just under 8,000 reported cases in 2019. Syphilis is much more common in large cities / towns than in rural areas. Men are affected significantly more often than women.
- What are the symptoms of syphilis? The symptoms of syphilis are very variable and depend on the stage of the disease. Initially, painless ulcers develop at the point of entry of the pathogen and swollen lymph nodes. In the second stage, the syphilis spreads, those affected complain of skin rashes and unspecific symptoms (e.g. fever, headache and joint pain). In the third stage, syphilis affects internal organs. Inflammation in the brain and spinal cord mark the fourth stage - possible consequences are blindness, deafness, and dementia.
- What antibiotics do you get for syphilis? Doctors usually treat syphilis with the antibiotic penicillin G. If they are allergic to penicillin, they use other antibiotics, such as doxycycline or ceftriaxone.
- Does syphilis heal on its own? Syphilis can be cured with antibiotics. Without therapy, the disease sometimes heals on its own. If left untreated, however, it can also be chronic and cause severe organ damage.
- Am I immune after a syphilis infection? No. Even after an infection has healed, you can get infected again with syphilis bacteria!
Syphilis: symptoms
An infection with syphilis (syphilis, hard chancre) is "asymptomatic" in about half of all patients. That means: the infected do not develop any symptoms. The other half of those infected have syphilis symptoms. These can be very different and differ from patient to patient.
-
"You can get infected repeatedly with syphilis"
Three questions for
Dr. med. Dagmar Ludolph-Hauser,
Specialist in skin and venereal diseases -
1
How is syphilis mostly recognized today?
Dr. med. Dagmar Ludolph-Hauser
Syphilis is a diagnostic chameleon. The symptoms can manifest themselves in skin or organ changes. In addition, syphilis is rare, so you don't necessarily think about it first. Changes in the skin or open areas, genitally or in the mouth, usually lead you on the right track. If there is any suspicion, a blood test is then carried out. Incidentally, pregnant women are routinely tested because they can transmit syphilis to the unborn child.
-
2
How dangerous is syphilis?
Dr. med. Dagmar Ludolph-Hauser
Syphilis is a very serious disease if left untreated if it does not heal spontaneously. It can cause severe permanent damage in all organ systems - for example the eyes, heart and central nervous system. However, especially in the early stages of the disease, the infection can be treated well with penicillin.
-
3
Can you get rid of syphilis completely?
Dr. med. Dagmar Ludolph-Hauser
Complete healing is possible in the majority of cases. Provided that the illness is treated in a timely manner and does not occur with other serious illnesses, for example HIV. But even those who have been successfully treated should have a blood test once a year for life, as syphilis does not lead to immunity and new infections are possible.
-
Dr. med. Dagmar Ludolph-Hauser,
Specialist in skin and venereal diseasesDr. med. Dagmar Ludolph-Hauser devotes herself holistically to healing and aesthetic medicine in her practice in Landshut and believes that venereal diseases should not be a taboo subject.
Symptoms of syphilis in both men and women
Basically, syphilis symptoms can affect women and men equally. The only thing that varies is where the first sign of infection develops: a painless, fluid-secreting nodule. The small ulcer arises at the entry point of the syphilis pathogen. In men this is mostly on the penis (preferably on the glans) and in women very often on the labia.
Another potential gender difference concerns hair loss, which can occur in later stages of the disease. There is evidence that it is more common in men than women.
That being said, syphilis generally has four stages in both sexes. The first two stages are also called early syphilis, the last two late syphilis. The time interval between the individual stages and their characteristics can vary greatly from patient to patient. It can also happen that individual syphilis stages are barely noticeable or even completely absent.
1st stage syphilis symptoms
The first sign of syphilis appears an average of three weeks after infection: a small, coarse ulcer forms at the point of entry of the pathogen. It is called "ulcus durum" or "primary effect". As mentioned above, the small nodule is mostly found on the penis in men and on the labia or in the vagina in women. It causes little or no pain in these areas.
In people who contract syphilis through oral sex, the ulcer often develops on the lips, in the oral cavity, or in the throat. If infected through anal intercourse, it forms on the anus or in the rectum. These syphilis nodules outside of the genital region can be painful.
At first the nodule is a small, reddish spot. A sharp, flat ulcer develops from this within one to two weeks. It is covered in yellow and has a rough edge wall. It often secretes a colorless liquid that contains a large number of syphilis pathogens. So it is highly infectious.
Over the next few weeks, the lymph nodes around the ulcer swell. They don't hurt and feel hard.
The ulcer at the point of entry of the syphilis pathogen heals spontaneously (by itself) within four to six weeks. The lymph node swelling can persist for months. Without treatment, the first stage of syphilis (primary stage) can move on to the next stage.
