Ascites
and Martina Feichter, medical editor and biologistHanna Rutkowski is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
With ascites, fluid collects in the abdomen. That is why one speaks of ascites or water belly. Usually the ascites indicates a serious illness. A bulging abdomen is a typical symptom of advanced liver cirrhosis. But heart failure can also be accompanied by ascites. You can find out more about possible causes of ascites and how you can even recognize ascites here!

Brief overview
- What is ascites? Build-up of fluid in the abdominal cavity. Colloquially also called ascites or water belly. There are different forms of ascites such as portal ascites, inflammatory ascites, and hemorrhagic ascites.
- Causes: e.g. cirrhosis of the liver, heart failure (heart failure), abdominal inflammation such as peritonitis or pancreatitis, infections such as tuberculosis or chlamydia, cancer (such as infestation of the peritoneum in cancer of the gastrointestinal tract or the ovaries, liver carcinoma or metastases), injuries from Abdominal organs, vascular ruptures, burst operation scars, protein deficiency (e.g. due to malnutrition, kidney disease or cancer).
- When to the doctor With every suspicion of ascites! If left untreated, it can develop into life-threatening peritonitis, among other things.
- Diagnostics: taking the medical history (anamnesis) to record existing underlying diseases, physical examinations with palpation / tapping of the abdomen, ultrasound examination, blood test, possibly removal (puncture) of a sample of the fluid that has accumulated in the abdomen to determine the ascites shape.
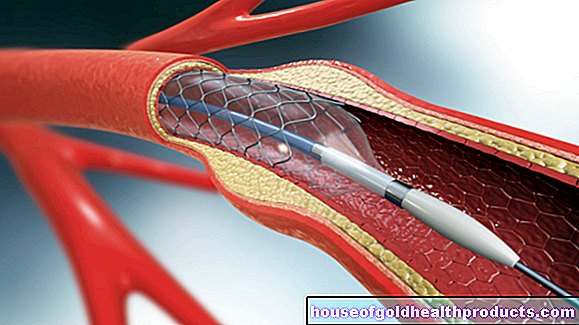
- Therapy: Treatment of the underlying disease. In the case of severe ascites, the fluid can also be removed from the abdominal cavity by means of paracentesis. Insertion of an indwelling catheter for repeated ascites.
What is an ascites?

Ascites means nothing more than dropsy. In fact, ascites is a pathological accumulation of fluid in the free abdominal cavity. The typical signs are a greatly enlarged waist size, accompanied by a feeling of pressure, pain and gas. If the accumulation of fluid is very large, it can even lead to breathing problems and circulatory disorders. An umbilical hernia (umbilical hernia) is also not uncommon in ascites.
About 80 percent of all ascites cases are due to severe liver damage such as liver cirrhosis. In other cases, tumors, inflammation or disorders of the lymphatic drainage are the triggers of ascites.
Ascites: causes
Various mechanisms can lead to ascites: The human body consists predominantly of fluid that is distributed over the cells, the environment between the cells (interstitium) and the blood vessels. A small part of this fluid gets from the blood into the tissue and is there absorbed by the lymphatic system. The fluid (lymph) is transported back into the veins via these “lines”.
If this balance is disturbed, more water gets into the surrounding tissue. The mechanisms that can lead to such a disorder and thus to ascites are:
- Increased pressure within the blood vessels, so that more fluid is pressed out (for example in the case of portal hypertension or right heart failure: see below)
- Protein deficiency (for example as a result of hunger - a visible sign is the "water belly")
- increased permeability of the cell walls (e.g. in the case of inflammation)
- Disorders of the lymphatic drainage (when obstructed by tumors or scarring)
The kidney's control circuit also plays a role: the fluid level is constantly measured at various points (baroreceptors) in the body. If more fluid escapes from the vessels, the impression arises that there is a lack of fluid, as the filling level of the vessels decreases and the blood pressure drops as a result. The kidneys then pass less urine and release hormones that raise blood pressure again. This vicious circle leads to even more liquid escaping from the vessels.
Below is an overview of the most common forms and causes of ascites:
Portal ascites
It is by far the most common form of ascites and is caused by portal hypertension (also called portal hypertension or portal hypertension):
The portal vein brings the blood from the abdominal organs (such as the stomach, small intestine) to the liver, which functions as the central metabolic organ. However, if the pressure in the portal vein is abnormally increased, this hinders the flow of blood. The blood accumulates in front of the liver, which can lead to increased leakage of fluid into the abdomen and thus to ascites. Possible causes of portal hypertension are:
- Liver cirrhosis: most common cause of portal hypertension and overall ascites. In cirrhosis, healthy liver tissue is gradually replaced by functionless connective tissue - the liver shrinks and becomes hard. Since it can no longer fulfill its function, the blood accumulates in the portal vein, which triggers portal high pressure. The most common causes of liver cirrhosis are alcohol abuse and virus-induced liver inflammation (viral hepatitis).
