Incontinence
and Carola Felchner, science journalistDr. Andrea Bannert has been with since 2013. The doctor of biology and medicine editor initially carried out research in microbiology and is the team's expert on the tiny things: bacteria, viruses, molecules and genes. She also works as a freelancer for Bayerischer Rundfunk and various science magazines and writes fantasy novels and children's stories.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Incontinence means that you can no longer hold urine or stool - some of it comes off uncontrollably. The causes for this can be very diverse. Urinary incontinence is usually based on a disruption in the finely tuned system of bladder muscles, sphincters and pelvic floor muscles. The reason can be, for example, errors in the signal transmission of the nerve cells involved. There are good therapeutic options for incontinence today. Read here what they are and what you can do yourself with incontinence.

Brief overview
- What is incontinence? Inability to hold back urine (urinary incontinence) or, less often, stool (fecal incontinence) in a controlled manner
- Causes: different depending on the shape, e.g. B. urinary stones, enlarged prostate, tumors, nerve injuries or irritations, neurological diseases (multiple sclerosis, stroke, Alzheimer's, etc.)
- Examinations: depending on the type and severity of the incontinence, for example gynecological examination, proctological examination (examination of the rectum), ultrasound, urine and blood tests, urodynamic examinations (to determine the bladder function), cystoscopy, colonoscopy, etc.
- Therapy: depending on the form and severity of the incontinence, for example pelvic floor training, toilet training, electrotherapy, pacemaker, medication, surgery
Incontinence: Description
People with incontinence can no longer hold their urine or, less often, their stool in a controlled manner. One then speaks of urinary or fecal incontinence.
Urinary incontinence
Colloquially, this symptom is also called "bladder weakness". However, the blister is not always the cause. There are five different manifestations of urinary incontinence:
- Stress incontinence: Formerly known as stress incontinence because physical stress is the trigger: If the pressure in the abdomen increases (e.g. when lifting heavy objects, coughing, sneezing, laughing), those affected involuntarily lose urine. In severe cases, urine leaks with every movement, in extreme cases even when standing or lying down. Those affected do not feel the urge to urinate before the urine starts to leak out unintentionally.
- Urge incontinence: With this form of incontinence, the urge to urinate occurs very frequently (sometimes several times an hour) even though the bladder is not yet full. Often those affected do not make it to the toilet in time. The urine comes off like a gush.
- Reflex incontinence: People with reflex incontinence no longer feel when the bladder is full and can no longer control emptying. The bladder empties itself at irregular intervals, but often not completely.
- Overflow incontinence: When the bladder is full, small amounts of urine continually leak. Those affected may also feel a permanent need to urinate.
- Extraurethral urinary incontinence: Here too, urine is constantly leaking without the patient being able to control it. However, this does not happen through the urinary tract, but through other openings (medical: extraurethral), for example through the vagina or anus.

Stress incontinence affects women particularly often. In contrast, overflow incontinence is a typical consequence of prostate enlargement in men.
Some people also suffer from mixed incontinence. This is a combination of stress and urge incontinence.
Fecal incontinence
This form of incontinence is less common. Patients with fecal incontinence cannot arbitrarily hold back the intestinal contents and intestinal gases in the rectum. Doctors differentiate between three degrees of severity:
- Partial incontinence 1st degree: uncontrolled loss of air and occasional stool smear during exercise.
- Second degree partial incontinence: Patients cannot hold intestinal gases and thin stools.
- Total incontinence: total loss of control over bowel evacuation, which is associated with constant stool smear. Patients also lose solid stools.
As with urinary incontinence, there are cases in which the person concerned feels that the stool is about to pass but does not make it to the toilet in time, and those in which the stool occurs unexpectedly (the person concerned does not feel anything in the anal area).
Incontinence: causes and possible diseases

In the case of urinary incontinence, the finely coordinated system of bladder muscle, sphincter muscle and pelvic floor muscles as well as the controlling nerves and centers in the brain and spinal cord no longer function properly. In fecal incontinence, the disorder affects the occlusive apparatus of the anus and the corresponding nerve structures. In both cases, there can be a variety of reasons for this:
Causes of Urinary Incontinence
The five forms of urinary incontinence have very different causes, but all of them impair the function of the urinary bladder.
This fulfills two important tasks: it has to store the urine and empty itself (if possible) at the desired time. When storing, the bladder muscle is relaxed. This allows the bladder to expand and fill. At the same time, the sphincter muscle is tense, so that the urine cannot flow straight away through the urethra. To empty, the bladder muscle contracts, while the sphincter muscle relaxes with the pelvic floor muscles. The urine can then drain through the urethra.