Stage 2 syphilis symptoms
The second stage of syphilis (secondary stage) can occur around four to ten weeks after infection. This happens when the pathogen spreads through the blood and lymph vessels in the body.
Initial syphilis symptoms at this stage are flu-like symptoms such as fever, tiredness, headache, muscle and joint pain. More hard lymph node swellings develop.
As the disease progresses, a skin rash (exanthema) forms, which can be very variable: Typically, slightly reddish, non-itchy spots appear first, mainly on the trunk. After a few days, the spots can develop into rough nodules (papules). Like ulcers, they may open up and begin to ooze. Again, the leaking liquid is highly contagious.
At the base of the neck, after the skin symptoms have healed, the color pigments of the skin may disappear (depigmentation). What remains is the pale "necklace of Venus".
Possible syphilis symptoms in this second stage of the disease are also changes in the mucous membrane in the oral cavity: a wide variety of plaques can form here (red, furrowed, whitish, etc.). In addition, the tonsils can swell.
Flat, lobed tissue growths sometimes form in the anus region.
In many patients, hair begins to fall out in places. Doctors refer to this as alopecia syphilitica.
Although syphilis in the 2nd stage is primarily noticeable in the area of the skin and mucous membranes, all organ systems are affected by the disease! This can manifest itself, for example, in anemia, liver swelling and headaches.
The symptoms of syphilis in the second stage (secondary stage) may subside after a few weeks without leaving any traces (such as scars). But they can recur several times (relapse = recurrence, relapse). The symptoms are less pronounced from time to time, and the skin symptoms are increasingly limited to a smaller area.
Resting phase (latency)
After the second stage of syphilis, the disease can come to a prolonged standstill. This can last up to ten years (on average it is three to four years). During this time, there are no syphilis symptoms at all. However, the pathogen is still in the body: there is still a risk of infection. At some point the syphilis can break out again - now as so-called late syphilis (3rd and 4th stages).
Stage 3 syphilis symptoms
The third or tertiary stage is characterized by syphilis symptoms, which in addition to skin and mucous membranes can also affect internal organs (such as the skeleton, nervous system, eyes, etc.). So-called gums can now develop anywhere in the body. These are slow-growing lumps that can break open and form one or more ulcers. The tissue in the ulcer usually dies (necrosis).
The name "gums" comes from the fact that the tissue knots contain a thin, stringy (rubbery) and inflammatory secretion.
It becomes particularly dangerous when syphilis damages the wall of the main artery (aorta). Doctors speak of "mesaortitis luica" here. A bulging wall (aneurysm) can form. At this point the aortic wall is very thin and can easily burst. Then there is a mortal danger! The aorta carries a lot of blood. If it tears open, you can bleed to death internally in a short amount of time. This can happen decades after being infected with syphilis.
4th stage syphilis symptoms
If left untreated, syphilis can develop inflammation in the central nervous system (brain and spinal cord) about ten to twenty years after infection. Then one speaks of neurolues or neurosyphilis. The symptoms of syphilis that you experience depend on which part of your brain and / or spinal cord is affected.
If the back marrow is infected, reflexes can fail and coordination of movements can be disturbed. Incorrect sensations (such as tingling in the skin), stabbing pain in the lower abdomen and legs, and impotence are also possible. In addition, many patients can no longer control the emptying of the bladder and bowel.
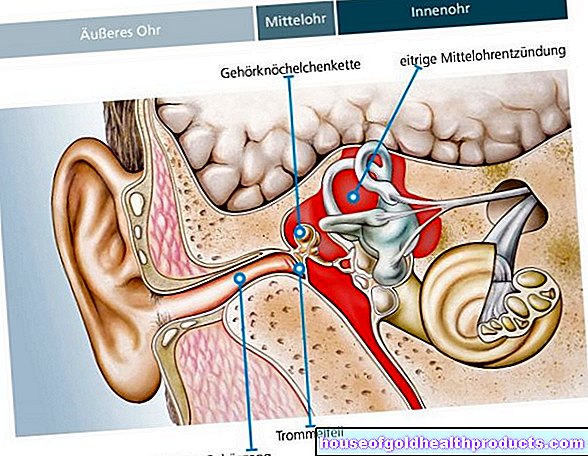
Some syphilis patients develop meningitis with damage to the cranial nerves. Doctors call this "syphilitic meningitis". Possible consequences are, for example, numbness, dizziness, paralysis of the eye muscles and visual disturbances.
