Cushing's Syndrome
and Martina Feichter, medical editor and biologistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Cushing's syndrome develops when too large an amount of the hormone cortisol circulates in the body - or its artificial counterpart, the drug cortisone. The consequences are far-reaching changes in the entire body: The patients develop a “full moon face” and a “buffalo neck”. In addition, the susceptibility to infection increases, blood pressure shoots up, muscle weakness and a constant feeling of thirst develop. Find out the most important information about "Cushing's Syndrome" here.

Brief overview
- What is Cushing's Syndrome? A complex of various symptoms that result from an excess of the hormone cortisol.
- Symptoms: including trunk obesity, full moon face, bull's neck (buffalo neck), increased cholesterol, high blood pressure, reduced muscle mass, osteoporosis, wound healing disorders, parchment skin, increased susceptibility to infections, male hair type (hirsutism) and cycle disorders in women, erectile dysfunction in men, growth disorders in children, psychological changes like depression)
- Causes: either excessive intake of drugs containing cortisone (exogenous Cushing's syndrome) or overproduction of cortisol in the adrenal glands (endogenous Cushing's syndrome). The latter is usually based on a benign or malignant tumor (e.g. tumor of the pituitary or adrenal gland).
- Diagnostics: taking the medical history (anamnesis), physical examination, blood tests, imaging tests if a tumor is suspected
- Treatment: discontinuation of cortisone-containing drugs (exogenous Cushing's syndrome), tumor treatment by means of surgery, radiation therapy, chemotherapy or adrenostatic drugs (endogenous Cushing's syndrome)
Cushing syndrome: description
Doctors speak of a “syndrome” when several symptoms are present at the same time. In the case of Cushing's syndrome, there are actually many symptoms. The cause is too high a concentration of the hormone cortisol. In the right dose, cortisol is essential in the human body. But if it is in abundance (hypercortisolism), cortisol can cause problems at many different switching points in the body and thus lead to the full picture of Cushing's syndrome.
The inactive precursor to cortisol in the body is called cortisone. There are also drugs that are colloquially known as cortisone. More precisely, these are synthetically produced glucocorticoids. If they are administered in too high a dose, Cushing's syndrome can also develop (see below: Exogenous Cushing's syndrome).
Cushing's Syndrome: How Cortisol Works
Cortisol is an essential hormone that has numerous functions. It is also known as the stress hormone because it is produced more when the body is permanently exposed to increased demands.
Cortisol activates degrading (catabolic) metabolic processes, which means that more energy-rich compounds in the form of carbohydrates, fats and proteins are available to the body - the body is thus adequately supplied with energy. Cortisol intervenes on different metabolic levels:
- It indirectly (via gene expression) ensures the supply of sugar (through glucogenesis in the liver), proteins (mainly through muscle breakdown) and fat. In the middle of the body (stomach, neck, face) there is also increased fat storage.
- Furthermore, cortisol causes a breakdown of collagen, connective tissue and bone material, which in excess leads to a breakdown (atrophy) of the skin and a decrease in bone density.
- Cortisol increases blood pressure by increasing the cardiac output and constricting the blood vessels.
- Finally, cortisol also plays an important immunosuppressive role by inhibiting the immune and inflammatory reactions to a certain extent. This is also the reason why cortisol is of great importance as a drug.
Cushing syndrome: symptoms
Due to the diverse functions of cortisol in the body, the symptoms of Cushing's syndrome are very different:
- Trunk obesity: In Cushing's syndrome, increased fat is stored on the trunk of the body. That is why those affected usually have a massive stomach ("beer belly"). Legs and arms, on the other hand, are slim.
- Full moon face / moon face: A face that is round and reddened due to fat deposits is also typical of Cushing's syndrome.
- Bull neck (buffalo neck): Increased fat is also deposited in the neck area.
- High cholesterol: The amount of cholesterol in the blood is often high in Cushing's syndrome.
- High blood pressure: Many people with Cushing's syndrome have high blood pressure.
- Diabetic metabolic situation: Due to the increased concentration of sugar in the blood (hyperglycaemia) and an increased release of insulin, a metabolic situation occurs in Cushing's syndrome that is very similar to that of diabetes mellitus (diabetes). The high levels of sugar in the blood trigger an increased feeling of thirst and frequent urination.
- Muscle weakness and decreased bone density: As part of Cushing's syndrome, muscles and bone tissue break down. This reduces muscle mass and develops osteoporosis.
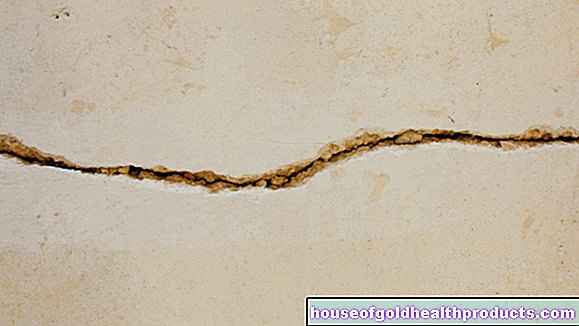
- Skin changes: The skin also suffers from Cushing's syndrome - it becomes thin (parchment skin), and sometimes red stretch marks (Striae rubrae) develop, mainly on the abdomen. Impaired wound healing and episodes of acne and boils are also possible.