Stress incontinence:
In stress incontinence, the locking mechanism between the bladder neck and the urethra is no longer functional. The reason could be that the pelvic floor tissue was injured, for example during prostate surgery or an accident. Nerve injuries and irritations as well as bulging of the urinary bladder can trigger stress incontinence. It is also favored by risk factors such as:
- chronic cough
- Obesity
- frequent lifting of heavy loads
- Lack of exercise (poorly trained pelvic floor!)
- (in women) sinking pelvic organs (such as lowering of the uterus)
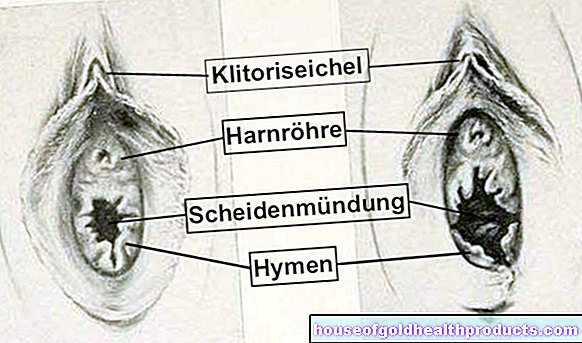
Stress incontinence is much more common in women than in men. This is because they have a wider pelvis and weaker pelvic floor muscles. There are also three openings in the female pelvic floor (for the urethra, vagina and rectum), while men only have two. These are "natural weak points". At these points, the connective tissue can give way due to stress such as pregnancy and childbirth, a lowering of the uterus or hormonal changes during the menopause - urinary incontinence occurs.
Urge incontinence:
With this form of incontinence, the signal "bladder full" is wrongly sent to the brain even if the bladder is not full. The response is an uncontrollable urge to urinate. One also speaks of "overactive bladder". Possible causes of urge incontinence are:
- Nerve damage or irritation as a result of surgery
- neurological diseases such as multiple sclerosis, Parkinson's, Alzheimer's, a brain tumor or a stroke
- constant irritation of the bladder, for example from bladder stones or urinary tract infections (cystitis)
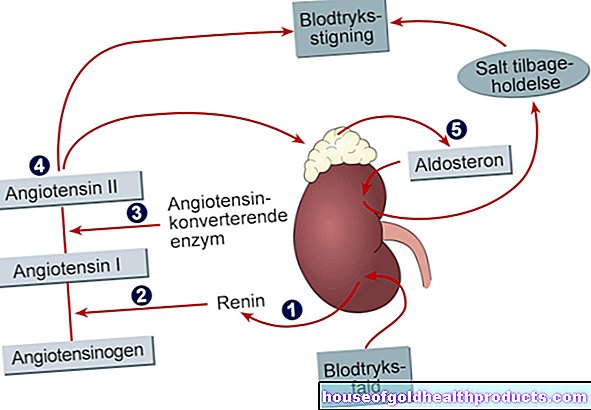
- Inadequately treated diabetes (diabetes mellitus): Toxins caused by high blood sugar levels affect the nervous system.
- psychological causes
Reflex incontinence:
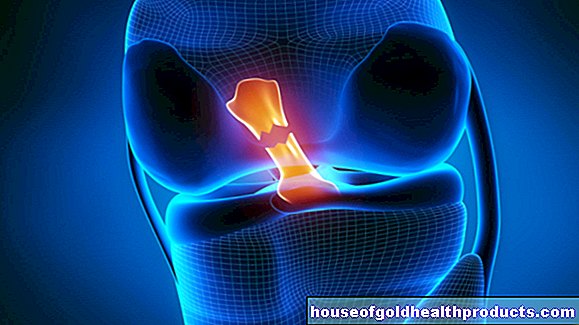
With reflex incontinence, nerves in the brain or spinal cord that control the bladder are damaged. This can be the case with paraplegia or neurological diseases such as Parkinson's, multiple sclerosis, stroke or Alzheimer's.
Overflow incontinence:
In this form, the outlet of the bladder is blocked and interferes with the flow of urine, for example through an enlarged prostate (as with benign prostate enlargement) or a narrowing of the urethra. The latter can be caused by a tumor or urinary stones.
Extraurethral incontinence:
This form of incontinence can be caused by congenital malformations or a fistula. In general, a fistula is understood to be an "unnatural" connecting tubule between two hollow organs or a hollow organ and the surface of the body. In the context of extraurethral incontinence, a fistula can exist between the urinary system (such as the bladder, urethra) and the skin, the intestine or the female genital tract. Accordingly, urine can leak through the skin opening, the anus or the vagina. Such a fistula can develop as a result of inflammatory processes or after an operation or X-ray irradiation.
Various medications (such as diuretics, antidepressants, neuroleptics) and alcohol can aggravate existing urinary incontinence.