If the syphilis pathogens affect the brain, the result is chronic encephalitis (encephalitis). It is known as progressive paralysis and can cause a variety of symptoms. For example, those affected show changes in their personality, develop concentration and memory disorders and gradually become demented. Paralysis is just as possible as epileptic seizures, delusions and depression. Without treatment, progressive paralysis leads to death within four to five years.
The 4 stages of syphilis and their symptoms
Congenital syphilis: symptoms
Many children who are infected with syphilis in the womb die during pregnancy (miscarriage, stillbirth) or shortly after birth. Others are born prematurely (premature birth).
Infected newborns are often normal at first. Syphilis symptoms such as breathing problems (respiratory distress syndrome in the newborn), tissue swelling (edema), enlarged liver and spleen, jaundice, anemia and skin symptoms rarely occur immediately after birth.
Many of the small patients do not show signs of syphilis until they are 3 to 10 weeks old. These include:
- Fever and swollen lymph nodes
- variable skin changes (mostly on the palms of the hands and soles of the feet) and mucosal ulcers
- broad-based, wart-shaped raised areas of the skin (condylomata lata), especially in the skin folds (anus and genital region, armpits, etc.)
- Tissue swelling (edema)
- Enlargement of the liver
- Enlargement of the spleen
- Jaundice
- paleness
- punctiform skin bleeding (petechiae)
- Inflammation of the nasal mucosa (rhinitis, "runny nose")
- Inflammation of the intestine (enteritis)
- Inflammation of the larynx (laryngitis)
- decreasing drinking from breast or bottle
Meningitis as a result of congenital syphilis (syphilis connata or syphilis connata) usually becomes noticeable between the ages of 3 and 6 months (refusal to drink, screaming or whimpering, breathing disorders, etc.). Other signs that syphilis has affected the central nervous system are, for example, seizures and "water head" (hydrocephalus).
All of these syphilis symptoms in newborns and infants are summarized under the term "Lues connata vorcox". Without treatment, the disease will sooner or later move on to the next phase of the disease after the second year of life ("Lues connata tarda"):
There are now signs of syphilis in various organs. Some examples:
- "Saddle nose" as well as changes in the palate, forehead and shins, swellings in the knee joints
- Inflammation of the cornea of the eyes (with photophobia, eye pain and vision problems up to blindness)
- Hearing loss or deafness
- Malformations of the teeth ("barrel teeth")
- small cracks in the skin and mucous membrane (fissures), e.g. torn corners of the mouth
- Seizures, failure of cranial nerves, etc. when the nervous system is affected
At this stage, syphilis patients are no longer contagious.
Syphilis: Contagion & Causes
The cause of the so-called French disease is the bacterium Treponema pallidum. It is mainly transmitted from one infected person to another during unprotected sexual intercourse. Syphilis infection is also possible through oral and anal intercourse. People with frequently changing sexual partners are particularly at risk.
The syphilis bacteria can also be spread by simply kissing them. This can happen, for example, if the patient has a small vesicle / ulcer in the oral cavity and the partner has a tiny injury in the mucous membrane.
Syphilis transmission through contaminated blood products is also possible during a blood transfusion. In Germany, however, all blood products are subjected to a syphilis test before they are administered to a patient. In this country there is no risk of infection in this way.
There is another possibility of infection with drug addicts: They can become infected with syphilis if they share syringes (like needles) with infected people and thus come into direct contact with infected blood.
There is also a congenital form of syphilis (syphilis connata or congenital syphilis): Pregnant women who are infected with syphilis can transmit the pathogen to the unborn child from the 5th month of pregnancy. This risk is particularly high in the early stages of the disease. If the woman only becomes infected during pregnancy, the pathogen almost always spreads to the unborn child.
Syphilis and HIV often go hand in hand. This is due, for example, to the fact that the skin ulcers in the early stages of syphilis are easy entry points for the AIDS pathogen. Both diseases can negatively influence each other in their course.
Syphilis: incubation period
The incubation period is the time between infection with a pathogen and the appearance of the first symptoms. In syphilis, this period can be anywhere from ten to 90 days. On average, however, the disease breaks out within two to three weeks.
Duration of contagion
Stage 1 patients are highly contagious. The risk of infection in the 2nd stage of syphilis is slightly lower. From the 3rd stage of the disease, there is no longer any risk of patients infecting other people with the syphilis pathogen.
Syphilis: treatment
Syphilis therapy can often be done on an outpatient basis. Sometimes, however, inpatient treatment in the hospital is necessary. This is especially true with neurolues (neurosyphilis) and congenital syphilis.
