Ulcer molle
All content is checked by medical journalists.Ulcus molle (ulcus, Latin = ulcer; molle = soft) is one of the sexually transmitted diseases. The sexually transmitted disease is relatively rare in Europe, but it can be brought in by tourists. Synonyms for ulcus molle are the terms soft chancre or chancroid. Read how you can recognize the disease and how you can protect yourself from it.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A57
Ulcus molle: description
Ulcus molle belongs to a group of diseases that are mainly transmitted through unprotected sexual intercourse. Doctors also speak of sexually transmitted diseases, STD (sexually transmitted disease) for short - they are popularly referred to as sexually transmitted diseases. STDs include, for example, syphilis (hard chancre), gonorrhea, better known as "gonorrhea", genital herpes and HIV.
The soft chancre resembles the hard chancre in appearance, but the course of the disease and the causative pathogens are completely different. It is therefore important that the two diseases are differentiated from one another.
Ulcus molle occurs predominantly in the countries of South America, Southeast Asia and Africa. Occasionally, however, infections with the bacterial pathogen can also be observed in western industrialized countries. Men are about ten times more likely to be affected by the disease than women. However, not all women notice the infection, while men usually experience typical symptoms. The most obvious signs of disease are genital ulcers. The ulcus molle does not heal on its own, but it can be treated well with antibiotics.
Ulcus molle: symptoms
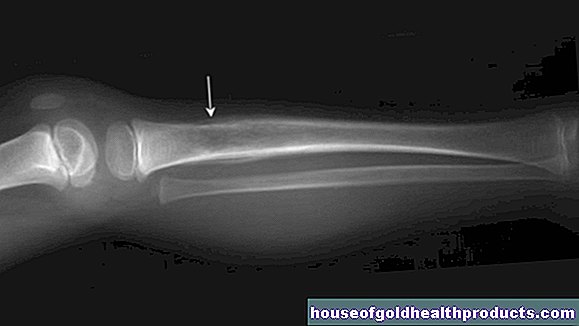
The ulcus molle causes quite characteristic symptoms. The first signs of the disease appear around two to ten days after sexual contact with an infected partner. Initially, small, reddish papules form, which then transform into vesicles. Such a vesicle eventually becomes an ulcer. This is surrounded by a red, slightly raised hem. In the center of the ulcer is a small grayish-yellow colored pit. At first, the ulcers are only a few millimeters in diameter. If there is no treatment, however, they can enlarge to a diameter of up to two centimeters as the disease progresses.
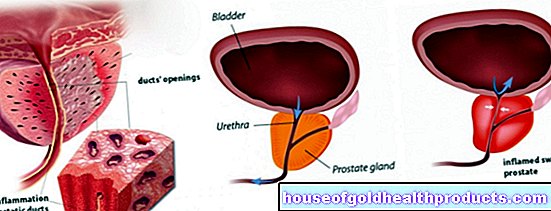
The ulcer feels soft to the touch (hence the Latin term molle = soft) and causes pain. In men, ulcer molle ulcers typically occur on the inside of the foreskin, on the edge of the glans and on the foreskin ligament. The skin changes on the glans, penis shaft or pubic mound are somewhat less common.
In women, the ulcers appear mainly on the labia majora and minor, as well as in the vicinity of the urethral orifice. The typical changes also occur in the internal sexual organs such as the vaginal mucous membrane and the cervix. Since they usually do not cause pain in these areas, affected women usually do not notice the infection. The ulcerated skin changes can also serve as entry points for other pathogens. The soft chancre can therefore pave the way for infections with HIV, genital herpes or syphilis.
Depending on the sexual practice, the ulcers of the soft chancre can in rare cases also appear on the oral mucosa or in the anal area.
If the ulcus molle is not treated, the infection will progress. The bacteria can then spread along the nearby lymphatic ducts and cause inflammation there (ulcus molle lymphangitis). In men, this can be noticeable in the form of small abscesses the size of a cherry stone in the area of the penis base. The pathogens reach the inguinal lymph nodes about one to two weeks after the first signs of the disease. These are then painfully swollen and abscesses can also form here, which the doctor calls Ulcus-molle-Bubo. In extreme cases, such an abscess breaks open and the pus empties outwards.
Ulcus molle: causes and risk factors
The cause of ulcus molle is the bacterium Haemophilus ducreyi. The infection almost always occurs through unprotected sexual intercourse, that is, when no condoms are used during sex. As a result of direct skin contact, the bacteria can then penetrate the skin or mucous membrane of the genitals through the smallest of injuries that are usually invisible to the naked eye. In contrast to circumcised men, the sexually transmitted disease occurs more frequently in men with a preserved foreskin. Therefore, the presence of the foreskin is considered a risk factor for infection with the ulcus molle. Inadequate hygienic conditions and inadequate medical care in the areas where the soft chancre is distributed play a major role in the spread of the disease. In addition, prostitution and sex tourism encourage the pathogen to spread to other regions of the world.
Ulcus molle: examinations and diagnosis
The externally visible changes to the skin and mucous membrane in ulcus molle are similar to other sexually transmitted diseases such as syphilis or genital herpes. It is important to distinguish these from each other when diagnosing ulcus molle. The doctor - usually a specialist in skin and sexually transmitted diseases - first inquires in a detailed discussion about how long the symptoms have existed and how they are expressed. Information about sexual habits is also helpful for the doctor - for example, if the person concerned has had unprotected sexual intercourse with partners whose state of health is uncertain.
This is followed by the physical examination. The doctor looks at the external genitals and palpates the lymph nodes in the groin region. In uncircumcised men, he pays special attention to the area under the foreskin. In women, a gynecologist often makes the diagnosis of ulcus molle. In addition to the outer genital region, he also examines the inside of the vagina and the cervix. If the typical ulcerated skin changes show up here, he takes a sample from the affected areas (smear) with a cotton swab. The sample is then examined for bacteria in the laboratory. If the laboratory can detect the pathogen Haemophilus ducreyi, the diagnosis of ulcus molle has been made.
The ulcus molle can also be the gateway for other sexually transmitted diseases. In most cases, the doctor will therefore arrange for further tests to rule out additional infections, for example with syphilis, herpes simplex viruses or HIV.
Ulcus molle: therapy
Therapy for ulcus molle is relatively simple and usually quite straightforward. The pathogen, Haemophilus ducreyi, can usually be fought well with an antibiotic. The drug of choice is the antibiotic ceftriaxone, which the doctor injects once into the muscles. Alternatively, antibiotics such as azithromycin, ciprofloxacin or erythromycin are available in tablet form. However, the pathogen is more often resistant to older antibiotics. If a lymph node abscess has formed in the course of the infection, the doctor may have to surgically open it to drain the pus. In order to prevent a new infection, the partner concerned must be treated in any case. It is also advisable to refrain from sexual contact until the ulcus molle has completely healed.
Ulcus molle: prevention
It is relatively easy to protect yourself from venereal diseases such as ulcus molle. Always use condoms when you have sex with people whose health you are not sure about. Use the condoms consistently, i.e. before the beginning of the first sexual contact, until it is over and for any sexual practice. If you have been found to be infected, be sure to inform your partner or anyone with whom you have had sex in the past few weeks.
Ulcus molle: disease course and prognosis
The ulcus molle usually has a good prognosis, as treatment is usually relatively easy. Without therapy, however, the disease can progress and complications such as lymph node abscesses are possible. In addition, untreated people run the risk of infecting other sexual partners. An existing infection with Haemophilus ducreyi also increases the risk of contracting other sexually transmitted diseases such as HIV.
Tags: sports fitness menopause fitness