Causes of fecal incontinence
Fecal incontinence is rarely congenital; it is then based on malformations, for example. The much more common acquired fecal incontinence is due to a disruption or damage to the so-called continence organ (anorectum). This consists of the rectum, in which the stool is “stored” (reservoir), and the sphincter muscle (sphincter) around the anal canal. Possible causes for a disorder or damage to the anorectum are:
- Injuries, for example caused by childbirth or operations: They can lead to a dysfunction of the sphincter muscle or impair the perception of nerves at the anus.
- inflammatory bowel diseases such as Crohn's disease
- neurological diseases such as dementia or multiple sclerosis
- Tumors in the rectum (such as rectal cancer)
- Sluggishness and constipation: Stuck stools cause a blockage that only watery stools can pass through.
- Pelvic floor weakness
- Medications such as laxatives, antidepressants, or Parkinson's medication
- pronounced hemorrhoids
- Prolapse of the rectum or rectum
Incontinence: Therapy
There are several ways to treat incontinence. In individual cases, the incontinence therapy is adapted to the form and cause of the incontinence as well as to the living situation of the patient.
Therapy of urinary incontinence
Pelvic floor training: In the case of stress urinary incontinence, good results can be achieved with pelvic floor training under the guidance of a physiotherapist. In doing so, the patient learns, for example, to reduce the stress on the pelvic floor in everyday life, to discard false tension patterns and to strengthen the pelvic floor with suitable exercises.
Biofeedback training: Some people find it difficult to feel the pelvic floor muscles and to consciously perceive and control the sphincter muscles. During biofeedback training, a small probe in the rectum or vagina measures contractions of the pelvic floor and triggers an optical or acoustic signal. During the pelvic floor exercises, the patient can see whether he is really tensing or relaxing the right muscles.
Electrotherapy: Here the pelvic floor muscles are passively trained using painless electrical impulses.
Toilet training (bladder training): Here the patient has to keep a micturition log for some time. In it, he enters when he felt the urge to urinate, when and how much urine he excreted and whether the urination was controlled or uncontrolled. The patient must also make a note of what and how much they drank in the course of a day or night. Based on these records, the doctor creates a drinking and micturition plan. This specifies how much the patient is allowed to drink and when to go to the toilet to empty the bladder (even without the urge to urinate). The aim is to prevent uncontrolled leakage of urine through regular emptying of the bladder.
Toilet training should only be done under medical supervision, even if the patient does the training himself at home.
Hormone treatment: In the event of incontinence due to estrogen deficiency during or after the menopause, the doctor can prescribe a local estrogen preparation (such as an ointment).
Medication: Depending on the type of incontinence, anticonvulsant medication (urge incontinence) or so-called alpha receptor blockers are suitable for treatment. The latter can loosen the bladder occlusion (overflow incontinence) or inhibit the spontaneous activity of the urinary bladder muscles (reflex incontinence).
Catheter: In the case of reflex incontinence, the bladder may have to be emptied regularly via a catheter.
Surgery: Extraurethral incontinence must always be treated surgically (e.g. by closing the fistula). If the incontinence is due to an enlarged prostate, an operation is also usually necessary. Otherwise, in the case of urinary incontinence, surgical intervention is only considered if non-operative therapeutic measures do not bring the desired success.
For example, the urethra can then be closed by an artificial sphincter or an adjustable loop. An implant that compresses the urethra to such an extent that the urine can no longer flow out involuntarily achieves a similar effect. In certain cases, the urethra is stabilized with collagen or silicone to alleviate the symptoms of incontinence. An implanted "bladder pacemaker" can help calm an overactive bladder or stimulate a bladder that can no longer empty on its own.
Therapy of fecal incontinence
Pelvic floor training, electrotherapy and toilet training are also effective therapy methods for faecal incontinence. Sometimes the patient is also implanted with a pacemaker that improves coordination between the brain, pelvic floor, intestine and sphincter muscles.
Further possible therapeutic approaches are:
- Laxatives: They specifically stimulate the elimination of stool.
- Motility inhibitors: These medicines stop bowel movements (peristalsis) and thereby reduce the frequency of bowel movements.
- Surgery: For example, injured sphincters can be sewn. If the large intestine has sunk due to a weak pelvic floor, the surgeon can fix it back to the sacrum. In some cases of fecal incontinence, an artificial sphincter is used.
Urinary Incontinence: Drink Correctly
Especially with urinary incontinence, drinking suddenly plays a decisive role for those affected: For fear of uncontrolled urination, they try to drink as little as possible. However, this does not improve the condition - on the contrary: if there is insufficient fluid intake, the urine in the bladder is more concentrated, which can increase the urge to urinate and irritate the mucous membrane of the bladder. In addition, the bladder, ureter and tube are poorly flushed out if you drink too little. This makes it easier for bacteria to attach themselves - a urinary tract infection results.