Syphilis is usually treated with penicillin (benzathine-benzylpenicillin). The pathogen is very sensitive to this antibiotic and has not yet become resistant (insensitive) to it. The duration and dosage of antibiotic treatment depend on the stage of the disease:
In early syphilis (first and second stage of the disease), the doctor usually injects the patient with a single dose of penicillin. Those who do not tolerate the active substance are given a different antibiotic. Often, for example, tablets with doxycycline or erythromycin are then prescribed. They must be taken every day for two weeks. Alternatively, in these early stages of syphilis, the antibiotic ceftriaxone can be given as a short infusion, once a day for ten days.
Late syphilis (except neurosyphilis) is also preferably treated with penicillin. But then three penicillin injections are necessary, each with an interval of several days. Here, too, another antibiotic can be used in the event of intolerance (doxycycline, erythromycin, ceftriaxone). The duration of treatment is then longer than for early syphilis (e.g. doxycycline tablets for 28 days).
Neurosyphilis requires even higher doses of antibiotics and hospital treatment. Most patients are given high-dose penicillin directly into a vein every day for two weeks. In the case of penicillin intolerance, ceftriaxone (as an infusion) or doxycycline (in tablet form) can be given.
In addition, individual symptoms of neurosyphilis are specifically treated. For example, the doctor can relieve epileptic seizures with anticonvulsant medication (anti-epileptic drugs).
In some patients it can be proven that the syphilis pathogen has attacked the central nervous system, but no symptoms occur. This asymptomatic neurosyphilis is treated in the same way as one that causes discomfort.
Side effect of therapy
From the second stage of syphilis, patients receive a one-time cortisone preparation before the first antibiotic treatment. From this stage of the disease, the number of syphilis pathogens in the body is so high that antibiotic therapy can trigger the so-called Jarisch-Herxheimer reaction:
Due to the antibiotic treatment, large amounts of syphilis bacteria break down in a short time. The body can react very violently to the bacterial toxins that are released in the process. Within two to eight hours of taking antibiotics, those affected develop a fever, chills, and headache. In addition, new rashes may appear and existing rashes may get worse.
This Jarisch-Herxheimer reaction only occurs with the first administration of penicillin. It can be prevented if cortisone is given half an hour or a full hour before the antibiotic.
Regular check-ups
The success of the syphilis treatment is checked in several follow-up examinations. At certain time intervals (every few months) the attending physician will examine the patient's blood for the type and amount of antibodies against the syphilis pathogen. In the case of neurosyphilis, the cerebral spinal cord fluid (liquor) must also be examined. How often and at what intervals check-ups are advisable in individual cases can be found out by their doctor.
Treat partners too
Up to the 3rd stage of the disease, syphilis patients can infect other people, especially during sexual intercourse. In patients in the 1st stage of syphilis, all sexual partners of the previous three months should therefore be advised, examined and - if necessary - treated with antibiotics by a doctor. In the case of syphilis in the 2nd stage or in the early resting phase (latency phase), the same is recommended for all sexual partners of the past two years.
Syphilis therapy in pregnant women
In all stages of the disease, syphilis should be treated with penicillin during pregnancy.
If the woman has a penicillin allergy, doctors recommend specific immunotherapy (desensitization): the patient is given gradually increasing amounts of penicillin (starting with a very small dose). So your hypersensitive immune system should slowly get used to it.
Many other antibiotics used to treat syphilis are unsuitable during pregnancy. Some can endanger the unborn child (such as doxycycline), others damage the liver and trigger gestosis ("pregnancy poisoning") (erythromycin estolate). In exceptional cases, syphilis during pregnancy can be treated with the antibiotic ceftriaxone.
Therapy of congenital syphilis
Newborn babies born with syphilis are given penicillin directly into a vein for two weeks. If the baby is also infected with HIV, the antibiotic may be given longer.
Syphilis: examinations and diagnosis
If syphilis is suspected, the doctor first takes the patient's medical history (anamnesis). Among other things, he has the symptoms described in detail, asks how long they have existed and whether there are any pre-existing or underlying diseases (such as HIV infection). The doctor also inquires about the patient's sex life. As uncomfortable as such questions are for some people affected, the doctor needs the information in order to be able to make the correct diagnosis as quickly as possible.
In the next step, the doctor tries to detect the syphilis pathogen directly or indirectly:
In the early stages, the bacteria can be found in large numbers in the liquid secretion of the skin ulcers. A special microscopy technique is used (dark field microscopy).