- Increased susceptibility to infections: Due to the general suppression of the immune system in Cushing's syndrome, those affected are susceptible to infections - for example, one cold often chases the next.
- Psychological changes: Sometimes Cushing's syndrome is also accompanied by psychological changes such as depression.
- Masculinization: Women with Cushing's syndrome can masculinize (virilism) - increased body hair develops in areas typical for men (hirsutism) as well as menstrual disorders.
- Impotence: Men with Cushing's syndrome often develop impotence.
- Decreased growth: In children, Cushing's syndrome impairs growth through an indirect inhibition of growth hormone.
Cushing syndrome: causes
When asked about the cause, one must first differentiate between exogenous Cushing's syndrome and endogenous Cushing's syndrome. Exogenous means that it is brought about from the outside. In contrast, the endogenous Cushing's syndrome arises from a malfunction or disease in the body.
Exogenous Cushing Syndrome
An exogenous Cushing's syndrome usually results from an excessive intake of glucocorticoids (cortisone) as part of a drug therapy. One then speaks of iatrogenic Cushing's syndrome (iatrogenic = caused by a doctor or medical therapy).
The active ingredient cortisone (after it has been converted into cortisol in the body) has an anti-inflammatory and immunosuppressive effect on the immune system. It is therefore used, for example, to treat chronic inflammatory bowel diseases (Crohn's disease, ulcerative colitis), asthma, multiple sclerosis and many autoimmune diseases. In such cases, cortisone is usually administered systemically, for example as a tablet or infusion. If it is accidentally overdosed, exogenous Cushing's syndrome can develop. It is therefore important that cortisone therapy is always carried out under medical supervision.
The dose of glucocorticoids that causes Cushing's syndrome in a patient is called the Cushing's threshold.
Endogenous Cushing's Syndrome
Endogenous Cushing's syndrome is also based on an excess of glucocorticoids / cortisol. Here, however, this arises in the body itself. Endogenous Cushing's syndrome is much rarer than the exogenous variant. Women are affected significantly more often than men.
The regulation of cortisol production
Cortisol is produced in the adrenal glands, more precisely in the so-called adrenal cortex. Other hormones are also produced there: androgens (male sex hormones such as testosterone) and aldosterone (important for regulating the water and sodium balance).
The production of cortisol does not take place arbitrarily, but is subject to complex regulation by higher-level control bodies. The first control point is the pituitary gland. The hormone adrenocorticotropin (ACTH) is produced in its anterior lobe. It stimulates the activity of the adrenal cortex. Put simply, this means: the more ACTH is formed in the pituitary gland, the more hormones (mainly cortisol) the adrenal cortex produces.
The production of ACTH in the pituitary gland is in turn controlled by the diencephalon, or more precisely by the hypothalamus.This acts as a further control point for cortisol production: the hypothalamus forms CRH (corticotropin-releasing hormone), which ensures an increase in ACTH formation in the pituitary gland - and thus indirectly an increase in cortisol formation.
The self-control of cortisol formation now takes place with the help of a control circuit between CRH, ACTH and cortisol: If sufficient cortisol circulates in the blood, it throttles the release of CRH and ACTH in the hypothalamus or in the pituitary gland - and thus indirectly the further cortisol production. The following applies: the higher the cortisol level in the blood, the more CRH and ACTH are inhibited and the less new cortisol is in turn formed in the adrenal cortex.
In this way, an excess of cortisol is automatically prevented in a healthy organism. However, if this control loop is disturbed at one point, cortisol production can get out of hand and lead to endogenous Cushing's syndrome. Depending on where the disorder is located, a distinction is made between an ACTH-dependent and an ACTH-independent variant in endogenous Cushing's syndrome:
ACTH-dependent Cushing's syndrome
ACTH-dependent Cushing's syndrome is responsible for around 85 percent of all cases of endogenous Cushing's syndrome. It is based on an excess of the pituitary hormone ACTH. As a result, the adrenal cortex is stimulated to produce excessive cortisol.
The fact that too much ACTH is produced is usually due to a small tumor (microadenoma) of the pituitary gland. More rarely, an overactive hypopthalamus is to blame: The hypothalamus produces too much CRH, which stimulates the ACTH formation in the pituitary gland too strongly. But regardless of whether the increased ACTH formation ultimately originates from the pituitary gland or from the hypothalamus - in both cases one speaks of central Cushing's syndrome (also called Cushing's disease). Because the cause of the ACTH excess lies in the central nervous system (brain).