If you have urinary incontinence, you should therefore discuss with your doctor how much and at what times of the day you should drink. He may first ask you to keep a micturition log for a few days, in which you precisely record your fluid intake and urination (see above: toilet training). Based on these records, the doctor can recommend suitable amounts and times to drink.
Still water and herbal teas are best for incontinence. A special bladder tea can also help, for example with urge incontinence. Coffee, alcohol, and carbonated drinks are less good because they are diuretic.
Incontinence: Other Things You Can Do
Yes, incontinence means loss of control. But it doesn't mean that those affected are helpless. There are some things that everyone can do themselves to cope better with incontinence or to prevent incontinence:
Use incontinence aids: Templates in different suction strengths, disposable panties with included templates, incontinence briefs or anal tampons can help to deal with incontinence in everyday life. Men with urinary incontinence can use a condom urinal. This is a type of condom that drains urine into a bag.
Going to the toilet often enough: If you go to the toilet too often or too seldom, your bladder is not good and can significantly increase your risk of urinary incontinence. If you urinate too often, the bladder “gets used” to the small amounts of urine at some point and is then no longer able to store larger amounts of urine. If you go to the toilet very rarely, you constantly overstretch your bladder muscles and risk functional disorders.
Reducing weight: Obesity is an important risk factor for incontinence. It increases the pressure in the abdominal cavity and thus favors incontinence or exacerbates existing incontinence. So if you weigh too much, try to lose weight. This also has a positive effect on the success of the pelvic floor training.
Take care of the body: With careful body care you can prevent skin diseases as a result of bladder weakness.
Eating bladder-friendly food: Avoid foods that can irritate the bladder, such as hot spices or coffee. In the case of fecal incontinence, a high-fiber diet can normalize bowel movements. You should largely avoid flatulent foods.
Relaxation techniques: Relaxation exercises such as autogenic training can help if incontinence has emotional (co-) triggers.
Incontinence: medical examinations
Many people feel embarrassed when they can no longer hold their urine or stool properly. They endure their illness quietly and do not even dare to speak to their doctor about the subject. A mistake, because there are effective tools. In any case, those affected should be examined and treated by a doctor as soon as possible.
Medical history survey
In a conversation, the doctor first inquires about the exact complaints and the patient's history (anamnesis). In this way he can find out what type of incontinence someone is suffering from and narrow down the possible causes. Possible questions in the anamnesis interview are:
- How long have you had uncontrolled urine or stool leakage?
- How often do you pass urine / stool?
- Does it cause pain?
- On what occasions does involuntary urine or stool leakage occur?
- Do you feel like your bladder / bowel is not emptying completely?
- Can you feel whether your bladder / bowel is full or empty?
- Did you have an operation? Have you given birth to a child?
- Do you have any underlying illnesses (diabetes, multiple sclerosis, Parkinson's etc.)?
Investigations
Various examinations help to clarify incontinence. Which methods make sense in individual cases depend, among other things, on the type and severity of the incontinence. The most important investigations are:
- Examination of the external genitals and rectum: It provides clues about the causes of incontinence. This can sometimes help the doctor spot fistulas or an enlarged prostate. He can also check the tension of the sphincter muscles.
- Gynecological examination: For example, a lowering of the uterus or the vagina can be identified as the cause of urinary incontinence.
- Urine and blood tests: They may give evidence of infection or inflammation.
- Ultrasound examination: Ultrasound can be used to estimate the amount of urine remaining in the bladder in the event of urinary incontinence. Kidney or bladder stones, tumors or congenital malformations can also be detected. Injuries after an operation can also be detected in the ultrasound.
- Urodynamics: In the case of urinary incontinence, the doctor can use urodynamic examinations to assess the function of the urinary bladder. For example, as part of uroflowmetry, electrodes can be used to measure the amount of urine, the duration of bladder emptying and the activity of the pelvic floor and abdominal muscles while urinating.
- Bladder or colonoscopy: It may be necessary to uncover, for example, inflammation of the bladder or intestinal mucosa or tumors of the bladder or intestine.
- X-ray contrast images: They can provide information about a malfunction of the bladder or rectum. To do this, the bladder or rectum is first filled with a contrast medium. X-rays are then taken while urinating or defecating. In this way, functional processes can be analyzed and protuberances and indentations or internal incidents can be identified as the cause of incontinence.
Additional information
Guidelines:
- Guideline "Stress Incontinence of Women" of the German Society for Gynecology and Obstetrics
- Guideline "Urinary Incontinence in Geriatric Patients, Diagnostics and Therapy" of the German Society for Geriatrics
Self-help groups:
- Incontinence Self-Help e.V .: https://www.inkontinenz-selbsthilfe.com/
- Self-help association incontinence e.V .: https://www.selbsthilfeverband-inkontinenz.org/