Hemostasis
and Eva Rudolf-Müller, doctorValeria Dahm is a freelance writer in the medical department. She studied medicine at the Technical University of Munich. It is particularly important to her to give the curious reader an insight into the exciting subject area of medicine and at the same time to maintain the content.
More about the expertsEva Rudolf-Müller is a freelance writer in the medical team. She studied human medicine and newspaper sciences and has repeatedly worked in both areas - as a doctor in the clinic, as a reviewer, and as a medical journalist for various specialist journals. She is currently working in online journalism, where a wide range of medicine is offered to everyone.
More about the experts All content is checked by medical journalists.Hemostasis (hemostasis) is an important process that the body uses to stop bleeding in several intermediate steps. The wounds are closed with the help of a clot (thrombus) and then heal as the process progresses. Here you can find out everything you need to know about the process and disorders of hemostasis!
What is Hemostasis?
Hemostasis is the process by which the body stops bleeding. The word “hemostasis” comes from ancient Greek and is made up of the words “haima” (blood) and “stasis” (breastfeeding).
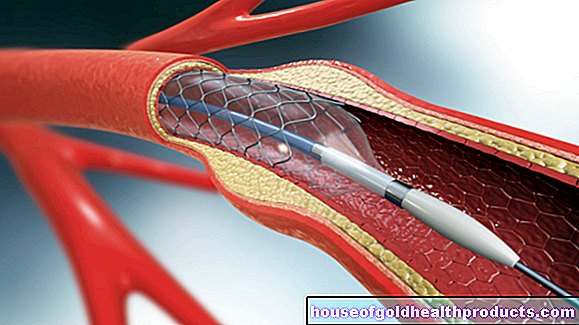
Hemostasis can be roughly divided into two steps: Primary hemostasis is used to temporarily treat a wound (vascular leak) via a rather unstable clot (white thrombus). In contrast, secondary hemostasis (blood clotting) leads to stable wound closure through a red thrombus. Despite the subdivision, primary and secondary hemostasis both take place almost simultaneously and interact with one another via many mechanisms.
Primary hemostasis
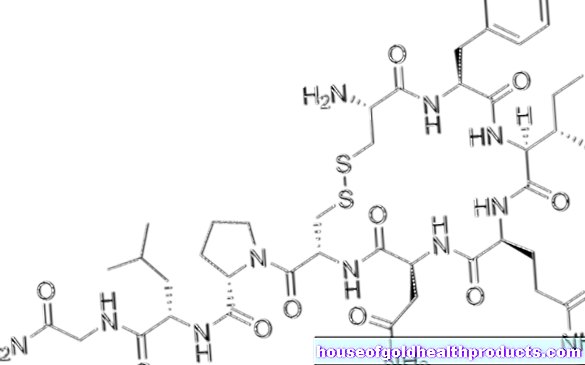
Primary hemostasis is also called cellular hemostasis, as the blood platelets (thrombocytes) are the most important component here. When bleeding, blood leaks from injured blood vessels. Damage to the inner vessel wall (endothelium) exposes various proteins that lie under the endothelium. Above all, the collagen underneath leads to binding of the so-called Von Willebrand factor to the proteins. The Von Willebrand factor attracts platelets, which also attach themselves and thus cover the damage to the endothelium.
The accumulated platelets release various substances that attract further platelets and the so-called fibrinogen (precursor of the blood fiber fibrin). In addition, they change their shape and form spiky runners that are linked with the help of fibrinogen. The enzyme cyclooxygenase (COX) also stimulates the connection between platelets. In the end, a dense structure is formed - the white thrombus that closes the wound.
Secondary hemostasis (blood clotting)
You can find out how blood clotting with the help of a red thrombus works in the article Blood clotting.
When do you determine the hemostasis values?
If a patient's wounds bleed for an unusually long time, laboratory tests should be performed to rule out a disruption of primary or secondary hemostasis. Hemostasis is also checked before operations to protect the patient.
With regard to secondary hemostasis, the so-called Quick value and the activated partial thromboplastin time help diagnose disorders.If the fault lies in the primary hemostasis, either an insufficient number of thrombocytes (thrombocytopenia) or defective thrombocytes (thrombocytopathy) can be detected.
Hemostasis values
The doctor usually takes a small sample of blood from the vein. The patient does not necessarily have to be sober for this, as food intake does not significantly change the hemostasis values. The number of platelets in healthy adults is between 150,000 and 400,000 per microliter.
The so-called bleeding time is also important. Here, depending on the method, the doctor inflicts a more or less standardized small skin injury on the patient and then checks the time until the bleeding stops. The standard values differ depending on the measurement method. A prolonged bleeding time suggests thrombocytopathy or thrombocytpenia.
After the evaluation, your doctor will explain the results to you and explain all further examination or treatment steps.
When are the hemostasis values too low?
Low platelet counts can be caused by many things. This includes:
- heavy bleeding
- Infections, such as malaria
- various forms of blood cancer (leukemia)
- Destruction of platelets by the body itself (autoimmunological destruction, e.g. thrombotic-thrombocytopenic purpura)
- certain rheumatic diseases
- blood thinning therapy
- Allergies, poisons, drugs and vitamin deficiencies
- Tumors
- pregnancy
- Cirrhosis of the liver
- increased breakdown in the spleen (trigger can be liver cirrhosis and infections)
Sometimes a low platelet count is also due to an incorrect measurement.
A bleeding time that is too short is not medically relevant.
When are the hemostasis values too high?
The increase in bleeding time may indicate a platelet deficiency. However, it is mainly used to detect thrombocytopathies. The possible causes of such dysfunction of the blood platelets include the use of certain medications such as aspirin (acetylsalicylic acid) or chemotherapy drugs. Hereditary diseases such as Willebrand-Jürgens syndrome and Bernard-Soulier syndrome can also be the reason for thrombocytopathy.
If the blood contains too many platelets (thrombocytosis), the risk of blood clots increases. The cause of thrombocytosis can be bone marrow disease or malignant tumors.
What to do if the hemostasis values change?
Smaller deviations are usually not a cause for concern. However, if an altered platelet count or a prolonged bleeding time suggests an illness, further tests and examinations should be carried out. In this case, your doctor will discuss how to proceed with you. Since hemostasis is a vital function of the body, it is important to always clarify and treat disorders.
Tags: vaccinations news alcohol