In addition to the central Cushing's syndrome, there is also the ectopic (paraneoplastic) Cushing's syndrome: It usually arises from a tumor outside the pituitary gland that produces ACTH and thus increases the unregulated cortisol formation in the adrenal glands. These ACTH-producing tumors include, for example, small cell bronchial carcinoma (form of lung cancer) and rare colon tumors. Occasionally, ectopic Cushing's syndrome is also due to a CRH-producing tumor: it stimulates the production of ACTH in the pituitary gland excessively and thus also the production of cortisol.
ACTH-independent Cushing's syndrome
About 15 percent of the cases of endogenous Cushing's syndrome arise independently of ACTH directly in the adrenal cortex: Despite a normal ACTH level, the adrenal cortex produces too much cortisol. Doctors also speak of adrenal Cushing's syndrome (adrenal = affecting the adrenal glands).
Its cause is usually a cortisol-producing tumor in the adrenal cortex. In adults it is usually a benign tumor (adenoma), in children it is more often a malignant tumor (carcinoma). Very rarely, an excessive increase in adrenal tissue (hyperplasia) is responsible for ACTH-independent (adrenal) Cushing's syndrome.
To be distinguished from these forms of Cushing is an excess of cortisol caused by alcohol consumption - the alcohol-induced "pseudo-Cushing syndrome".
Cushing Syndrome: When Should You See a Doctor?
If you notice one or more of the above symptoms, you should see a doctor. Even if it is not Cushing's syndrome and there are other causes behind it, these should be clarified. The earlier Cushing's syndrome or its causes are treated, the greater the chances that it will regress.
Cushing's Syndrome: What Does the Doctor Do?
If Cushing's syndrome is suspected, the doctor will first talk to the patient in detail in order to collect their medical history (anamnesis). Among other things, he asks about the exact complaints. He also asks what medication the patient has been taking recently - Cushing's syndrome is usually triggered by certain medications (exogenous Cushing's syndrome).
This is followed by a physical exam. Among other things, the doctor will measure the patient's blood pressure and weight and inspect his skin.
Various tests can be used to determine whether there is actually an excess of cortisol (hypercortisolism) in the blood and, if so, what its origin is:
- Cortisol measurement in saliva or blood: If the measured value is significantly increased late in the evening, it speaks for Cushing's syndrome.
- 24-hour urine collection: The urine excreted over the course of 24 hours is collected in order to determine the concentration of free cortisol in it. In the case of Cushing's syndrome, the measurement result is significantly higher.
- Dexamethasone inhibition test (short test): The patient receives the active ingredient dexmethasone at night. This signals to the body that it is no longer producing CRH or ACTH and consequently no more cortisol. If an elevated cortisol level is still measured in the patient's blood the next morning, Cushing's syndrome is likely. The increased cortisol level can also have other reasons. The dexmethasone inhibition test can also be positive in people without Cushing's syndrome, for example if they suffer from stress or depression or are taking certain medications (such as contraceptive pills, anti-epilepsy drugs).
There are other tests that can be used to clarify Cushing's syndrome. These include the insulin hypoglycemia test (to detect increased cortisol levels) as well as the dexamethasone long test and the CRH stimulation test: The last two help to differentiate between the different forms of Cushing's syndrome (central, paraneoplastic or adrenal Cushing's syndrome).
If the laboratory tests indicate a tumor as the cause of Cushing's syndrome, an attempt is made to detect it using imaging methods. Depending on the location of the tumor (such as the adrenal glands, pituitary gland), ultrasound, computed tomography (CT) or magnetic resonance tomography (magnetic resonance tomography, MRI) can be used.
Cushing syndrome: therapy
In the case of exogenous Cushing's syndrome, all drugs containing cortisone are discontinued whenever possible. But this must not happen suddenly! If you take a cortisone preparation for longer than just a few days, this inhibits the body's own cortisol production by the adrenal glands. If the drug is then stopped abruptly, there is a risk of cortisol deficiency - the body needs time to start producing cortisol again. That is why cortisone-containing drugs should always be "tapered off" at the end of therapy, i.e. slowly reducing the dose. So the body can adapt to it.
Endogenous Cushing's syndrome is treated based on its cause. For tumors, whether in the pituitary gland or the adrenal cortex, surgery is usually the first choice. If surgery is out of the question, a tumor can possibly also be treated with radiation therapy or chemotherapy. Sometimes so-called adrenostatic drugs are also prescribed - drugs that inhibit the production of cortisol in the adrenal glands.
forecast
The exogenous Cushing's syndrome can usually be brought under control if you stop taking the triggering drug or at least reduce its dose. However, this should only be done on the instructions of the attending physician.
If a tumor causes Cushing's syndrome and if it can be treated successfully, the prognosis is good. If left untreated, however, endogenous Cushing's syndrome can potentially lead to death (within months to a few years).
Tags: vaccinations Diseases nourishment