- Fatty liver
- Formation of a blood clot in the portal vein (portal vein thrombosis)
- Inflammation of the liver (hepatitis)
- Heart failure
Cardiac ascites
Ascites can also be a direct result of heart disease. Then one speaks of a cardiac ascites. It is often based on a right heart failure (right heart failure). The right half of the heart cannot adequately pump the oxygen-poor blood coming from the liver and other parts of the body towards the lungs. The blood backs up in the body, including the liver, which results in a congested liver. This can lead to jaundice (jaundice), bleeding disorders and ascites.
An "armored heart" (pericarditis constrictiva) can also cause cardiac ascites. In this heart disease, the pericardium is so thickened and hardened that the heart muscle in it can no longer expand sufficiently when it is filled with blood. This causes the blood to build up in front of the heart. As a result, accumulations of fluid develop on the ankles and lower legs (edema) and in the abdomen (ascites). An armored heart is created by repeated inflammations of the pericardium (chronic pericarditis).
Malignant ascites
This is understood to be cancer-related ascites: In healthy people, the peritoneum produces a small amount of fluid that acts as a lubricant between the organs. Lymph vessels in the abdomen then take up most of this fluid and direct it back into the blood vessel system. Malignant tumors can unbalance this cycle if they narrow lymph vessels in the abdomen. These can then absorb and remove less fluid from the abdominal cavity - an ascites develops.
In addition, many tumors stimulate the formation of new blood vessels in their environment by releasing messenger substances. You want to improve your own supply of oxygen and nutrients. However, the messenger substances make the vessel walls more permeable, so that more fluid escapes. This also contributes to the fact that many cancer patients develop malignant ascites (especially in the advanced stages).
Most often, people with cancer of the peritoneum (peritoneal carcinosis) develop malignant ascites. The cancer cells that settle on the peritoneum mostly come from tumor foci on neighboring abdominal organs, mainly stomach cancer, colon cancer, ovarian cancer or pancreatic cancer.
In addition to peritoneal carcinoma, liver carcinoma (liver cancer) can also cause malignant ascites. The same applies to liver metastases (daughter settlements of, for example, colon cancer, lung cancer, breast cancer, gastric or esophageal cancer).
Inflammatory ascites
In this form of ascites, the fluid that has accumulated in the abdomen is cloudy and bacteria or other pathogens can be detected in it. Possible causes of an inflammatory ascites are for example:
- Peritonitis: The life-threatening peritonitis is often caused by previous illnesses (such as appendicitis), injuries or surgical scars in the abdomen. In many cases it is accompanied by ascites. Conversely, peritonitis can also be the result of ascites that cannot be treated.
- Acute pancreatitis: Acute pancreatitis manifests itself in severe, belt-shaped upper abdominal pain, fever, nausea and vomiting. As a result, jaundice and ascites can develop.
- tuberculosis
- inflammatory vascular disease (vasculitis)
- genital infection with chlamydia or gonococci (gonorrhea)
Hemorrhagic ascites
This form of ascites is caused by heavy bleeding into the abdomen (hematoperitoneum), for example as a result of injuries or tears (ruptures) of organs or vessels or burst surgical scars in the abdomen. There is an additional risk of death by bleeding to death!
Chylous ascites
With chylous ascites, the fluid that has accumulated in the abdominal cavity is milky. It is namely leaked lymph fluid. The relocation of the lymphatic drainage is mainly due to:
- Tumors or metastases
- Scarring after abdominal surgery
Other causes of ascites
Severe albumin deficiency (hypoalbuminemia) is one of the rare causes of ascites. Albumin is an important protein in the blood. If there is too little of it, the pressure in the vessels drops (colloid osmotic pressure). Then water is stored in the body - water accumulates in the tissue (edema) and ascites. The causes of the albumin deficiency are diverse:
- Hunger, malnutrition, anorexia nervosa: The pictures of emaciated children with water bellies in impoverished regions are particularly well known.
- Nephrotic syndrome: It is caused by damage to the kidney corpuscles, for example as a result of diabetes, tumor diseases or vascular inflammation. The damage leads to the fact that more proteins such as albumin are excreted in the urine. This can be associated with pronounced ascites.