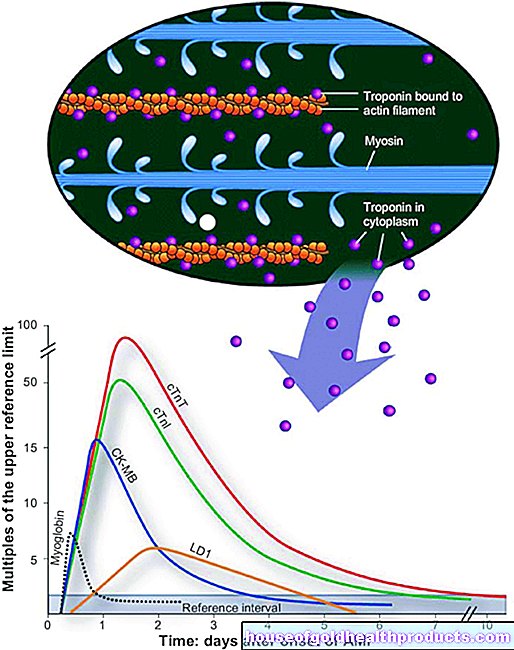
Specific antibodies in the blood can be detected after the pathogen has passed into the bloodstream. Various test methods are used for this search test, for example the Treponema pallidum hemagglutination test (TPHA). It shows a positive result two to three weeks after infection, which usually lasts for a lifetime. Then the patient is very likely to actually have syphilis.
Rapid syphilis tests are also suitable as a search test for specific antibodies against the pathogen.
However, the result of addiction tests is not one hundred percent certain. Even if it turns out positive, a confirmatory test with another method is therefore necessary (such as a fluorescence treponema antibody absorption test, FTA-ABS test).
Once the diagnosis of "syphilis" has been made, the doctor still has to find out whether it is an old infection or an active infection that requires treatment. The VDRL test (Veneral Disease Research Laboratory Test) is suitable for this. It detects antibodies that the immune system produces in syphilis, but also in other diseases (such as malaria, HIV). A positive test result is therefore generally an indication of tissue destruction and inflammatory processes. In the case of confirmed syphilis, the test can say something about the disease activity.
A syphilis infection can become active again after a long period of rest without symptoms (latency phase) and cause symptoms (reactivation). On the other hand, after the infection has healed successfully, you can get infected again with syphilis (reinfection). It is not possible to read from the results of the antibody determination whether it is a matter of reactivation or reinfection.
If neurosyphilis is suspected, the doctor will also take a sample of the cerebrospinal fluid (CSF puncture). It is examined in the laboratory for specific antibodies against syphilis bacteria.
Often the doctor will carry out further examinations. Among other things, they serve to rule out comorbidities. For example, some syphilis patients still suffer from other sexually transmitted diseases such as HIV, hepatitis B or chlamydia.
Syphilis is notifiable
Doctors must report any evidence of the syphilis pathogen to the responsible health department. This applies to both direct detection (smear of skin ulcers) and indirect detection (specific antibodies against syphilis bacteria). The name of the patient is not given to the health department.
Syphilis: disease course and prognosis
Antibiotics are very effective in treating syphilis: the first two stages of the disease are almost 100 percent curable thanks to these drugs. Even in the third stage, penicillin therapy can cure the infection in most cases. In general, however, existing organ damage cannot be reversed.
Without treatment, syphilis heals spontaneously in about every third patient (early stages). In others, the disease progresses and becomes chronic. In advanced stages, organs are permanently damaged. Approximately every 10th patient dies from untreated syphilis.
In HIV patients, syphilis is often untypical and more severe than in HIV-negative patients. They are also more likely to develop neurosyphilis.
Syphilis: prevention
You can prevent syphilis above all with safe sex: Always use condoms during sexual intercourse. In the case of oral sex, licking towels are recommended to protect against syphilis and other sexually transmitted diseases.
Such protective measures are especially important if someone changes sexual partners frequently. You can significantly reduce the risk of syphilis, but not completely eliminate it. The syphilis pathogen can also be transmitted when kissing or simply touching, if the infected person has ulcers in the mouth and the partner has tiny skin or mucous membrane injuries.
Caution should also be exercised with items and materials that have come into contact with the blood or infectious rash of syphilis patients in the early stages. These would be, for example, syringes, towels and bandages. They should not be used any further. With normal social contacts, however, no special precautionary measures (disinfection, etc.) are necessary - syphilis patients do not have to be avoided!
As part of prenatal care, the mother-to-be's blood is tested for syphilis, among other things. If the test is positive, the pregnant woman should be treated immediately with penicillin. The antibiotic also reaches the child via the placenta. So it is also treated. This can prevent or at least contain a child's infection.
Blood from blood donors is also subjected to a syphilis test to avoid transmission through blood transfusions.
Additional information
Guidelines:
- Guideline "Diagnosis and Therapy of Syphilis" of the German STI Society e. V.
Tags: Baby Child sleep dental care