- Exudative gastroenteropathy: This is where the stomach and intestinal mucous membranes absorb more protein, so that the protein level in the blood drops. Typical symptoms are severe diarrhea, edema, ascites and weight loss. Examples of triggers for exudative gastroenteropathy are Crohn's disease, ulcerative colitis and celiac disease.
The cause of biliary ascites lies in the area of the gallbladder. For example, a gallbladder inflammation can lead to a perforation in the gallbladder wall. Then bile and pus drain into the abdominal cavity.
Other rare causes of ascites include an underactive thyroid (hypothyroidism) and Whipple's disease (a rare bacterial infectious disease).
Ascites: when do you need to see a doctor?
If the abdominal circumference increases, this does not necessarily mean that you have ascites. It can also be due to very simple flatulence or indigestion, which should, however, go away after a few days. Another possible explanation for an enlarged abdomen is rapid, unwanted weight gain due to underactive child's gland.
In otherwise healthy people, there is no need to immediately think of ascites when the abdominal girth increases. Ascites develops much more often in people who already have a serious pre-existing condition such as liver or heart disease. In cancer, too, ascites is rarely the first symptom; usually numerous other complaints have occurred before.
Nevertheless, the following applies: If ascites is suspected, a doctor should always be consulted! Ascites is usually a symptom of a serious illness or injury. In addition, if left untreated, it can lead to life-threatening peritonitis or acute shortness of breath (if there is a very large amount of fluid).
Ascites: what does the doctor do?
From a certain amount of fluid in the abdominal cavity, ascites can usually be recognized at first glance by the enlarged abdominal circumference. The doctor can obtain further important information from the patient's medical history (anamnesis). In many cases, previous illnesses are already known that could trigger ascites (such as heart failure or cirrhosis of the liver). In other cases, the initial consultation with the patient will help the doctor track down such a pre-existing condition or other possible cause of ascites (such as a recent accident with a bruise in the abdomen).
During the subsequent physical examination, the doctor palpates and pats the stomach. If wave-like movements become apparent under the abdominal wall when you tap it, this indicates greater edema.
The most reliable way to detect ascites is by means of ultrasound (abdominal sonography). The doctor can use it to detect even the smallest accumulations of fluid of 50 to 100 milliliters. In addition, the doctor can also use ultrasound to examine the liver, heart and digestive organs and determine any diseases that are causing the ascites.
A blood test is also one of the standard examinations for ascites: Changes in the blood count can indicate underlying functional disorders of the liver or heart, among other things.
The exact shape of the ascites can be found out with a puncture: the doctor uses a thin hollow needle to pierce the abdominal wall into the abdominal cavity and take a sample of the accumulated fluid. Their color alone provides important information about the cause of ascites. Clear secretion is more likely to be found in liver and heart diseases, while a milky color indicates impaired lymphatic drainage. In the case of inflammatory ascites, the triggering germs can be detected and determined in the liquid sample. This is important for later therapy.
Therapy of ascites
Ascites therapy has two goals: First, it is important to treat the cause of ascites. Second, the waist circumference should be reduced in order to relieve the patient's symptoms such as feeling of pressure, pain or shortness of breath.
An example of treatment for ascites:
Liver diseases are treated with diets that are free or low in salt and water that is used to remove water (diuretics). If this treatment alone does not work or the ascites is very pronounced, the doctor can also remove the fluid in the abdominal cavity by means of a small surgical procedure (paracentesis). This therapy immediately improves patient well-being, but carries the risk of infection or bleeding. Often the paracentesis has to be repeated as the ascites often recurs. Then an indwelling catheter can help.
Ascites: You can do that yourself
You should always see a doctor if you have ascites. He will - depending on the cause of the ascites - initiate appropriate therapy. In support of this, you should observe the following rules:
- Little salt: If you have ascites, avoid too much salt because the sodium it contains promotes water retention in the body. Ask your doctor what amount you should limit your daily salt intake to.
- No alcohol: Liver diseases such as cirrhosis are the most common cause of ascites. In order not to put additional strain on the diseased organ, you should definitely refrain from alcohol.
- Light whole food: In the case of liver diseases, a light whole food is generally recommended, i.e. a wholesome diet in which individually incompatible or difficult to digest foods (e.g. deep-fried or high-fat foods, legumes) are avoided.
- Bed rest stimulates the body to excrete more water. Because the blood is distributed differently when lying down than when standing, the vessels in the abdomen are then also plumper - a signal for the kidneys to excrete more fluid. This can help eliminate ascites.







.jpg)







.jpg)